Presentation and Presenting Images
( ▶ Fig. 102.1, ▶ Fig. 102.2, ▶ Fig. 102.3, ▶ Fig. 102.4, ▶ Fig. 102.5, ▶ Fig. 102.6)
A 65-year-old female presents with a palpable mass in the right breast that was diagnosed as a grade 2 invasive lobular carcinoma (ILC) with axillary metastases. The imaging presented is of her left breast at the time of her right breast cancer diagnosis.
102.2 Key Images
( ▶ Fig. 102.7, ▶ Fig. 102.8, ▶ Fig. 102.9, ▶ Fig. 102.10, ▶ Fig. 102.11)
102.2.1 Breast Tissue Density
There are scattered areas of fibroglandular density.
102.2.2 Imaging Findings
The right breast has an ill-defined mass that has resulted in an increase in breast density and overall shrinkage of the breast (not shown). The ultrasound-guided biopsies of the right breast revealed invasive lobular carcinoma and metastases to the ipsilateral level I lymph nodes. The left breast mammogram when the patient initially presented had a vague asymmetry ( ▶ Fig. 102.7) and possible calcifications at the 12 o’clock location in the posterior depth. Craniocaudal (CC) and mediolateral (ML) spot-magnification images ( ▶ Fig. 102.8 and ▶ Fig. 102.9) were obtained that demonstrated architectural distortion. Due to the complexity of the findings, full CC and ML digital breast tomosynthesis (DBT) images of the left breast were obtained, which demonstrated the architectural distortion in the posterior depth at 12 o’clock ( ▶ Fig. 102.10 and ▶ Fig. 102.11). An ultrasound was performed and a correlating lesion was not identified. Because this lesion was best seen on tomosynthesis, it was recommended that the patient undergo tomosynthesis-guided biopsy.
102.3 BI-RADS Classification and Action
Category 4C: High suspicion for malignancy
102.3.1 Tomosynthesis Biopsy Images
( ▶ Fig. 102.12, ▶ Fig. 102.13, ▶ Fig. 102.14, ▶ Fig. 102.15)
102.3.2 Imaging Findings
Due to the 12 o’clock location of the lesion, a CC approach was first tried. The lesion was not as well seen, and thus the lesion was approached from the lateromedial (LM) approach. Tomosynthesis movies were obtained in the prefire and postfire needle positions. No stereo pair images were obtained. The needle can be seen in good position for the biopsy ( ▶ Fig. 102.12) and the clip is placed at the completion of the biopsy ( ▶ Fig. 102.13). The postprocedure mammogram demonstrates the biopsy marking clip in the location of the mammographic finding ( ▶ Fig. 102.14 and ▶ Fig. 102.15).
102.4 Differential Diagnosis
Breast cancer (invasive ductal carcinoma [IDC]): The patient has advanced ILC of the contralateral breast. This lesion, although unexpected, is very suspicious. The biopsy results yielded grade 1 invasive ductal carcinoma.
Radial scar: The patient’s last mammograms were many years ago and so it was difficult to make an adequate comparison with them. Radial scars are often best seen on one view. This would have been considered a concordant diagnosis for this architectural distortion.
Sclerosing adenosis (SA): Sclerosing adenosis can present as a mass, calcifications, and architectural distortion when it has a larger component of fibrosis. This would be considered concordant if the size of the imaging lesion matched the size of the histopathologic lesion. If only small fragments of histopathologic lesion were identified as SA, then this diagnosis would be considered discordant and excision would be recommended.
102.5 Essential Facts
Satisfaction of search is always a problem when viewing imaging studies. It is especially important to evaluate the entire breast and the contralateral breast completely when faced with an obvious finding. Had the evaluation been halted too early, the contralateral cancer (presented here) would have been missed and the patient would have had a delayed diagnosis.
Patients diagnosed with breast cancer are at increased risk of developing an ipsilateral or contralateral breast cancer.
Synchronous breast cancers (occurring at the same time or within 6 months of the initial diagnosis) have a prevalence of 1 to 3%. Metachronous breast cancers (occurring greater than 6 months after initial diagnosis) have a prevalence of 5 to 7%.
Contralateral synchronous breast cancers detected by mammography are reported in 0.19 to 2.0% of patients, and detected by magnetic resonance imaging, in 9 to 10% of patients.
102.6 Management and Digital Breast Tomosynthesis Principles
A benefit of digital tomosynthesis-guided stereotactic-guided biopsy over the prone stereotactic biopsy table is the ability to use the full detector. The prone table is limited by a 50 × 50 mm field of view (FOV). The clear compression plate on the tomosynthesis biopsy unit allows visualization of the adjacent tissues. This can be extremely helpful when the lesion is difficult to target.
The current tomosynthesis biopsy units allow the performance of a biopsy using stereotactic localization with -15 degree and +15 degree imaging pairs, and the ability to use tomosynthesis-guided stereotactic-guided biopsy techniques. The technique needs to be chosen prior to the biopsy.
Tomosynthesis-guided biopsy techniques allow for biopsy of low-contrast lesions. This optimizes the biopsy of focal asymmetries, masses, and architectural distortions.
102.7 Further Reading
[1] Lee SG, Orel SG, Woo IJ, et al. MR imaging screening of the contralateral breast in patients with newly diagnosed breast cancer: preliminary results. Radiology. 2003; 226(3): 773‐778 PubMed
[2] Majid AS, de Paredes ES, Doherty RD, Sharma NR, Salvador X. Missed breast carcinoma: pitfalls and pearls. Radiographics. 2003; 23(4): 881‐895 PubMed
[3] Schrading S, Distelmaier M, Dirrichs T, et al. Digital breast tomosynthesis-guided vacuum-assisted breast biopsy: initial experiences and comparison with prone stereotactic vacuum-assisted biopsy. Radiology. 2015; 274(3): 654‐662 PubMed
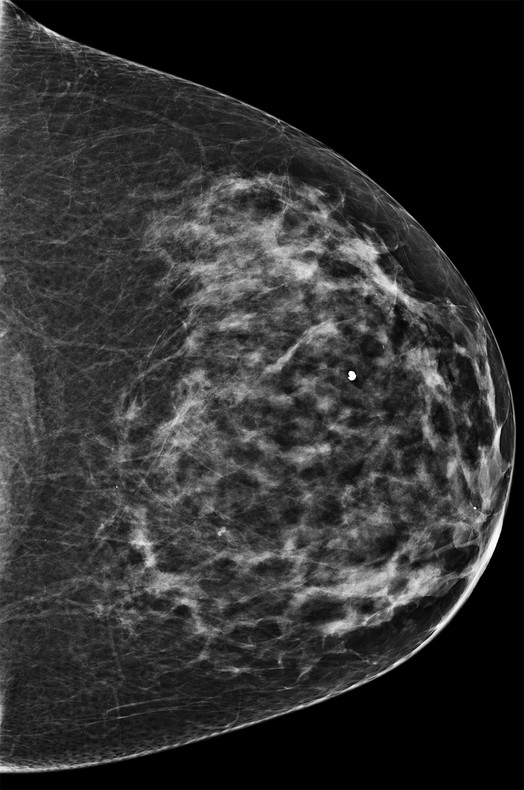
Fig. 102.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree