Key Points
- ▪
An arteriovenous fistula typically lies closer to the skin surface than the native vessel and is therefore more likely to be easily compressed by the probe during scanning, falsely suggesting narrowing. Hence, when scanning, use very light pressure and lots of gel.
- ▪
The flow velocity within a arteriovenous fistula is slower in a mature and well-dilated arteriovenous fistula than in a recently created, smaller diameter vein. Volumetric flow is a more reliable measurement.
Hemodialysis first became available, albeit in a limited fashion, in 1962 in Seattle. The first hemodialysis fistula was created in 1966. Until the 1980s, relatively low median dialysis flow rates were used, and thus even patients with small-veined fistulas could achieve adequate hemodialysis. By the mid-1980s, it was established that urea clearance time could be improved with higher blood flows during dialysis, with very little increase in dialysis time. This, in turn, led to a preference for grafts over fistulas that could more easily handle the increase in flow required and could be used sooner after surgery than fistulas.
In 1997, the National Kidney Foundation Kidney Disease Outcomes Quality Initiative (KDOQI) published a set of evidence-based practice guidelines for vascular access. These guidelines recommended that the primary placement for hemodialysis be autogenous arteriovenous fistula in preference to synthetic grafts. Although arteriovenous fistulas have a higher primary failure rate than arteriovenous grafts, the fistulas are less prone to infection and thrombosis and require less corrective intervention.
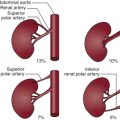
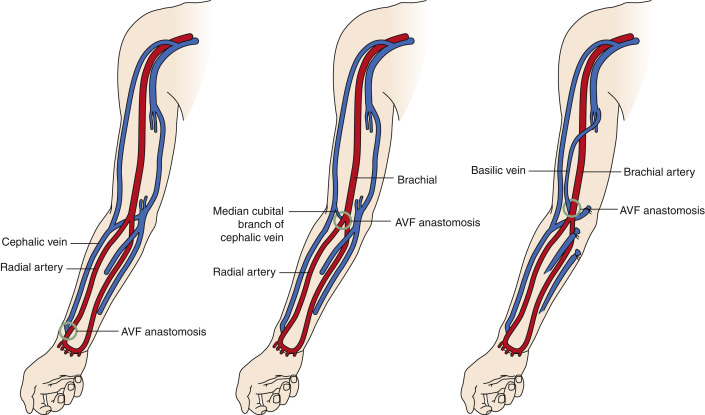
There are many different configurations of arteriovenous fistulas. The preferred and most commonly used are created in the upper extremity: radiocephalic, brachiocephalic, and brachiobasilic transposition ( Fig. 4-1 ). Brachiobasilic transposition has been increasingly used in patients possessing veins of insufficient caliber to support the preferred radiocephalic or brachiocephalic fistulas. This involved the transposition of the basilic vein, a vein not used for venipuncture, and therefore much less likely to be diseased than the cephalic vein, to a more superficial level, by dissecting and tunneling the vein to a position that can be more easily reached by the dialysis needle (1 to 1.5 inches in length). The normal volumetric flow through an arteriovenous fistula is held to be >600 mL/min.
Between 20% and 50% of fistulas fail to mature, due principally to the development of stenosis at the venous anastomosis, but also to a lesser extent, due to the presence of large branch veins.
Duplex Scanning
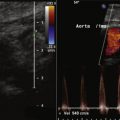
Duplex scanning is used to provide accurate preoperative diameter measurements of the cephalic and basilic veins of the forearm and upper arm (vein diameter > 3 mm is preferred), and also, to determine whether there is stenosis or chronic recanalized thrombosis caused by damage from previous indwelling catheters or venipuncture.
To assess for patency, the veins at the axilla and below are scanned in their entirety and compressed, in short axis, by the transducer at 1- to 2-cm intervals. The subclavian and proximal axillary veins usually collapse briefly if the patient takes in a long “sniff” breath. If the cephalic vein appears to be deeper than usual, the vein is measured with respect to the skin level. Most surgeons also want to know if any significant accessory branch vessels are present (e.g., accessory cephalic vein), which might divert flow away from the main outflow channel.
The scan may be unilateral or bilateral, but the nondominant arm is preferred for access creation. Previously unsuccessful access attempts influence which vessels are most likely to be used for fistula creation.
A full upper extremity arterial scan is also performed to include diameter measurement of the radial artery to uncover any evidence of wall calcification or stenosis that would interfere with the ability of the artery to dilate after surgery. There is a significant prevalence of a high brachial artery bifurcation, and this should be documented when present. Duplex protocol for vein mapping is given in Table 4-1 .
| VENOUS ANATOMIC SEGMENT | TECHNIQUE | DUPLEX INTERROGATION |
|---|---|---|
| SAX sweep with or without compression | Grayscale |
| Grayscale | |
| SAX sweep with or without compression | Grayscale |
| Grayscale | |
| Brachial veins | SAX sweep with or without compression | Grayscale |
| Axillary vein | SAX sweep with or without compression | Grayscale |
| Grayscale/color Doppler/pulsed-wave spectral | |
| Subclavian vein |
| Grayscale/color Doppler/pulsed-wave Doppler |
| Internal jugular vein | SAX sweep | Grayscale |
| LAX sweep | Grayscale/color Doppler/pulsed-wave Doppler | |
| Brachiocephalic vein | LAX | Grayscale/color Doppler/pulsed-wave Doppler |
| Radial artery | SAX sweep | |
| Diameter: distal | Grayscale | |
| LAX sweep | Grayscale/color Doppler/pulsed-wave Doppler | |
| Brachial artery | SAX sweep | Grayscale |
| LAX sweep | Grayscale/color Doppler/pulsed-wave Doppler | |
| Axillary artery | LAX sweep | Grayscale/color Doppler/pulsed-wave Doppler |
| Subclavian artery | LAX sweep | Grayscale/color Doppler/pulsed-wave Doppler |
| Brachiocephalic artery | LAX sweep | Grayscale/color Doppler/pulsed-wave Doppler |
Duplex Interpretation and Reporting
Venous Scan: Venous Criteria
Compressibility is the main criterion for the forearm and upper arm veins. Evidence of partial compressibility, accompanied by an intraluminal “cavitational” appearance on grayscale, most likely occurs as a result of thickened walls and recanalized organized residual thrombus. The walls and the thrombus are caused by previous venous cannulation that renders these veins unsuitable for use as a conduit for hemodialysis.
Signs of Deep Vein Thrombosis
Noncompressibility
The venous system is normally distended under low pressure, and as such, veins are compressed easily with very little pressure required from the transducer. With venous thrombosis, the presence of intraluminal thrombus material renders the vein incompletely or noncompressible. Compression maneuvers are best performed in short-axis imaging, because it can be assured that the plane of imaging is not moving off to the side of the vessel, giving a false impression of compressibility as can occur with long-axis imaging. Generally, soft tissue material within the vessel is seen at sites of incompressibility.
Flow Obstruction
Typically, venous flow exhibits spontaneous respiratory variation and in proportion to respiratory effort. In addition, normally, abrupt compression of a muscle bed distally to a site of sampling results in a surge of blood through the vein. With complete obstruction to flow by deep venous thrombosis, the signs of spontaneity, phasicity, and augmentation are lost. With partial obstruction, these signs are attenuated. Therefore, flow signs corroborate some cases of deep venous thrombosis; however, from a diagnostic and therapeutic standpoint, there is no difference between occlusive and nonocclusive thrombosis.
Arterial Scan
Obtain representative peak systolic velocity measurements along the artery every 2 to 3 cm. When a lesion is detected with grayscale scanning and color Doppler flow mapping, record peak systolic velocity measurements immediately proximal to the site of stenosis, within the stenosis, and immediately distal to it. Criteria for arterial occlusive disease are listed in Table 4-2 .