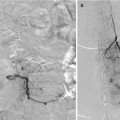
Fig. 1
Left vertebral origin stenosis treated with a balloon-mounted stent. 3.5 mm Pharos balloon expandable stent

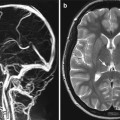
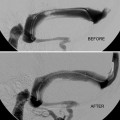
Fig. 2
Left intradural vertebral stenosis treated with a balloon-mounted stent. Intradural vertebral stenosis pre- and post-stenting
Post-dilatation a check angiogram is performed and, if appearance is satisfactory, the delivery system is removed.
Rarely the lesion needs to be pre-dilated.
Technical tip: Access to the right vertebral can often be difficult, and sometimes using a 7 French sheath with a wire into the subclavian stabilizes the system to gain access.
Brachial artery puncture using a 5 French sheath is sometimes necessary for access.
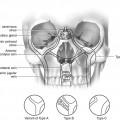
Stent Types
Monorail preferred; various stent types are available including cardiac, renal, and specific intracranial stents such as the Pharos.
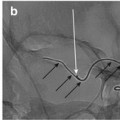
Intracranial Stenting
Premedication as above. Heparinization as above.
Procedure is ideally performed under general anesthesia.
Both balloon-mounted Pharos and self-expanding (Wingspan) stents are used. Self-expanding stents usually require pre-dilatation of the lesion using a gateway balloon to approximately 75 % of the diameter of the normal vessel before deployment of the stent. Dilation beyond this risks vessel rupture and catastrophe.
Post-procedure Care
Extracranial can be managed in a high dependency unit overnight. Heparinization is not necessary for extracranial stents.
Intracranial stenting – essential the patient has access to an HDU or even an ITU bed overnight for close monitoring of blood pressure and other neurological parameters. Heparinization is usually continued for 24 h after the procedure.
It goes without saying that all of these patients have atheromatous disease and will be managed by a neurologist or stroke physician with control of risk factors such as hypertension, glucose, and cholesterol.
Imaging Follow-Up
Unless follow-up is prescribed as part of a trial, noninvasive imaging such as ultrasound, particularly to look at flow through an origin stenosis, or CTA or MRA is recommended.
Catheter angiography is reserved for those who become symptomatic or as follow-up as part of a trial.
Key Points
The risk of stroke following vertebrobasilar TIA/minor stroke is as high as for the carotid circulation.
The risk is highest earliest after TIA.
CEMRA and CTA provide sensitive screening for vertebral stenosis.
Stenotic disease occurs in approximately 20–30 %.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree