CHAPTER 4 Applied anatomy and physiology of the gastrointestinal tract (GIT)
Overview
The gastrointestinal (GI) tract, also known as the alimentary canal, commences at the buccal cavity of the mouth and terminates at the anus. It can be divided into an upper GI tract (consisting of mouth, pharynx, esophagus and stomach) and a lower GI tract (small and large intestines). The three primary functions of the GI tract are the ingestion of food and water, the digestion of food and absorption of nutrients and the expulsion of waste matter. These primary functions are carried out in conjunction with the accessory digestive organs such as the salivary glands, pancreas, liver and gall bladder. Further detailed exploration of the accessory abdominal organs is outside the remit of this book, but suitable references are suggested at the end of the chapter.
Embryology of the GI tract
As the newly implanted embryo reaches the fourth week of gestation it begins to fold ventrally (anteriorly) in two directions. The head and tail end of the embryo curl towards each other and the sides of the embryo begin to fold ventrally towards each other. A constriction results between the embryo and the greater part of the yolk sac, trapping a small part of the yolk sac within the embryo (Figure 4.1A). The constriction corresponds to the future umbilicus. The trapped part of the yolk sac becomes the primitive digestive tube (Lewis, 2000).
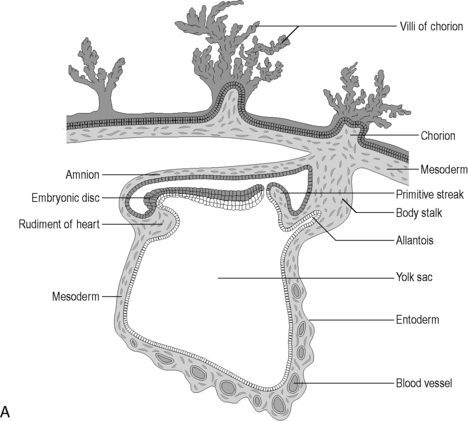
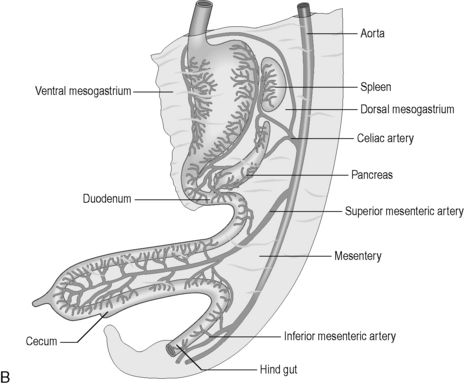
Figure 4.1 (A) The development of the primitive digestive tube. The embryonic disk curves ventrally trapping some of the yolk sac within it. This forms the primitive digestive tube. (B) The embryological gut and its blood supply.
(From an original drawing in Gray’s Anatomy).
Further anterior growth of the cranial end of the embryo results in folding of the buccopharyngeal membrane and this causes a diverticulum of the digestive yolk sac to form – this becomes the foregut. Another diverticulum also extends from the caudal end, becoming the hindgut. The remaining primitive digestive tube is known as the midgut. For the first four weeks of gestation, a wide communication exists between the digestive tube and the main yolk sac, but this gradually narrows to form the vitelline duct. This usually regresses but, where it remains after birth, it is known as a Meckel’s diverticulum, found in approx 2% of individuals (Lewis, 2000). The diverticulum is a 5 cm long blind-ended pouch projecting from the ileum in the affected adult, approximately 1 metre from the ileocecal valve (Lewis, 2000).
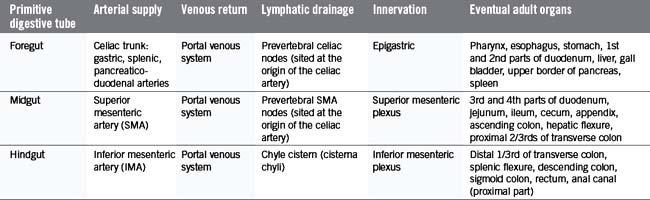
The primitive gut is well vascularized, receiving blood from the aorta via the celiac trunk (foregut), the superior mesenteric artery (midgut) and the inferior mesenteric artery (hindgut) (Figure 4.1B).
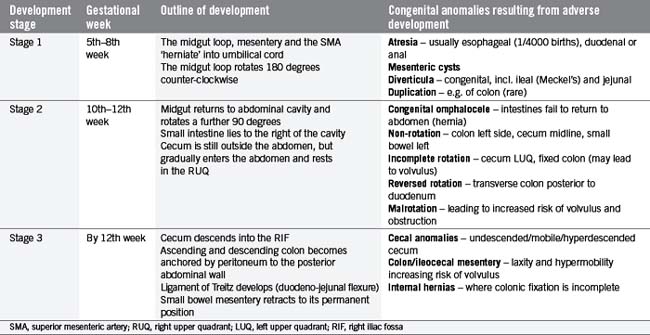
In the fifth gestational week, the primitive gut grows rapidly and reorganizes into the permanent GI tract structures (Table 4.1). This progression is traditionally divided into three stages:
Table 4.2 outlines the three stages and considers some congenital anomalies that can be seen as a result of developmental problems during these three stages. In particular, midgut rotational abnormalities are relatively common and can be seen in Figure 4.2.
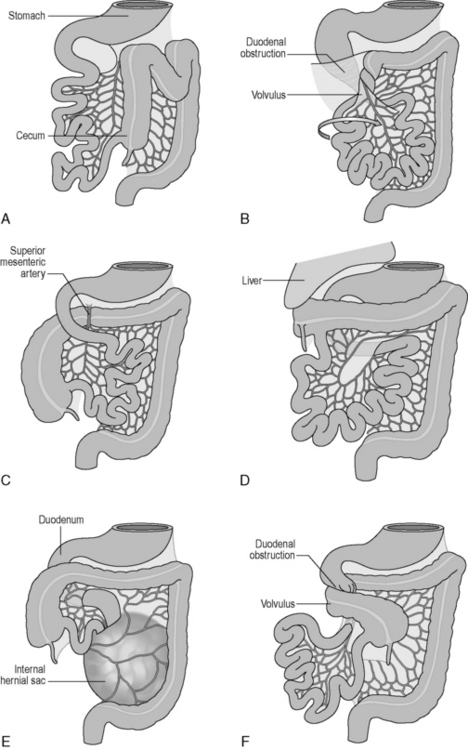
Figure 4.2 Abnormalities of midgut rotation. (A) Nonrotation; (B) Mixed rotation and volvulus (twisting) of the intestines; (C) Reversed rotation; (D) Subhepatic cecum; (E) Paraduodenal hernia; (F) Midgut volvulus.
(Reproduced from Moore KL and Persaud TVN, Before we are Born: Essentials of Embryology and Birth Defects, 7th edn. Saunders, Philadelphia, 2007.)
Histology of the GI tract
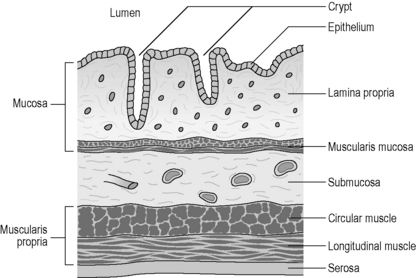
The GI tract displays a uniform histology throughout its length, with subtle differences between regions corresponding to functional specialization. The GI tract is divided into four concentric layers surrounding the lumen as shown in Figure 4.3 (mucosa, submucosa, muscularis externa and serosa or adventitia).
The innermost layer is known as the mucosa, which surrounds the lumen of the GI tract. It has both a protective function (from injury and infection), as well as a digestive function (chemical breakdown, absorption and secretion). The mucosa can be further subdivided into three layers. The epithelium is the innermost layer, in contact with the ingested material. It is supported structurally and nutritionally by the lamina propria, a layer of loose irregular connective tissue, well supplied by blood capillaries and lymphatic tissue. The outermost subdivision of the mucosa is a thin layer of smooth muscle known as the muscularis mucosae. This smooth muscle throws the mucosa into small folds, increasing the absorptive surface area and encouraging the turbulence of the fluid contents (chyme). The mucosal layer is highly specialized within each organ of the GI tract, reflecting the different functions and chemical environments (Table 4.3).
Table 4.3 Mucosal differentiation throughout the GI tract
The muscularis propria (externa) generally consists of two smooth muscle layers; however, in the esophagus, striated (skeletal) muscle replaces the smooth muscle in the proximal third. Throughout the rest of the GI tract, the inner circular muscle layer has smooth muscle fibers lying in a concentric fashion around the circumference of the GI tract, while the outer longitudinal muscle layer has fibers orientated parallel to the direction of the GI tract. (Note that in the stomach there is also an additional innermost oblique layer of muscle fibers, mainly limited to the cardiac end of the stomach). In between the two layers lies a second enteric nerve plexus, known as the myenteric (or Auerbach’s) plexus. This plexus is responsible for coordinating motility (movement) of the GI tract, including peristalsis, whereby coordinated contractions of the two muscle layers assist in propelling the food bolus along the lumen.
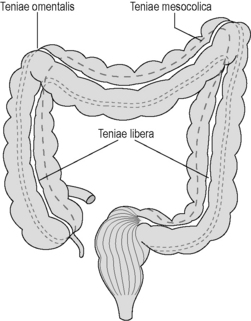
In the colon, the longitudinal muscle layer is incomplete, being gathered into three 1 cm thick bands called the teniae coli, with only a thin layer of muscle in between. These bands (the teniae omentalis, libera and mesocolica) converge on the base of the appendix, run the full length of the colon, fanning out into a continuous layer surrounding the rectum (Figure 4.4). Contraction of the teniae coli gathers up the colon in a concertina effect, the resulting sacculations being known as haustral pouches or haustrations. These are clearly defined and fixed in the proximal colon, but require active contraction in the distal colon, where the teniae are thinner (see Chapter 16).
Oral cavity
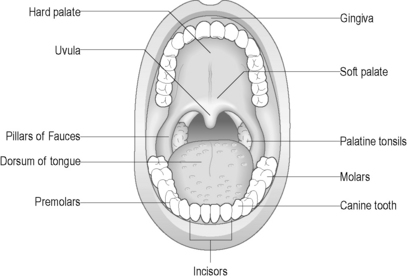
The oral cavity (mouth) is designed to support chewing, swallowing and speech. Two rows of teeth are embedded within the maxilla above and the mandible below and are surrounded by the gums (gingivae). The functions of the mouth are also facilitated by the hard and soft palate above, the floor of the mouth below, the cheeks laterally, the tongue, and the upper and lower lips externally (Figure 4.5). Two separate sets of teeth are grown in humans: the primary dentition (deciduous teeth) develops during early childhood and consists of 20 teeth. The secondary dentition (permanent teeth) gradually replaces the deciduous set with 32 adult teeth. These teeth are adapted for different functions, including cutting (incisors), tearing (canines), crushing (premolars) and grinding (molars).
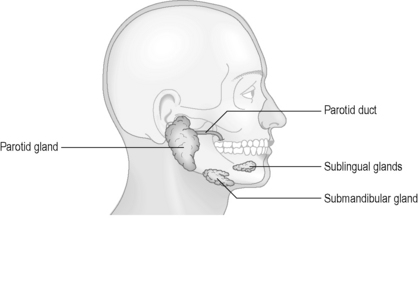
Several other openings within the oral cavity are associated with the salivary ducts. Three pairs of salivary glands secrete saliva into the oral cavity in response to food stimuli (Figure 4.6). Saliva is composed of primarily water (approximately 98%), in combination with ions, salivary amylase (which begins the breakdown of starch to sugars), lysozymes (antibacterial), as well as trace quantities of urea (a waste product). The saliva lubricates the food and helps to form it into a bolus suitable for swallowing.
The pharynx
The pharynx is a complex anatomical structure serving as a gateway to both the digestive and respiratory passageways. During respiration, the pharynx provides a patent airway from the nose and mouth through to the larynx. During swallowing (deglutition) it provides a passageway from the mouth to the esophagus, while ensuring that the bolus cannot enter the airway. The pharynx also has important functions in relation to speech, choking, vomiting and yawning (Rubesin, 1999).
The pharynx lies posteriorly to the nasal cavities, the oral cavity and the larynx. Laterally lie the muscles of the neck, the lateral portions of the hyoid bone and thyroid cartilage and the carotid sheath (Rubesin, 2000).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree