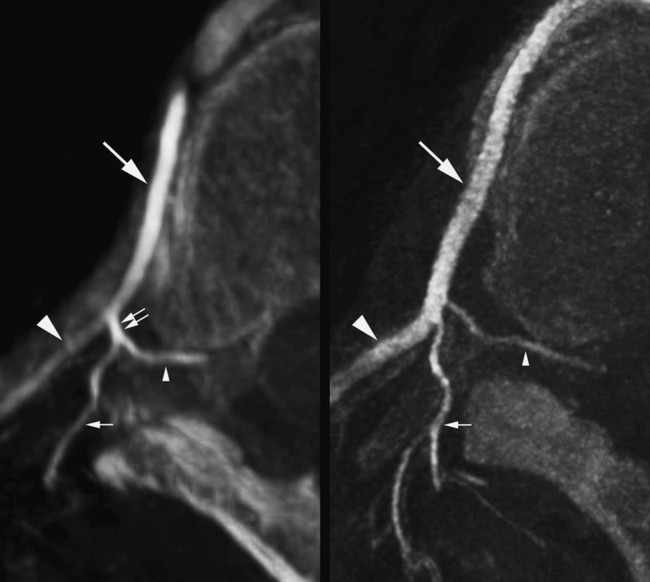
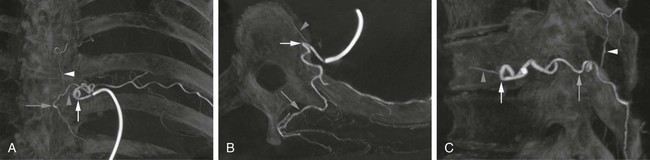
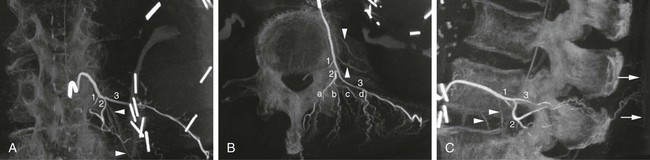
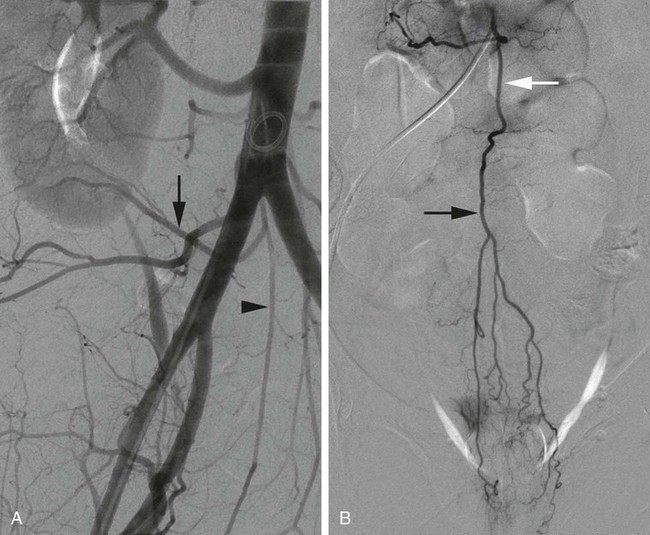
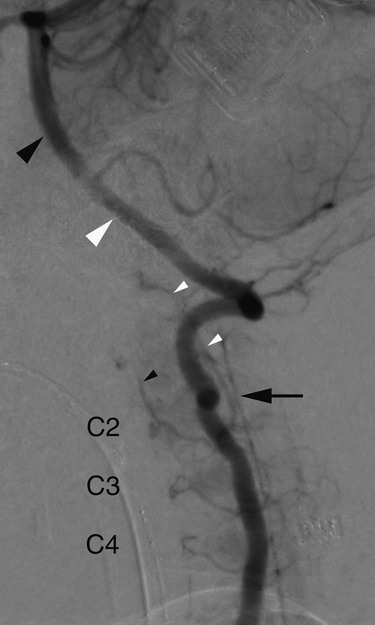
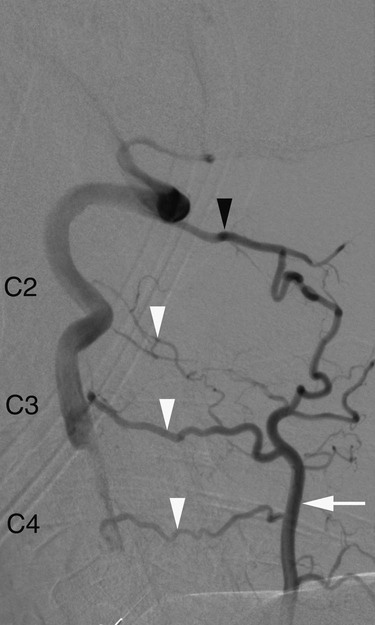
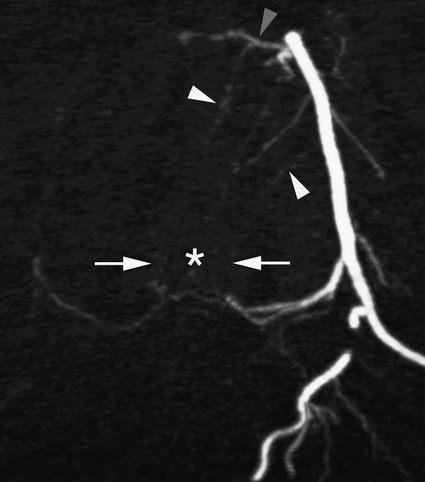
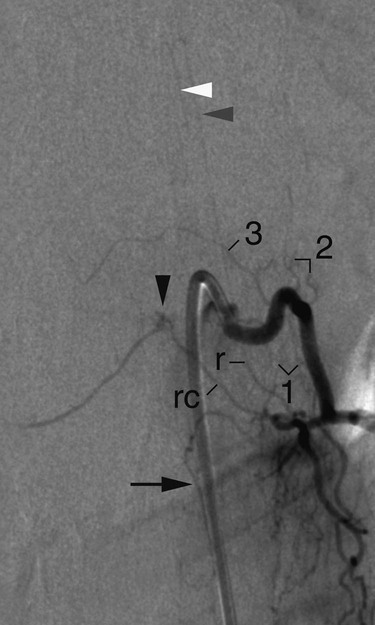
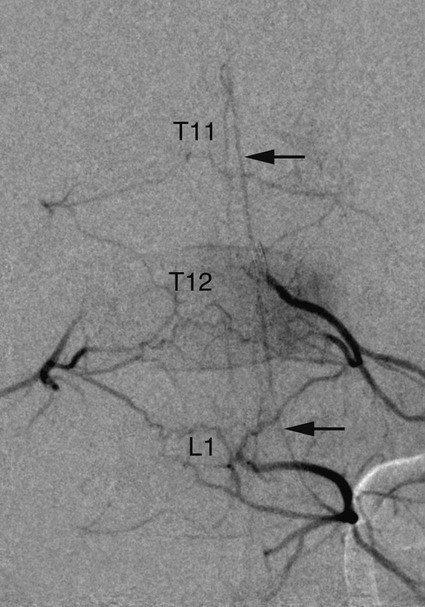
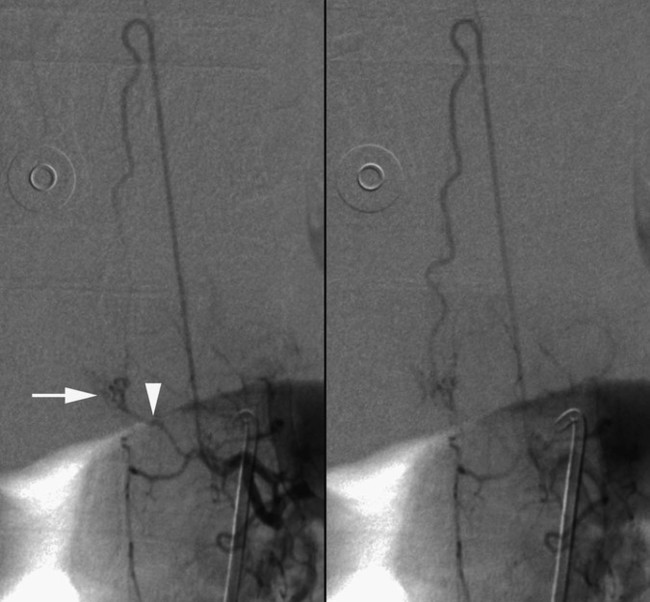
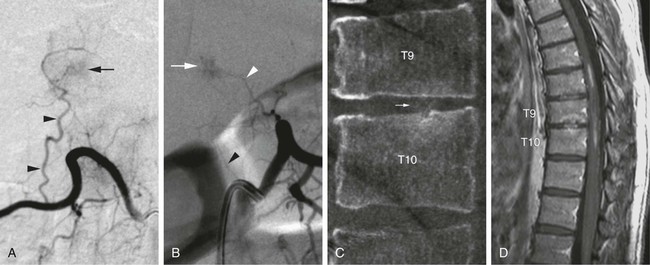
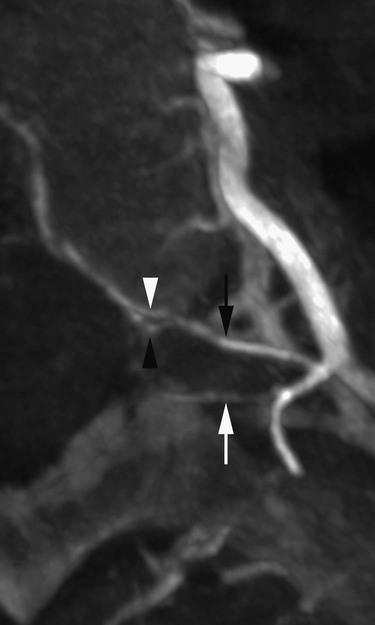
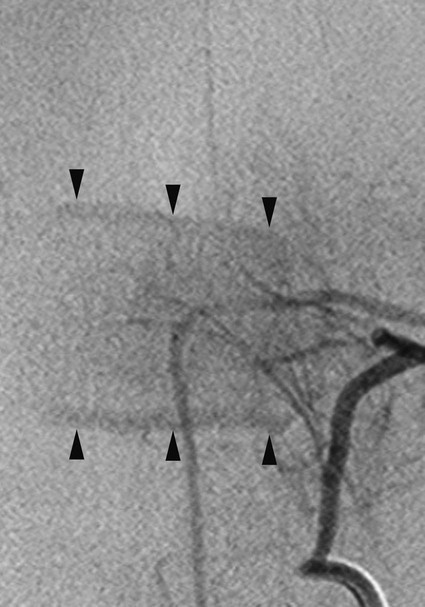
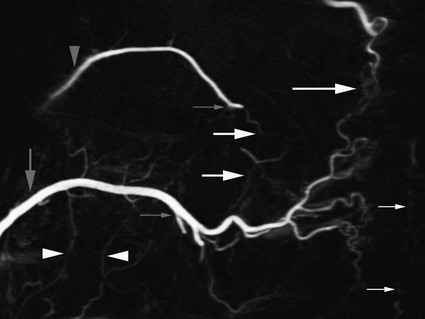
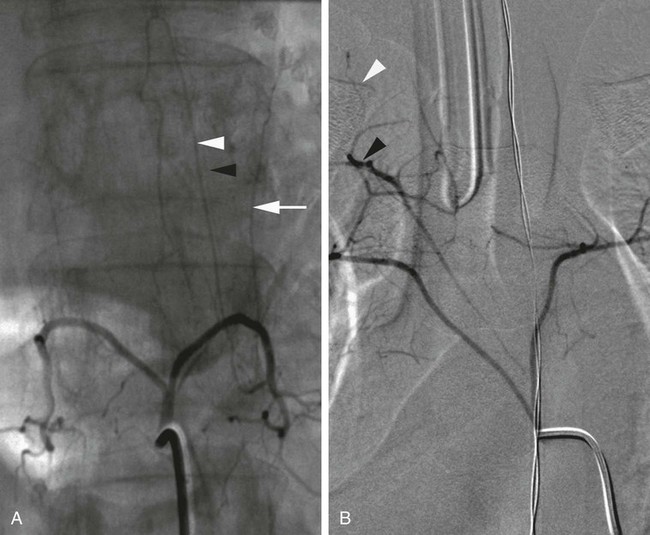
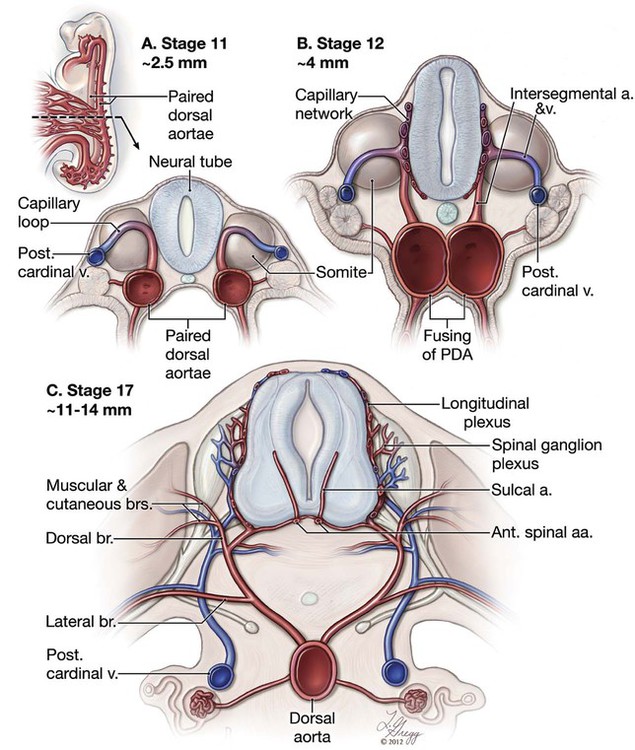
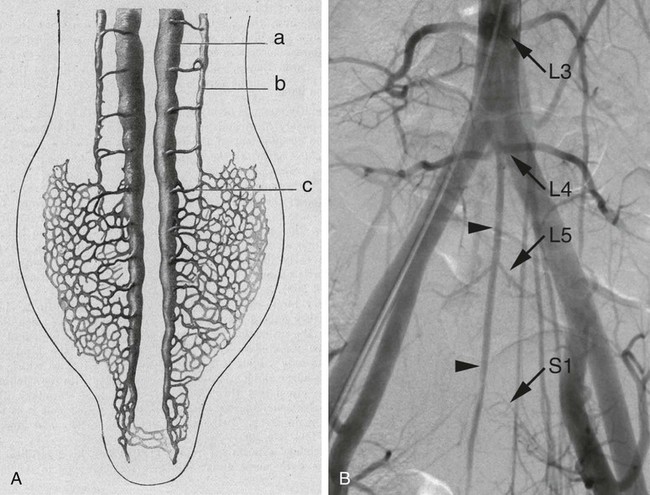
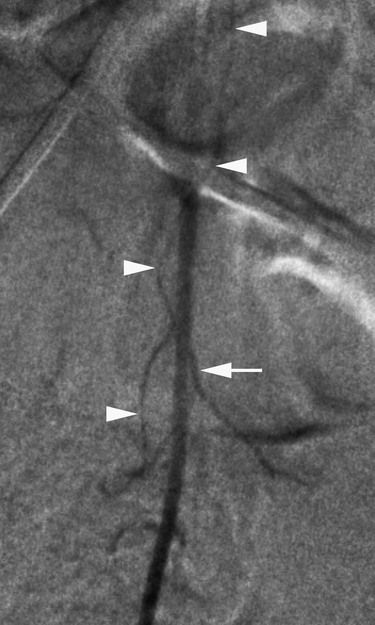
Chapter 88 Spinal digital subtraction angiography (SpDSA) is the gold standard imaging modality for evaluating vascular anomalies of the spine and spinal cord. Endovascular treatment of spinal vascular lesions was pioneered in the late 1960s1–3 shortly after the introduction of selective spinal angiography itself.4 Performing diagnostic and therapeutic SpDSA requires a solid understanding of the relevant vascular anatomy. This chapter offers an introduction to the arterial anatomy of the spine and spinal cord and discusses the basic principles of SpDSA. Each primitive dorsal aorta provides three groups of branches aligned in ventral, lateral, and dorsal rows. The dorsal rami start emerging early at the 6-somite stage, shortly after the still-unfused aortas have branched off the first ventral (or vitelline) arteries and slightly before the appearance of the first lateral branches.5 The dorsal branches stem from the primitive aortas in between somites, adopting an intersegmental rather than segmental distribution. These intersegmental arteries (ISAs) initially consist of capillary loops established between a dorsal aorta and the ipsilateral posterior cardinal vein. Later, the arterial and venous sides of the loops develop into the ISAs per se and their corresponding veins (Fig. 88-1, A-B).5 Rami sprouting from the arterial limb of the loops connect to similar vessels coming from contiguous ISAs to form longitudinal capillary plexi along the ventrolateral surface of the neural tube (Fig. 88-1, C). These plexi soon extend dorsally to cover the lateral surfaces of the neural tube as well.5 Transverse channels developing within this network form the primitive anterior and posterior radicular arteries, which are the first and, at this time, only branches of the ISAs. Capillaries extending further medially from each ventrolateral plexus establish a second set of longitudinal chains along the lateral edges of the floor plate of the neural tube. These chains correspond to the primitive anterior spinal arteries (ASAs), which will later coalesce more or less completely into a single ventromedian channel, the basilar artery cranially and the ASA caudally. In view of this developmental history, the dorsal branches and their capillary plexi for the spinal cord represent the fundamental anatomy of the ISA. At the adult stage, they correspond to the ISA stem and the spinal component of the dorsospinal artery (DA). Later-appearing branches include a dorsal branch (dorsal component of the DA) and a lateral branch (intercostal or lumbar arteries of the adult nomenclature) (see Fig. 88-1, C). The final configuration of the ISA depends upon the branching pattern of these secondary arteries; in particular, a DA exists only when the origin of the lateral branch is proximal to the takeoff of the spinal branch (Fig. 88-2). An understanding of the ISA based on its developmental anatomy is applicable at any vertebral level. Figures 88-3 and 88-4 show the typical configuration of thoracic and lumbar ISAs. Caudally, the median sacral artery (MSA) is the true continuation of the abdominal aorta beyond the takeoff of the common iliac arteries, derived themselves from the umbilical arteries6,7 (Fig. 88-5). The MSA remains temporarily connected with the capillary network supplying the hindgut and with the primary metanephric plexus.8,9 Through these connections, the MSA occasionally provides branches normally arising from the abdominal aorta,8 such as a renal artery (Fig. 88-6, A) or a superior rectal artery (Fig. 88-6, B). At the cervical level, longitudinal anastomoses linking the first six ISAs form the vertebral arteries (VA)10 (Fig. 88-7). According to Bracard, the VA is better described as a hemodynamic solution than a true artery.11 The distal V3 and V4 segments of the VA are formed by the enlarged spinal branch accompanying the first cervical nerve,12,13 a persistent segment of the proatlantal artery.14 The original intersegmental configuration, fairly apparent in children, accounts for the typical sources of collateral supply observed at the adult stage (Fig. 88-8). The vertebral body is vascularized by anterolateral and posteromedian osseous branches (Fig. 88-9). The anterolateral arteries originate from the stem of the ISA; they are divided into ascending, descending, and recurrent branches. Because of the leftward position of the aorta, they are more numerous on the right side than on the left.15 Ascending and descending branches connect with corresponding vessels from adjacent levels; these anastomoses often act as collateral supply pathways. They also participate in several anatomic variations described later in this chapter. After a short ascending course, the recurrent branch curves medially with a typical 90-degree angle to establish an anastomosis with the contralateral recurrent artery15 (Fig. 88-10). The spinal branch of the ISA usually divides into a radicular artery, coursing medially along the corresponding nerve root, and a retrocorporeal artery that provides the posteromedian osseous branches. Over the posterior aspect of the vertebral body, the retrocorporeal artery participates in the formation of a rich anastomotic network by joining analogous branches from adjacent levels. The retrocorporeal artery is frequently targeted during preoperative spinal embolization, so the presence of dangerous anastomoses within this network has to be kept in mind (Fig. 88-11). The cluster of posteromedian osseous branches is often associated with a prominent blush that can mimic a vascular anomaly (Fig. 88-12). Similarly, an enhancing Schmorl’s node can simulate a more aggressive pathology such as a metastasis (Fig. 88-13). The three branches of the ISA passing through the neural foramen are also known as the anterior, intermediate, and posterior spinal canal arteries.15 The anterior and intermediate branches are the retrocorporeal and radicular arteries, the posterior one is the prelaminar artery.16 These branches can have a common origin (i.e., the spinal branch in its complete form16) or originate separately (Fig. 88-14). The left and right prelaminar arteries establish an anastomotic network along the anterior aspect of the posterior vertebral arch that is often difficult to differentiate from the retrocorporeal network on angiographic projections. A modification of the retrocorporeal anatomy is seen at the level of the odontoid process, which is principally vascularized by two branches of the VA, the anterior and posterior ascending arteries17,18 (see Fig. 88-7). The posterior ascending artery is a cranial extension of the C2 retrocorporeal artery that courses upward within the anterior epidural space. It assumes a typical ogival shape around the odontoid process as it connects with the contralateral posterior ascending artery to form the apical arcade17,20 (see Fig. 88-29, B). The odontoid process receives additional supply from the ascending pharyngeal artery, notably a branch joining the apical arcade via the hypoglossal canal.19 A selective ISA angiogram usually results in visualization of a hemivertebral blush. The extent and conspicuity of that blush varies among individuals. Anastomoses linking osseous branches from adjacent/opposite ISAs explain the common visualization of partial or even complete hemivertebral blushes in adjoining vertebrae, or of a bilateral blush at the studied level. In children, the vertebral blush appearance depends upon the maturation of the growth plate and the progressive dominance of the anterolateral group of osseous branches over the posterior median one (Fig. 88-15) (Gailloud, unpublished data). The evolution of the blush also reflects the transition of the vertebral vascularization from the rich arterial network seen in children to the end-artery configuration of adults, a switch completed at about age 15.20 The conspicuity of the hemivertebral blush decreases with age as bone marrow is progressively replaced with fat. The stem of lumbar ISAs gives several superficial and deep branches to the psoas muscle (see Fig. 88-4, B).15 The paraspinal musculature is principally vascularized by the dorsal component of the DA via its medial, intermediate, and lateral muscular branches. Posterior perforators of the lateral branch of the ISA also contribute, either directly or by anastomosing with the lateral muscular branch of the DA (see Fig. 88-4, B). Despite extensive interconnections, the muscular branches continue to exhibit a segmental pattern at the adult stage. The terminal skin arteries, on the other hand, have less predictable territories owing to cutaneous shifting and vascular redistribution.5 Anastomoses between the osseous, muscular, and cutaneous branches of adjacent or opposite ISAs offer a wide range of potential collateral pathways. Figure 88-16 illustrates some typical connections, in particular the anterior and posterior laterovertebral anastomoses, which are commonly involved in anatomic variations and represent potential dangerous anastomoses during endovascular procedures. ISA trunks can be ipsilateral (i.e., involving arteries from two or more consecutive vertebral levels) or bilateral (i.e., providing the left and right ISAs for a single level). Bilateral trunks are most common in the lower lumbar region but exceptional in the mid- and upper thoracic regions (except in the Japanese population, according to Adachi21) (Fig. 88-17). A bilateral trunk is often falsely suggested by the origin of L4 or L5 ISAs from the MSA (see Fig. 88-5, B); a bilateral trunk must show a common stem arising from the MSA itself (Fig. 88-18). Ipsilateral trunks can be seen at any vertebral level. They are common in the upper thoracic region. Caudally, they are generally seen at L3, L4, or L5; they can involve several consecutive levels, with a complex interplay of spinal and muscular branches. The most extreme form of trunk reported so far consists of a single ascending midline vessel providing bilateral ISAs from T12 to T3.22 Ipsilateral trunks are divided into complete and incomplete types. To be complete, an ipsilateral trunk must have a full set of branches for each vertebral level it supplies. These include (1) an anterior component (or stem) providing the anterolateral osseous branches, (2) a lateral component (i.e., the lumbar, subcostal, or intercostal artery), (3) a dorsal component supplying the paraspinal musculature, and (4) a spinal component branching off the radicular artery (Fig. 88-19). The dorsal and spinal components, when sharing a common origin, form a DA. In the classic form of incomplete unilateral trunk, a DA missing at one of the levels supplied by the trunk arises separately from the aorta. This configuration, reported by Chiras and Merland in 1979,23 is known as an isolated DA or direct emergence of the DA from the aorta23–26 (Fig. 88-20
Arterial Anatomy of the Spine and Spinal Cord
Introduction
Developmental Anatomy
Arteries of the Vertebral Body
Muscular and Cutaneous Branches
Intersegmental Artery Trunks
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Arterial Anatomy of the Spine and Spinal Cord