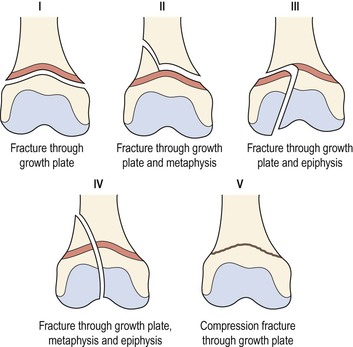
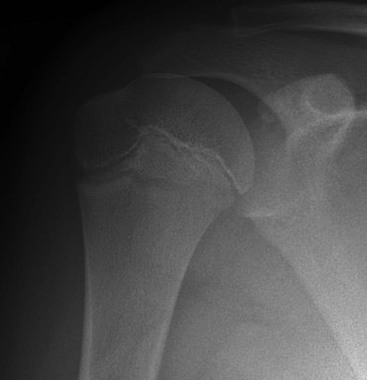
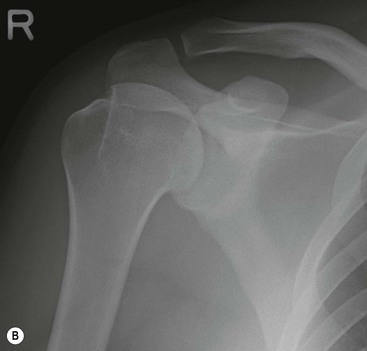
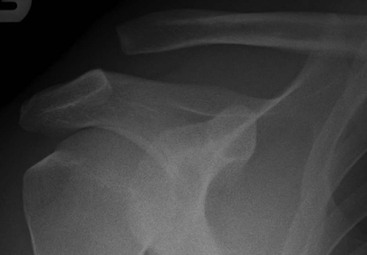
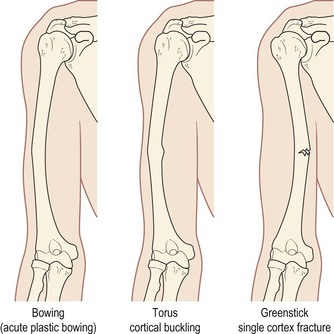
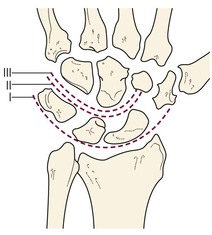
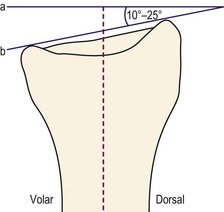
Nigel Raby, Philip M. Hughes, James Ricketts This chapter will consider skeletal trauma and its consequences. It will be largely confined to appearances on radiographs occasionally supplemented by CT. The soft-tissue aspects of trauma principally imaged with MRI will not be considered in this chapter. In evaluating any bony injury due to trauma it is essential that two radiographs are obtained, usually at right angles to each other (orthogonal). Many fractures are visible on only one of these radiographs. Inexperienced observers will tend to rely on the anteroposterior (AP) view as this is better understood intuitively. The lateral view, however, will identify at least as many fractures as the AP and may be the only view where the fracture is visible. Time spent becoming familiar with the lateral view will be well rewarded. The old adage ‘One view is no view’ is particularly relevant when assessing trauma radiographs. Fractures of bones can be considered to be incomplete or complete. Incomplete fractures are generally confined to injuries in children (Fig. 52-1). There are three types: 1. Plastic bowing injury where the bone is mildly deformed but there is no disruption of the cortex. Also seen only in children are fractures related to the epiphyseal growth plate. These have been classified by Salter and Harris into five types (Fig. 52-2). Complete fractures refer to a fracture which separates one part of bone from the other. The fracture pattern should be described. These fractures can be subdivided by the fracture direction into transverse, oblique, spiral and longitudinal. The presence or absence of angulation, rotation, distraction or shortening with overlap should be stated. The site of the fracture within the bone should be stated. If near a joint, note should be made as to whether the fracture extends to involve the articular surface. This is an important observation as, in general, intra-articular fractures have a poorer prognosis and surgical intervention is more often required. The term ‘comminuted’ refers to fractures which have more than two parts of bone at the fracture site, although by convention small bone fragments are often disregarded. A large triangular bone segment is referred to as a butterfly fragment and a segmental fragment is seen when there is a separate segment of bone between the main fracture components. A compound fracture is one where there is breach of the overlying soft tissue and skin. Although this can sometimes be identified on radiographs it is usually a clinical diagnosis. It is generally understood that a fracture results in a gap between the bone ends through which the X-ray beam can pass, resulting in a dark or black line on the radiograph. Not so well appreciated is that the presence of a white or sclerotic area of bone is an equally important sign of fracture. In the setting of trauma this finding is due to either impaction or overlap of bone. Both will result in increased bony density. The best-known example of this is an impacted fracture of the femoral neck. However, there are many other situations and sites where this can occur. It is a very useful radiological sign which can help detect subtle fractures. Its value will be demonstrated several times in this chapter. An avulsion fracture occurs at sites of tendon or ligament attachment when a fragment of bone is pulled off the underlying parent bone as a result of traction from either the muscle tendon kinetic chain or a joint ligament. To describe any injury as an avulsion fracture you must be able to identify the mechanism of injury and state what ligament or tendon attaches to the bone fragment. These should not be referred to as flake or chip fractures unless there is a clear mechanism of a direct impact to the area which would account for the findings; such fractures are rare. Understanding of the above will lead to an appreciation of the severity and significance of the findings. A bone avulsion at the site of tendon attachment occurs due to muscle contraction and will usually be a single-site abnormality (e.g. avulsion of fifth metatarsal base). Ligaments, on the other hand, have no contractile capacity and serve to stabilise joints. For a ligament to avulse a bone fragment there must have been a major distraction or angulation of the joint. This is therefore often associated with other injuries (see discussion of Segond fracture in the section ‘The Knee’). A knowledge of major tendon and ligament attachments is essential for correct interpretation of these injuries. The more common examples of this will be described throughout the chapter. Stress fractures occur when normal bone is subjected to repeated abnormal loading such that microfracturing occurs. Repetition of this loading over a period of time at a rate which exceeds the capacity of reparative processes results in progressive weakening of the bone to the point where a true fracture can occur at the site of stress. A lucent fracture line is, however, often not evident in the early stages of the process. A periosteal reaction and medullary sclerosis may develop at the site of stress and may be the only abnormality on the radiographs. If abnormal loading is continued, a frank fracture will eventually occur. (See examples in the sections ‘The Ankle’ and ‘Foot Injuries’.) A pathological fracture occurs through an area of abnormally weak bone. The term is usually reserved for fractures occurring at the site of bone involvement by tumour. This may be either primary benign or malignant lesions or secondary malignant deposits. Most commonly pathological fractures occur through the site of a metastatic deposit, including myeloma. Pathological fractures can also occur in weak bone, resulting from osteporosis or metabolic bone disease; these fractures are sometimes referred to as insufficiency fractures. Dislocation refers to the situation at a joint where the articular surfaces have lost all contact. They may be associated with fractures in addition. Subluxation occurs when the joint surfaces are no longer fully congruous but some articular surface contact is maintained. The shoulder consists of two separate joints: the gleno-humeral and the acromio-clavicular (AC) joint. It is essential that both are carefully evaluated in every patient. Standard views of the shoulder include an AP radiograph in all cases. A second view is essential but as none are ideal there are local variations. There are three possible additional views: axial, axial oblique and lateral. The authors favour the axial oblique as the patient does not have to move the injured shoulder and it is relatively easy to interpret. Its weakness is that it does not provide a second view of the scapula. A true lateral view can be obtained if a scapular fracture is suspected clinically. On the AP view it is important to appreciate that the humeral head is an asymmetric structure with more bone lying medial than laterally. The humeral head should be congruent with the glenoid fossa. In the adolescent shoulder the appearance of the unfused epiphysis should not be mistaken for a fracture (Fig. 52-3). Anterior dislocation is common, accounting for 95% of all dislocations1 and diagnosis is usually obvious (Fig. 52-4). The humeral head is no longer congruous with the glenoid and is displaced lying in a subcoracoid position. Anterior dislocations are often associated with fractures, of which there are three types: 1. A fracture of the greater tuberosity sheared off or avulsed as the humerus dislocates (15%) (Fig. 52-5). 2. Fracture of the anteroinferior corner of the glenoid (8%) known as a Bankart lesion (Fig. 52-6). These fractures may be subtle and CT can be used in such cases to clarify the site and extent of the fracture. 3. A V-shaped deformity of the humeral head caused by the impaction of the anterior glenoid rim on the posterosuperior humeral head. This is known as a Hill–Sachs lesion.2 Once the humeral head is relocated, the signs of a Hill–Sachs lesion are a notch in the superolateral humeral head and a sclerotic vertical line of impacted bone (Fig. 52-7). Careful search should be made for these fractures in all cases of anterior dislocation. Posterior dislocation is rare1 (<5%). The congruity of the humeral head with the glenoid often appears to be maintained on the AP view. The key observation on the AP view is that the normal asymmetrical appearance of the head is replaced by a much more spherical symmetrical appearance referred to as the ‘light bulb’ sign. Careful scrutiny of the second view is needed to confirm the loss of contact between the humeral head and the glenoid (Fig. 52-8). In many instances the humeral head appears symmetrical but is not dislocated. This is due to the arm being held in internal rotation such as when the arm is in a sling. Thus the second view must be used to determine whether the humeral head is in joint. Fractures of the humeral head and proximal shaft typically occur following a fall on the outstretched arm. The humeral head is driven into the hard cortical bone of the glenoid. This results in several fracture patterns. Fractures may involve the surgical neck and the greater and lesser tuberosities. This can result in up to four major bone fragments. Comminuted fractures of the humeral head have been classified by Neer depending on the number of major fracture fragments from 1 to 4.3 In this classification, to qualify as separate bone fragments they must be displaced by 1 cm or angled at 45° or more to the adjacent bone. Based on the above, a multiple part fracture of the humeral head which is undisplaced is classified as a Neer ‘1 part’ fracture.This pattern accounts for the great majority (85%) of such fractures which if they are minimally displaced are not considered as separate fragments. Two-, three- and four-part fractures are seen with fractures involving, respectively, the greater and lesser tuberosities in addition to the surgical neck. Any combination of injuries may occur. Isolated fractures of greater or lesser tuberosity are most often avulsion injuries due, respectively, to the pull of supraspinatous and subscapularis muscles and are comparatively rare outside of the setting of dislocation described above. Transverse fractures of the humerus involve either the surgical neck or the shaft inferior to this. Medial displacement of the humeral shaft occurs due to pull of pectoralis major muscle. Clavicle fractures are very common; as the bone is just under the skin surface, they are easy to detect clinically. Fractures most often involve the middle third (80%). Outer-third fractures occur in 15% of cases. Medial-third fractures are uncommon, accounting for only 5% of cases.4 The AC joint is held in place by the acromio-clavicular ligament and the two coraco-clavicular (CC) components known as conoid and trapezoid ligaments. Minor disruptions are best detected by looking at the inferior cortex of both the clavicle and the acromion. These should align. If they do not, then there is an AC joint subluxation. The normal distance between the superior surface of the coracoid and the inferior clavicle is no more than 13 mm. Disruptions are graded from 1 to 3.5 Grade 1 is sprain of the ligaments only. There is only minor separation, if any, at the AC joint. In grade 2 injuries the AC joint ligaments are torn but the CC ligaments are intact. In a grade 3 the CC ligaments are disrupted. As a result the coraco-clavicular distance may exceed 13 mm (Fig. 52-9). Surgical stabilisation will be required. Detecting the difference between a grade 2 and grade 3 injury may be facilitated if the affected limb is made to weight bear using weights strapped to the wrist to distract the AC joint. More recently direct visualisation of the ligaments by MRI has been suggested.6 There are no variations in the standard views of the elbow which are the AP and lateral. A useful soft-tissue sign in the elbow is the fat pad sign.7 The normal elbow has small pads of fat closely applied to the distal humerus both anteriorly and posteriorly. These are not normally visible as they lie within the bony fossae of the distal humerus. However, if there is a joint effusion such as may occur following trauma the fluid displaces the fat pads away from the humerus and out of the fossae. These fat pads can then be identified on a lateral radiograph as lucent areas. The anterior fat pad may just be visible normally but if displaced away from the humerus is abnormal. A visible posterior fat pad is always abnormal. The presence of displaced fat pads indicates an effusion8 and if a fracture is not readily identified further careful inspection of the radiograph is needed to exclude a more subtle fracture which may have been overlooked (Fig. 52-10). In children, a supracondylar fracture is the commonest lesion to be overlooked; in adults, a radial head fracture. Note, however, that the absence of the fat pad sign does not exclude a fracture and effusions are not always caused by trauma. Supracondylar fractures are the commonest injury around the elbow in children.9 Some fractures are grossly displaced with the distal bone fragment displaced posteriorly.The anteriorly displaced humeral shaft often has sharp bone edges which puts the adjacent brachial artery as well as the median and ulnar nerves in jeopardy. However, in 50% they are subtle greenstick-type injuries (Fig. 52-11). Detection of subtle injuries can be facilitated by using the anterior humeral line.10 On a lateral radiograph a line drawn down the anterior humeral cortex will pass through the capitellum such that at least one-third of the capitellum lies anterior to the line. If this rule is broken then it is very likely that there is a subtle greenstick or Salter–Harris growth plate injury of the distal humeral, allowing the distal humerus with the attached capitellum to be displaced posteriorly.11 The second commonest elbow injury in children is of the lateral condyle.12 Recognition of these injuries is made difficult by the presence of developing ossification centres in the immature skeleton. There are four in the distal humerus and one each in the radius and ulna. The order of appearance with few exceptions is capitellum, radius, internal epicondyle, trochlea, olecranon, lateral epicondyle—remembered by the mnemonic CRITOL13 from the first letter of each epiphysis. Knowedge of this order makes it possible to determine whether a bone fragment adjacent to the humerus is a normal ossification centre or represents a fracture. As the lateral epicondyle is the last ossification centre to appear, then if there is a bone fragment adjacent to the lateral aspect of the distal humerus look for the other ossification centres. If it is not possible to identify the five other centres, then the area in question must represent a fracture (Fig. 52-12). It should be noted that although there may only be a small bony component to this injury there will be a large fracture through the growing cartilaginous distal humerus.14 Dislocation of the radial head occurs in both children and adults. It may be difficult to appreciate on the AP radiograph but easier on the lateral. A helpful method of detecting these injuries is use of the radio-capitellar line. This line is drawn along the mid shaft of the radius proximal to the tuberosity. It should pass through the capitellum on every view; if not, the radial head is dislocated (Fig. 52-13). This rule is true also in children, although care is needed in the very young when the capitellum is small.15 There is a fracture association which must be recognised. The bones of the forearm are bound strongly at either end by strong ligaments. It is difficult to fracture one of these bones without the other, so fractures of radius and ulna occur commonly together. However, if only one bone appears fractured and, especially if the fracture is angled or overlapped, a covert injury of the other bone is very likely. This typically takes the form of a dislocation of the non-fractured bone. Thus a fracture of the ulnar shaft is often associated with a dislocation of the radial head at the elbow. This is known as a Monteggia fracture dislocation16,17 (Fig. 52-14). Conversely a radial shaft fracture is associated with a dislocation of the ulna at the wrist. This is known as a Galeazzi fracture dislocation. Fractures of the distal humerus in adults rarely cause diagnostic problems. Most fractures are readily apparent. Typically they involve the distal humeral condyles often with inta-articular extension into the elbow joint. Capitellar fractures are uncommon and may be difficult to see on the AP radiograph. The lateral view, however, provides the diagnosis. The displaced capitellum has an appearance like a half moon and is seen lying antero-superior to the forearm bones. Radial head fractures18 may involve the radial neck only or may be intra-articular, with disruption of the radial articular surface. The fat pad sign described above is useful in drawing attention to the radial head as a possible site for subtle radial head fracture. The commonest ulnar fracture is of the olecranon.19 The fracture involves the articular surface with the proximal fracture fragment often displaced due to the unopposed pull of the triceps muscle. Standard views for evaluation of the wrist are a posteroantererior (PA) and lateral radiographs. Additional views are required when there is clinical suspicion of a scaphoid fracture. On an AP radiograph look for the normal uniform spacing of 1–2 mm around each carpal bone and at the carpometacarpal junction. Loss of this spacing should lead to very careful inspection of the abnormal area, as often this will indicate significant carpal or carpometacarpal disruption. One should also observe the arrangement of the carpal bones into three smooth arcs. The first delineates the proximal surface of the proximal row of carpal bones (scaphoid, lunate, triquetral). The second is formed by the distal articular surface of the same bones. The third is along the proximal curvature of the capitate and hamate.20 These arcs should normally be smooth with no steps or interruption (Fig. 52-15). On a lateral radiograph the normal distal radius has a volar tilt of approx 10°. This represents the angle between a line drawn along the long axis of the radius and a line drawn from the dorsal to the volar rim of the radius and has a normal range of 2–20° (Fig. 52-16). Alteration of this angle occurs when there is a subtle fracture of the distal radius. Normal relationship of the distal radius and carpal bones is best assessed on the lateral view and this is discussed further in the section on carpal injuries. Displacement of the distal radial epiphysis and disruption of carpal alignment are often only evident on this view. Fractures of the triquetral will usually only be seen on the lateral radiograph. From the above it can be seen that the lateral radiograph is of critical importance in assessing wrist injuries. Most commonly, injuries result from a fall on the outstretched wrist. The type of injury sustained is age related. In young children fractures of the radius proximal to the epiphyseal plate predominate in age group 6–10. These fractures often involve both radius and ulna and may be grossly displaced. After this, until epiphyseal fusion, injuries most commonly involve the epiphyseal plate and are thus Salter–Harris fractures.9 Typically there is dorsal displacement of the epiphysis with or without an associated fracture fragment from the adjacent metaphysis, resulting in either a Salter–Harris type 1 or 2 injury (Fig. 52-17). Greenstick and buckle or torus fractures of the radius occur only in children (Fig. 52-18). Distal radial fracture (Fig. 52-19) is the commonest wrist injury in patients over age of 40.21 Increasing frequency with age suggests a relationship to osteoporosis. The definition of a Colles’ fracture includes the following: (1) fracture of radius within 2 cm of distal radial articular surface but not involving it; (2) dorsal angulation or displacement of distal fragment; and (3) associated fracture of ulnar styloid process. Smith described a variation of the above where the distal radial fragment is displaced and angled volarly and medially. In both of these injuries the articular surface remains intact (Fig. 52-20). Barton’s fracture differs from the above due to involvement of the articular surface of the radius. It is a shearing injury through the articular surface.The term is now often incorrectly ascribed to any intra-articular fracture. Subtle radial fractures may be detected by observing a minor disruption of the dorsal radius cortex on the lateral radiograph and alteration in the radial angle from the usual 10° volar (Fig. 52-21). Isolated fracture of the radial styloid process, also known as Hutchinson’s or chauffeur’s fracture, refers to an intra-articular fracture which runs obliquely across the distal radius from the radial cortex into the joint separating the radial styloid from the parent bone. Many fractures do not conform exactly with the original descriptions, with combination injuries common. For this reason, rather than using the eponymous names it is better to give a full description of the fracture lines, fragment displacement and angulation and extent of articular involvement. The scaphoid accounts for at least 60% of all carpal fractures.21 Typically, when scaphoid injury is suspected, one or two additional radiographic projections are employed with the intention of elongating the scaphoid, projecting it clear of other carpal bones and allowing the X-ray beam to pass through the scaphoid perpendicular to its long axis. The projections used vary but in the authors’ department a second PA view with ulnar deviation plus one with the tube angled at 45° toward the elbow is obtained. The blood supply of the scaphoid is unusual, with arteries entering distally then passing proximally to supply the rest of the scaphoid. When a fracture occurs through the waist (middle third) of the scaphoid, which is the commonest site (80% of cases), the blood supply to the proximal pole is interrupted. This results in significant risk of avascular necrosis of the proximal pole or non-union of the fracture (Fig. 52-22). Contrary to common belief, the great majority of fractures are visible on initial radiographs.22 Nevertheless there are a small number not identified. Accordingly, because of the risk of avascular necrosis and non-union, the patient is managed as if a fracture is present and the wrist is immobilised. The patient is then reviewed at about 10 days when further radiographs are obtained23,24 in the belief that resorption will occur around a fracture site rendering it visible on delayed radiographs, although this is now questioned. Alternative imaging techniques are now increasingly utilised. Skeletal scintigraphy is sensitive but non-specific. MRI is now the investigation of choice and there is good evidence that this should be undertaken soon after the initial injury25 (Fig. 52-23). After the scaphoid the triquetral is the most commonly injured carpal bone, accounting for 18–20% of injuries26 (Table 52-1). Typically the fracture is not evident on the PA view but can be seen on the lateral as a bone fragment seen on the dorsal aspect of the wrist (Fig. 52-24). Other carpal bone injuries are all relatively rare, each of the other carpal bone accounting for only 2–3% of injuries. CT or MR has a useful role to play in these injuries, which are often difficult to detect on plain radiography. TABLE 52-1 Relative Incidence of Carpal Bone Fractures Most carpal fractures and dislocations are caused by falling on the outstretched wrist with the wrist forced into an hyperextended position. Carpal dislocations most commonly involve the lunate.27 On a PA radiograph the lunate normally has a trapezoid appearance. When it is dislocated, it assumes a triangular shape. There is disruption of the normal carpal arcs and the intercarpal spaces are lost (Fig. 52-25). It is on the lateral radiograph, however, where the diagnosis is most easily made.28 On a normal lateral view of the wrist a vertical line drawn through the centre of the lunate should inferiorly pass through the radial articular surface and superiorly should pass through the centre of the capitate (Fig. 52-26). If this rule is broken, a carpal dislocation is certain (Fig. 52-27). Lunate dislocation is most commonly an isolated finding. The lunate will be seen displaced volar to the line. Perilunate dislocation is more common and is often associated with other carpal injuries, most commonly a fracture of the scaphoid. In this injury the lunate remains aligned with the radius but the capitate and the rest of the distal carpal row are displaced in a volar direction (Fig. 52-28).
Appendicular and Pelvic Trauma
General Considerations
Describing Fracture Types
The Shoulder
The Acromio-Clavicular Joint
The Elbow
Children
Adults
The Wrist
Radius and Ulna
Children
Adults
Carpal Injuries
Scaphoid
68.2%
Triquetrum
18.3%
Trapezium
4.3%
Lunate
3.9%
Capitate
1.9%
Hamate
1.7%
Pisiform
1.3%
Trapezoid
0.4%
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Appendicular and Pelvic Trauma
Chapter 52