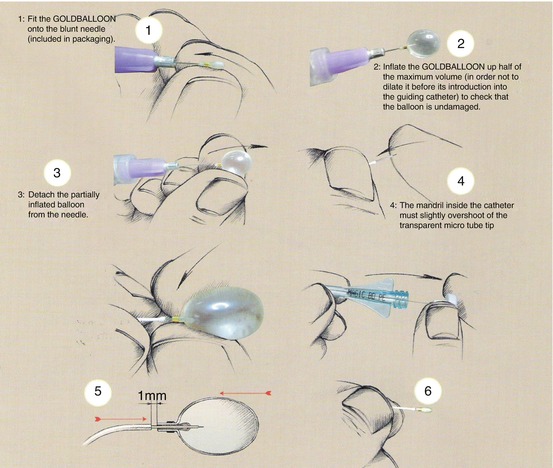
Fig. 1
(a) Angiographic narrowing (arrows) of codominant left proximal vertebral artery by encasing recurrent malignant cervical sarcoma. (b) Native image showing position of three detachable balloons which resulted in immediate/permanent vessel occlusion facilitating en bloc tumor resection 2 weeks later. (c) Preparation of the Goldballoon (With Permission from Balt Extrusion, Montmorency, France)
Goldballoon (Goldbal 1–5; Balt Medical, Montmorency, France)
Commercially available in most countries (excluding USA)
Range of sizes available: match to vessel lumen
Technically challenging/fragile in unfamiliar hands
Tips on Preparation
A minimum of two balloons should be prepared at the outset – prepare the first balloon and inflate with 50 % contrast/saline and leave inflated while preparing the second device. This will confirm integrity of the first balloon.
Reinsert the mandrill into the delivery microcatheter (with tip just inside the deflated balloon taking care not to damage it). This will support its passage through the guide catheter.
Tips on Safe Deployment
Always have a second balloon prepared and ready for deployment before introducing the first.
Once in the parent artery, remove the mandrill. Attach a 1 mL syringe of contrast/saline mixture via a two-way tap to the microcatheter.
Once fully clear of the guide catheter, partially inflate the balloon to ensure visualization and use flow guidance to navigate the balloon catheter to the desired position.
Further inflate the balloon gently until it fills the lumen and begins to elongate along the long axis of the parent artery (maximum inflation volume should never be exceeded).
It may be necessary to deflate and reinflate the balloon more than once while advancing/withdrawing the microcatheter to ensure appropriate positioning.
Once adequately inflated, perform gentle guide catheter angiography to confirm parent vessel occlusion while avoiding washing the balloon from the microcatheter prematurely and risking distal balloon embolization.
Once satisfied gently pull the microcatheter until the balloon detaches from the microcatheter tip – often requires considerable retraction force and may be assisted by advancing the guide catheter to abut the lower end of the balloon to hold in place; care must be taken not to allow the guide catheter to push the balloon forwards.
This is the most dangerous stage and further angiography should be avoided until position secured with additional proximal balloon(s).
Deploy a second proximal balloon using similar technique as soon as is safely possible.
Consider a third balloon for security (should one of the first two subsequently fail).
Final angiography is necessary to confirm occlusion and collateral flow and exclude complications.
Pros: Rapid occlusion, inexpensive
Cons: Fiddly to use, device fragile and may be damaged, risk of distal embolization of undersized balloon, risk of balloon deflation over time and recanalization of vessel, limited availability in some areas
Detachable Coil Occlusion (Fig. 2)
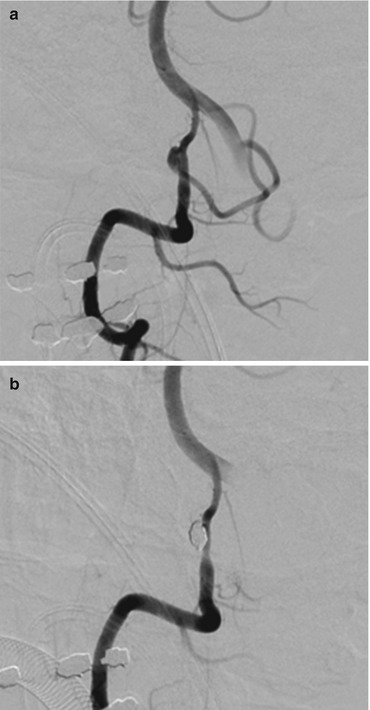
Fig. 2
(a) Recently ruptured right posterior inferior cerebellar artery (PICA) origin aneurysm in patient with poor grade subarachnoid hemorrhage. (b) Occlusion of aneurysm lumen and proximal PICA with detachable coils (no resulting attributable cerebellar or brainstem infarct in this case)
Coil occlusion involves familiar devices but occlusion of a “normal” vessel can be a difficult and lengthy procedure with two major challenges:
1.
Getting first coil to form a stable platform in a tubular structure
2.
Achieve sufficient packing density to establish rapid occlusion
May be assisted by:
Start coil deployment at a bend, dilatation, narrowing, or branch in the parent vessel to engage the first coil and promote formation a complex structure.
More rapid occlusion may be achieved by hydrogel coils which will swell inside the vessel or fibered coils which promote thrombosis.
Two-catheter technique – holding the undetached first coil in place and deploying further coils against it via a second catheter.
Proximal nondetachable to occlusion balloon to temporarily eliminate antegrade flow during coiling (especially dual lumen balloons such as Ascent (Micrus/Johnson & Johnson) and Sceptre (MicroVention) where coils can be deployed directly through balloon lumen).
Pros: Familiar devices, widely available
Cons: May be difficult to get coils to sit in tubular lumen
Usually slow, gradual occlusion – risk of distal embolization
Expensive – often needs many coils
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree