LEARNING OBJECTIVES
1. Recognize partial or complete atelectasis of the following on a chest radiograph or computed tomography (CT):
• Right upper lobe
• Right middle lobe
• Right lower lobe
• Right upper and middle lobe
• Right middle and lower lobe
• Left upper lobe
• Left lower lobe
2. Recognize complete collapse of the right or left lung on a chest radiograph or CT and list an appropriate differential diagnosis for the etiology of the collapse.
3. Recognize lung collapse related to massive pleural effusion on a frontal chest radiograph.
Atelectasis is defined as “diminished volume affecting all or part of a lung, which may or may not include loss of normal lucency in the affected part of lung (this finding is not to be confused with diminished volume produced by resection of pulmonary tissue)” (1). The term is derived from the Greek words ateles and ektasis and means “incomplete expansion” (2–4). The term collapse is used when a whole lobe or lung is involved. Pulmonary atelectasis is one of the most commonly encountered abnormalities in chest radiology. Recognizing an abnormality on chest radiography as being caused by atelectasis can be crucial in understanding the underlying pathology, such as a case of left upper lobe collapse in an adult with endobronchial carcinoma obstructing the left upper lobe bronchus. In this chapter, atelectasis will be used to describe pulmonary loss of volume without substantial filling of alveolar spaces. The term alveolar lung disease implies filling of alveolar spaces with fluid or other material. This chapter will review the types of atelectasis on the basis of mechanism, the signs of atelectasis, and the radiologic manifestations of lobar and nonlobar atelectasis.
TYPES OF ATELECTASIS
Pulmonary atelectasis can be divided into six types, on the basis of mechanism: resorptive, adhesive, compressive, passive, cicatrization, and gravity-dependent. Whereas atelectasis can be divided into types on the basis of these different mechanisms, in any given patient several mechanisms can occur simultaneously.
Resorptive atelectasis, the most common type, results from resorption of gas from the alveoli when communications between the alveoli and the trachea are obstructed. Resorptive atelectasis is therefore also referred to as obstructive atelectasis. The obstruction can occur at the bronchial or bronchiolar level. The most important condition producing intrinsic bronchial obstruction is lung cancer. Other causes of bronchial obstruction include other neoplasms, inflammatory etiologies (especially tuberculous or fungal infection), aspirated foreign bodies, mucous plugging (Fig. 11.1), a malpositioned endotracheal tube (Fig. 11.2), and extrinsic compression of an airway by neoplasm, lymphadenopathy, aortic aneurysm, or cardiac enlargement. Resorptive atelectasis is most commonly caused by obstruction of the small peripheral bronchioles, from impairment of mucociliary transport and pooling of retained secretions in the smaller airways. The larger airways are often patent and filled with air, resulting in air bronchograms within the atelectatic lung (Fig. 11.3). The presence of air bronchograms within the atelectatic lung usually, but not always, indicates the absence of a central obstructing neoplasm. Some of the conditions known to impair mucociliary clearance include thoracic and abdominal pain, central nervous system depression, respiratory depressant medication, general anesthesia, endotracheal intubation, and inhalation of toxic fumes or smoke (5). Resorptive atelectasis can also be associated with certain chronic obstructive airway diseases (e.g., asthma, chronic bronchitis, and emphysema), and it can be seen in acute bronchitis, bronchiolitis, and aspiration and other types of pneumonia from obstruction of small airways by inflammatory exudate.
Atelectasis resulting from surfactant deficiency is termed adhesive atelectasis. Insufficient surfactant leads to alveolar collapse; once collapsed, the alveolar walls tend to adhere, making reexpansion difficult. Diffuse surfactant deficiency can result from hyaline membrane disease, acute respiratory distress syndrome, smoke inhalation, cardiac bypass surgery, uremia, and prolonged shallow breathing (5). Rounded atelectasis is a form of juxtapleural lung collapse associated with chronic pleural disease, usually related to asbestos exposure (Fig. 11.4). A proposed mechanism of rounded atelectasis is collapsed lung floating on pleural effusion and development of fibrous adhesions suspending the rounded atelectatic area in an elevated and tilted position. The diagnosis can be made when computed tomography (CT) shows atelectatic lung contiguous with chronic pleural effusion/thickening, crowded vessels and bronchi sweeping into and around the base of the atelectatic lung, and volume loss in the affected lobe.
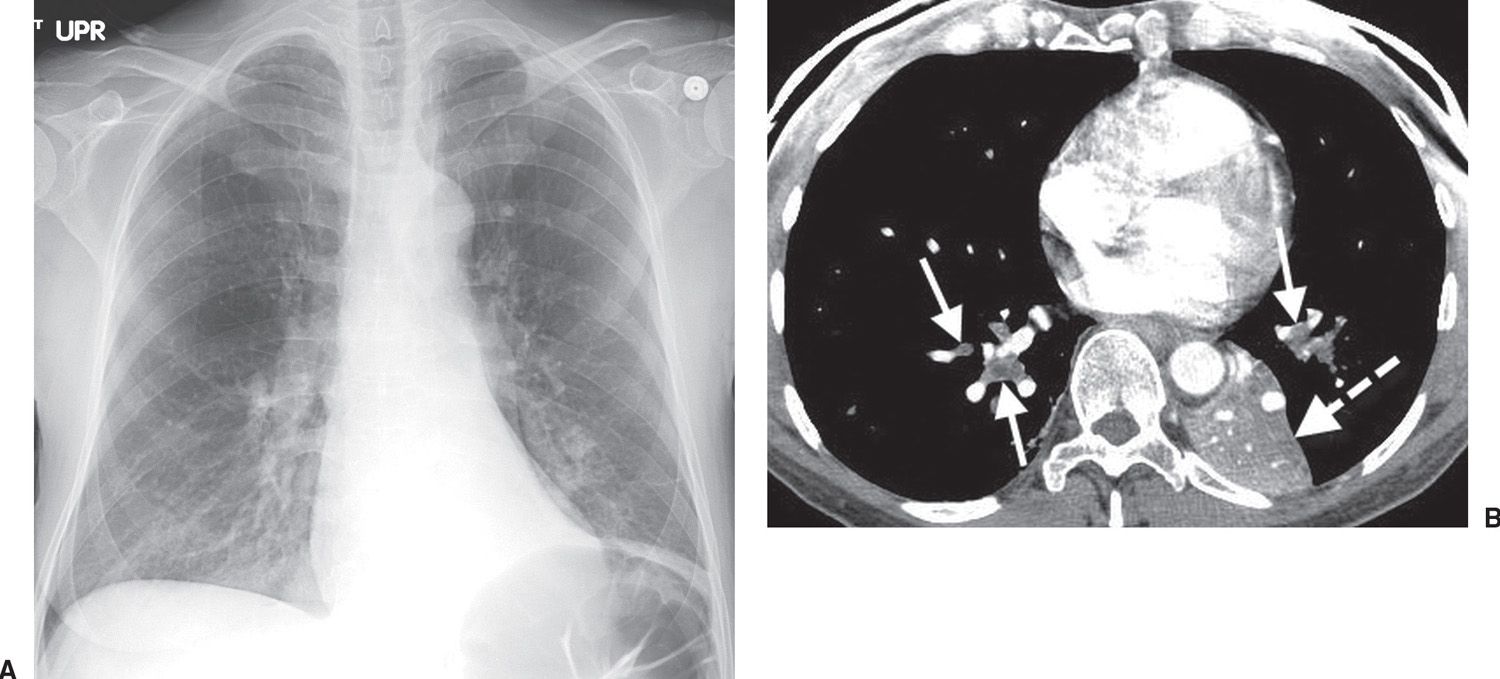
FIG. 11.1 • Lower lobe atelectasis. A: PA chest radiograph of a 45-year-old man with shortness of breath shows abnormal opacity at the left base and elevation of the left hemidiaphragm. B: CT shows low-attenuation mucus (solid arrows) filling the lower lobe airways. The airways abut the accompanying enhancing pulmonary arteries. Note the left lower lobe collapse, associated with medial and posterior displacement of the left major fissure (dashed arrow).
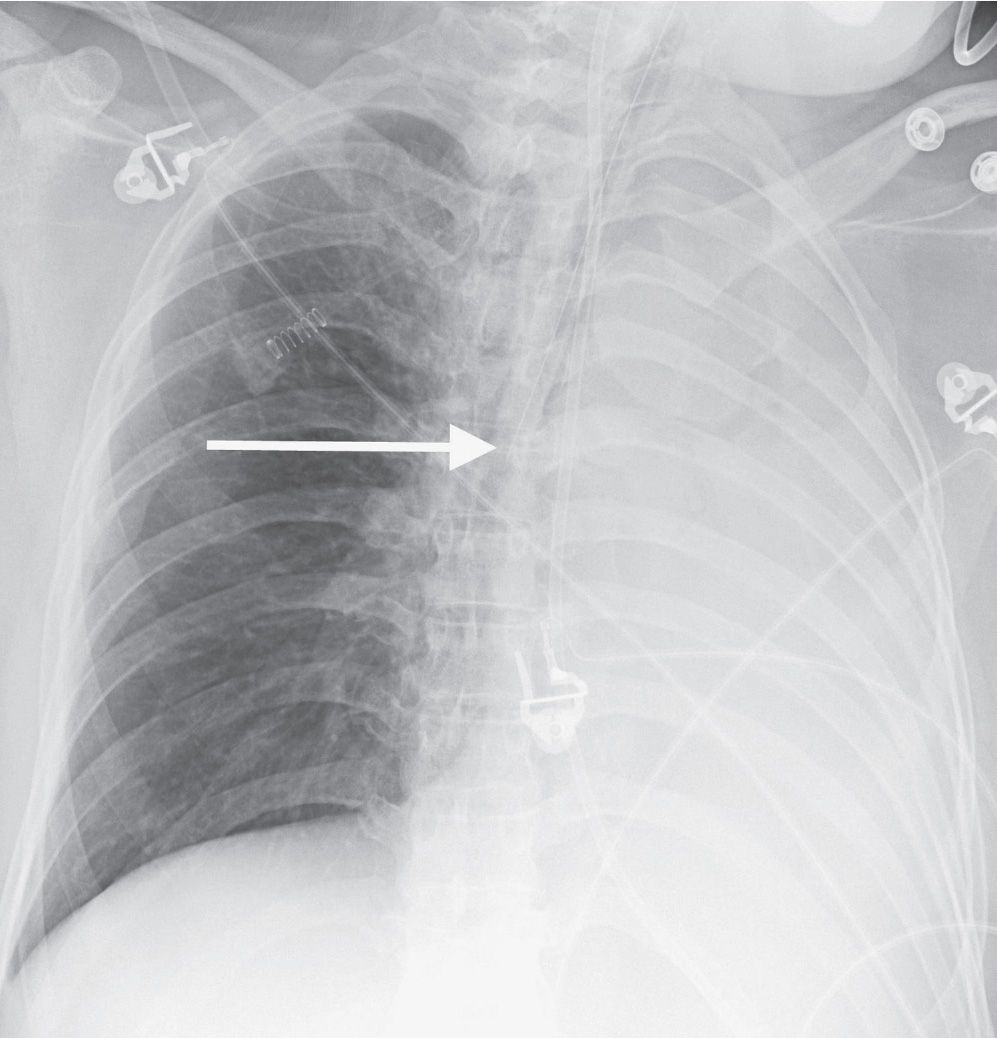
FIG. 11.2 • Left lung collapse. Anteroposterior (AP) chest radiograph shows the tip of the endotracheal tube (arrow) in the right main bronchus, resulting in collapse of the left lung. The left hemithorax is completely opaque and the mediastinum is shifted to the left.
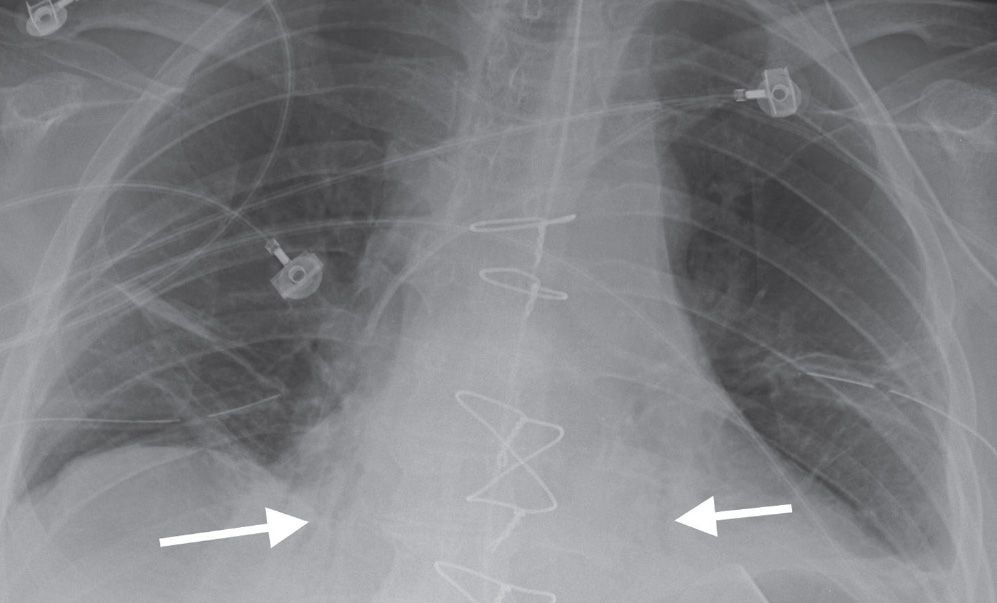
FIG. 11.3 • Bibasilar resorptive atelectasis. AP chest radiograph shows abnormal opacity associated with air bronchograms (arrows) in the lower lobes. There are other areas of linear subsegmental atelectasis more superiorly in the lower lungs.
Compressive atelectasis is caused by any space-occupying lesion of the thorax compressing the lung and forcing air out of the alveoli. Such space-occupying lesions include pleural effusion (including empyema), pneumothorax, pleural tumors, large pulmonary parenchymal masses, large emphysematous bullae, and lobar emphysema (6). Diaphragmatic hernias and abdominal distension from a variety of causes can also compress the lung.
The distinction between compressive and passive atelectasis is not clear-cut. Any space-occupying mass within the thorax can either compress the lung or allow the lung to retract, passively, from the lung’s normal elastic recoil mechanism.
Volume loss resulting from decreased pulmonary compliance as the result of pulmonary fibrosis is termed cicatrization atelectasis. This type of atelectasis is often associated with bronchiectasis in the affected lung. A number of conditions can result in pulmonary fibrosis and cicatrization atelectasis—for example, idiopathic pulmonary fibrosis, sarcoidosis, pneumoconioses, collagen vascular diseases, chronic tuberculous and fungal infections, and radiation fibrosis.
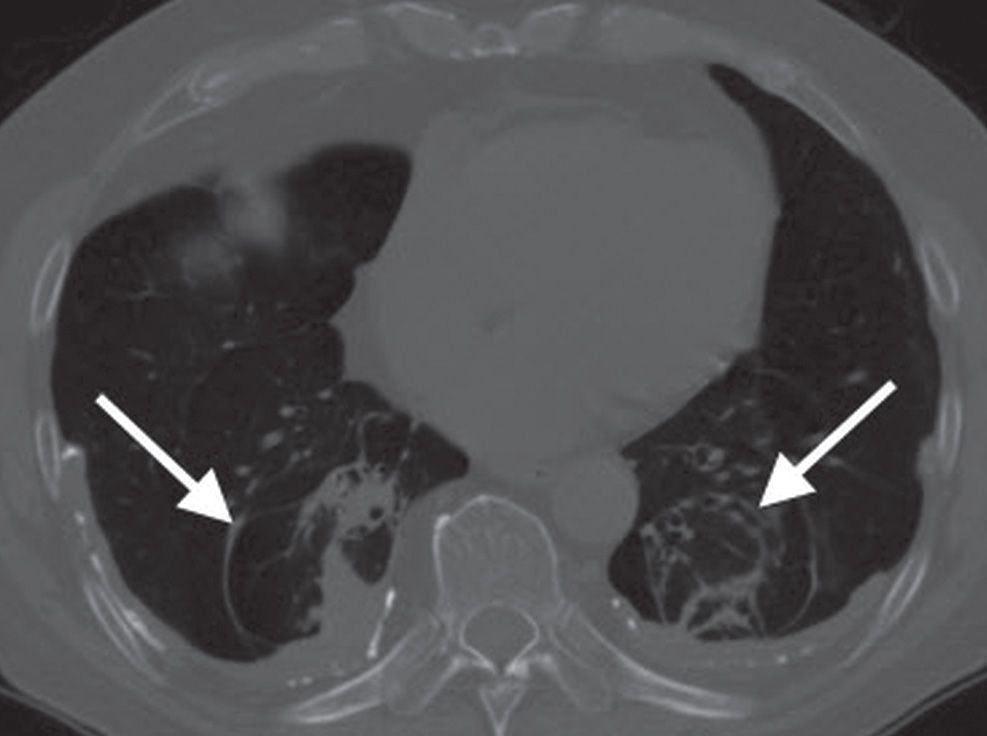
FIG. 11.4 • Rounded atelectasis. CT with bone windowing shows bilateral pleural thickening and calcified pleural plaques, consistent with asbestos-related pleural disease. There are abnormal opacities in both medial lower lobes (rounded atelectasis), abutting the pleural surface, associated with sweeping of vessels and bronchi (arrows) into and around the base of the atelectatic lung.
Normally, the most gravity-dependent portions of lung receive greater perfusion and have less alveolar expansion than non–gravity-dependent portions of lung. These gravity-dependent alterations in alveolar volume are normal but can exacerbate atelectasis in the dependent portions of the lungs, particularly in bedridden hospitalized patients with prolonged shallow breathing. Atelectasis occurring from these forces is termed gravity-dependent atelectasis.
RADIOGRAPHIC SIGNS OF ATELECTASIS
Radiographic signs of atelectasis are outlined in Table 11.1 (5). Opacification of atelectatic lung may not be seen until a considerable loss of volume has occurred. When edema fluid is drawn into the collapsing lung, pneumonia has resulted in atelectasis, or postobstructive pneumonitis is present, there can be abnormal opacification of lung without substantial evidence of volume loss. Elevation of the diaphragm as a sign of volume loss is most easily appreciated when comparison is made to a normal baseline radiograph. A key radiographic feature of upper lobe atelectasis is superior displacement of the hilus. Conversely, in lower lobe atelectasis, the hilus is displaced inferiorly. There is usually no hilar displacement with right middle lobe or lingular atelectasis. Displacement of a fissure follows the movement of the atelectatic lung and is most apparent with atelectasis of an entire lobe. The lung surrounding atelectatic lung often hyperexpands in an attempt to fill in the missing volume of lung; this is referred to as compensatory hyperexpansion or sometimes confusingly referred to as compensatory emphysema. Emphysema is a pathologic condition involving destruction of alveolar walls. Although emphysematous lungs are invariably hyperinflated, hyperexpanded lungs are not invariably emphysematous. If atelectasis affects only one lung, the ribs on that side may come to lie closer together than the ribs on the contralateral normal side. This should be distinguished from the approximation of ribs caused by poor patient positioning at the time the radiograph was obtained.
Table 11.1 RADIOGRAPHIC SIGNS OF ATELECTASIS
Crowding of pulmonary vessels
Crowded air bronchograms
Displacement of interlobar fissures
Abnormal pulmonary opacification
Obscured heart or diaphragm borders
Diaphragm elevation
Displacement of mediastinal structures
Hilar displacement
Compensatory hyperexpansion of surrounding lung
Approximation of ribs
One of the pitfalls in diagnosing left lower lobe atelectasis is artifactual loss of the medial margin of the left hemidiaphragm and abnormal opacity in the left lower lung as a result of incorrect angulation of the X-ray beam. Lordotic angulation of the beam by as little as 10 degrees results in the beam no longer being tangential to the apex of the hemidiaphragm, creating illusory opacity in the left retrocardiac region that may be interpreted as atelectasis or airspace disease in the left lower lobe. Normal-appearing diaphragms and lungs on a lateral view are helpful in making the distinction.
LOBAR ATELECTASIS
In an adult with lobar atelectasis, a central obstructing neoplasm should always be considered as the underlying cause. Lung cancer is relatively uncommon in adults under the age of 40, when bronchial carcinoid tumor is more likely. In children with lobar collapse, an aspirated foreign body or asthma is the usual cause. In postoperative patients, the most common cause is a mucous plug.
With right upper lobe atelectasis, the major and minor fissures move upward (Figs. 11.5 to 11.9); with severe atelectasis, the lung can approximate the mediastinum and lung apex. With complete atelectasis, or collapse of the right upper lobe, the minor fissure parallels the mediastinum and resembles pleural thickening or mediastinal widening. Compensatory hyperexpansion of the middle and right lower lobes leads to outward and upward displacement of the right lower lobe pulmonary artery. Upward angulation of the right mainstem and lower lobe bronchi may be difficult to appreciate on chest radiography. Two radiologic signs are associated with right upper lobe atelectasis. The Golden S sign, or S sign of Golden (see Fig. 2.12), refers to right upper lobe collapse around a central obstructing mass. The juxtaphrenic peak sign (see Fig. 2.16) refers to a small triangular shadow based on the apex of the dome of the involved hemidiaphragm with loss of silhouette of the adjacent hemidiaphragm. On CT, a collapsed right upper lobe appears as a triangular soft tissue density lying against the mediastinum and the anterior chest wall. The border formed by the major fissure posteriorly and the minor fissure laterally is sharp.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree