Presentation and Presenting Images
( ▶ Fig. 6.1, ▶ Fig. 6.2, ▶ Fig. 6.3, ▶ Fig. 6.4)
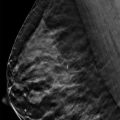
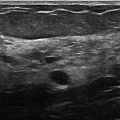
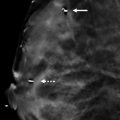
A 54-year-old female presents for screening mammography.
6.2 Key Images
( ▶ Fig. 6.5, ▶ Fig. 6.6)
6.2.1 Breast Tissue Density
There are scattered areas of fibroglandular density.
6.2.2 Imaging Findings
In the anterior depth of the right breast at the 11 o’clock location on the two-dimensional (2D) digital mammogram, there is an area of possible architectural distortion ( ▶ Fig. 6.6). This area appears more convincing on the craniocaudal (CC) view ( ▶ Fig. 6.5). The corresponding digital breast tomosynthesis (DBT) images (not shown) confirm that this is normal overlapping tissue.
6.2.3 BI-RADS Classification and Action
Category 1: Negative
6.3 Differential Diagnosis
Normal breast tissue (superimposition of breast tissue): Superimposition of tissue is a common occurrence in breast imaging and is a source of many recalled mammograms.
Surgical scar: Surgical scars are a source of architectural distortion on mammograms; however, this patient did not have any history of a surgical procedure. If in doubt, it is important to check the medical record.
Breast cancer: Breast cancer can present as architectural distortion; however, it is not very common. When architectural distortion is suspected to be breast cancer, it has a high positive predictive value. But in this case, the distortion was due to overlapping tissue.
6.4 Essential Facts
Summation artifacts, or superimposition of breast tissue, accounts for a substantial portion of the recalls (5%–25%) in a mammographic screening program.
A summation artifact occurs when normal breast tissue from different planes superimpose upon each other mimicking a lesion (also called a “pseudomass”).
Tomosynthesis technique, which limits the effects of overlapping structures, enhances lesion detection and can aid in determining if no lesion is present.
The decreased recall rate of digital breast tomosynthesis (DBT) increases the specificity of screening mammography.
6.5 Management and Digital Breast Tomosynthesis Principles
Tomosynthesis can decrease the number of benign recalls (false-positives) at screening mammography. Reports suggest DBT reduces the recall rate by 15 to17%.
There are significant added costs for unnecessary mammographic recalls – that of the diagnostic mammogram, the added patient time and anxiety, and the added radiation exposure.
Controversy exists as to whether DBT needs to be performed in both the craniocaudal (CC) and the mediolateral (MLO) projections. In a study by Rafferty and colleagues (2007), they found that in 35% of cases, the lesion was better visualized in one projection over the other. Most investigators have recommended performing DBT in both imaging planes to optimize lesion visualization.
Performing a combination 2D digital mammogram and DBT examination involves increased breast irradiation.
The appearance of radial scars stand out on DBT and thus are a source of false-positive findings.
6.6 Further Reading
[1] Kopans DB. Digital breast tomosynthesis from concept to clinical care. AJR Am J Roentgenol. 2014; 202(2): 299‐308 PubMed
[2] Rafferty EA. Digital mammography: novel applications. Radiol Clin North Am. 2007; 45(5): 831‐843, vii PubMed

Fig. 6.1 Right craniocaudal (RCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree