Aspergillosis, Angioinvasive
Helen T. Winer-Muram, MD
Key Facts
Terminology
Invasive aspergillosis: Tissue invasion either angioinvasive or airway invasive, typically occurs in patients with neutropenia or impaired neutrophil function
Imaging Findings
Nodules, single or multiple
Hypodense sign: Central hypodensity, due to infarction
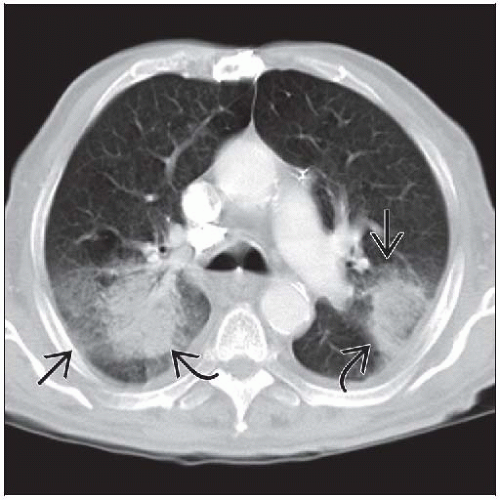
Halo sign: Large bull’s eye surrounded by smaller rim ground-glass opacification
Ground-glass attenuation corresponds to rim of hemorrhage
CT angiogram sign: Vessels cut off at edge of nodule
Air crescent sign, late sign, follows recovery of neutrophils
Top Differential Diagnoses
Halo Sign
Mucormycosis
Tuberculosis
Bacterial Abscess
Metastases: Angiosarcoma
Pathology
Hyphae invade vessels or airway walls causing occlusion
60% of fungal pneumonias in immunocompromised patients are caused by Aspergillus
Clinical Issues
Neutropenia main risk factor
Surgery may be indicated in some patients, particularly for treatment of massive hemoptysis
TERMINOLOGY
Abbreviations and Synonyms
Invasive pulmonary aspergillosis (IPA), chronic necrotizing pulmonary aspergillosis = semi-invasive aspergillosis
Definitions
Invasive pulmonary aspergillosis
Tissue invasion, either angioinvasive or airway invasive; typically occurs in patients with neutropenia or impaired neutrophil function
Semi-invasive aspergillosis
Indolent pulmonary infection in mildly immunocompromised patients
Prolonged corticosteroids, malignancy, diabetes, alcoholism, sarcoidosis
IMAGING FINDINGS
General Features
Best diagnostic clue: Fulminant lung disease in febrile neutropenic patient
Patient position/location
Invasive aspergillosis, no lobar predilection
Semi-invasive aspergillosis, upper lobes
Size: Nodule(s) from 6 mm to 3 cm
Morphology: Mass(es), consolidation with central hypodense sign or halo sign
CT Findings
Angioinvasive
Nodules, single or multiple, typically < 10 in number
6 mm to 3 cm
Hypodense sign, early sign
Central hypodensity in nodule or consolidation, due to infarction
Usually more than 50% of lesion
Halo sign, early sign
Mass-like lung consolidation or nodules surrounded by ground-glass attenuation
Bull’s eye larger than halo
Very suggestive of invasive aspergillosis in immunocompromised patient
Warrants starting antifungal therapy before confirmation with other tests
CT angiogram sign
Interruption of peripheral segmental artery at edge of nodule
Vessel not visible in lesion
Best demonstrated on MIP reconstructions
Air crescent sign, late sign
Crescentic and eventual circumferential cavitation
Fragments of infarcted lung separate from adjacent parenchyma (pulmonary sequestra)
Has limited utility for diagnosis, seen in up to 50%
Occurs during convalescence and recovery of neutrophil count, typically 2-3 weeks after therapy started
May evolve to reassemble aspergilloma or thin-walled cyst
Typically close in 2-3 weeks
Consolidation
Pleural-based wedge-shaped consolidation similar to infarct
May also show hypodense sign
May traverse fascial planes, invading pleura, chest wall, pulmonary artery, pericardium, heart, mediastinum
Airway invasive aspergillosis
Less common than angioinvasive (30%)
Centrilobular nodules, tree-in-bud opacities
Consolidation centered on airways (peribronchial)
Invasive tracheobronchial aspergillosis
Ulcerations of trachea and central bronchi
Can be associated with atelectasis and consolidation
Sometimes seen in lung transplant recipients
Semi-invasive aspergillus
Varied appearance, may present as slowly growing nodule or focus of consolidation at lung apex, mimics post-primary tuberculosis
Progressive upper lobe cavitary consolidation, pleural thickening
An aspergilloma can be present
Associated with preexisting pulmonary emphysema
Pleural effusion, 10%
May show hypodensities in liver, spleen, or kidneys, indicating disseminated disease
Radiographic Findings
Findings often nonspecific, new focal or multifocal abnormalities best investigated with CT
Invasive pulmonary aspergillosis
Initially, chest radiograph can be normal
Lung nodules or areas of consolidation can progress rapidly
Air crescent sign
Crescent-shaped gas collection within pulmonary nodule or consolidation
Can progress to extensive cavitation and necrosis
Can invade pleural space, causing empyema or pneumothorax
Semi-invasive aspergillosis
Mimics post-primary tuberculosis
Imaging Recommendations
Best imaging tool: HRCT best to show central necrosis, halo sign, air crescent sign
Protocol advice: MIP reconstructions for angioinvasion
DIFFERENTIAL DIAGNOSIS
Halo Sign
Infections
Mucormycosis, candidiasis, coccidioidomycosis, cryptococcus
Candida: Involves small blood vessels, random distribution
Tuberculosis, mycobacterium avium intracellulare
Coxiella burnetii
Herpes simplex, varicella-zoster, cytomegalovirus, myxovirus
Bacterial abscess, Pseudomonas aeruginosa, legionella
Primary tumors
Squamous cell carcinoma, Kaposi sarcoma, bronchioloalveolar cell carcinoma, adenocarcinoma
Metastases: Angiosarcoma, Kaposi sarcoma, choriocarcinoma, osteosarcoma, melanoma, hydatiform mole, gastrointestinal malignancies
Pulmonary emboli
Wedge-like consolidation or pulmonary infarcts
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree