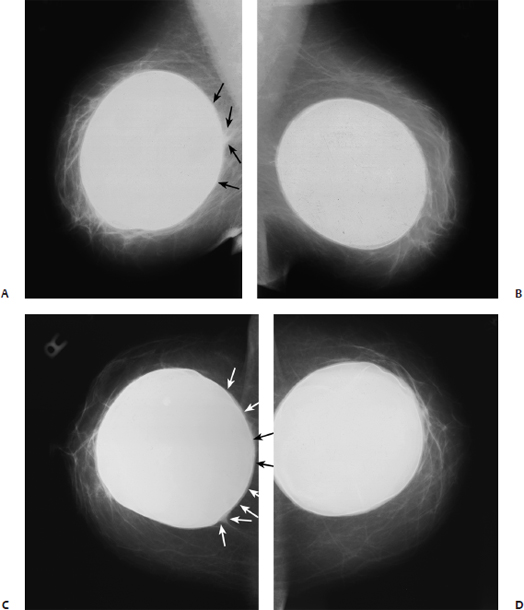
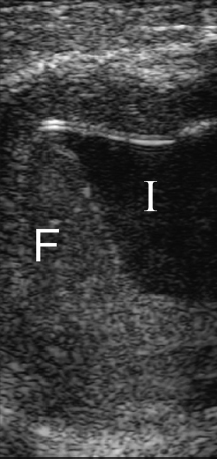
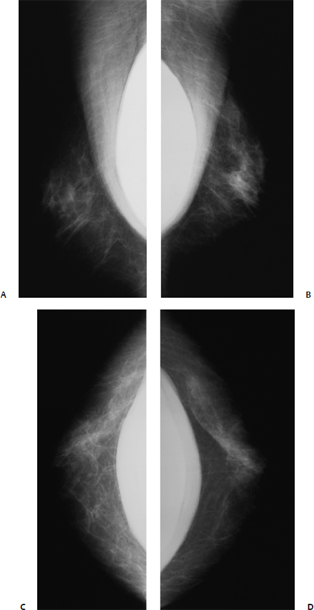
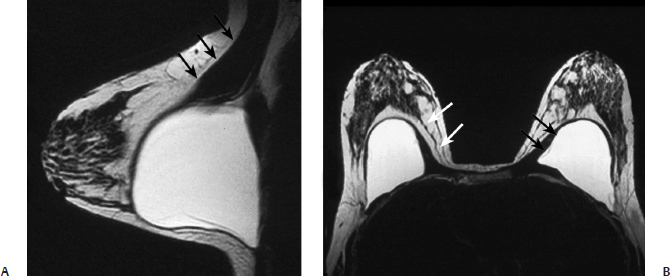
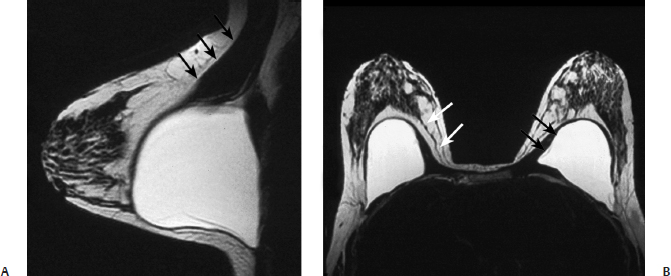
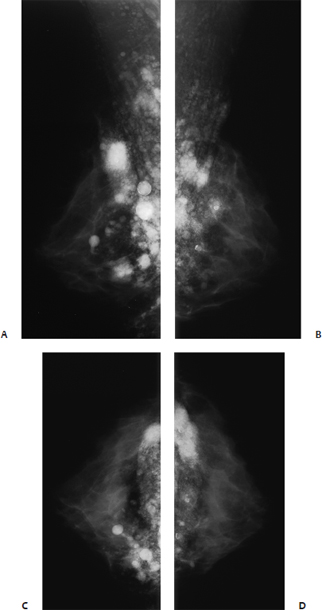
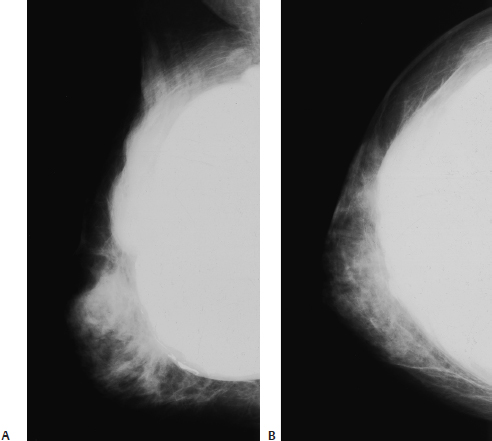
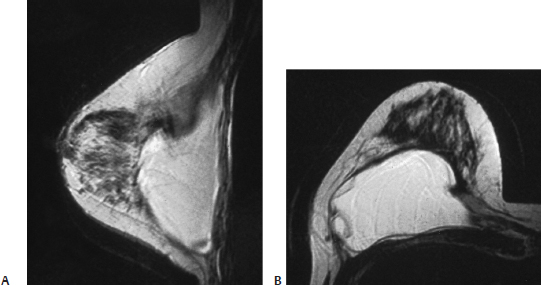
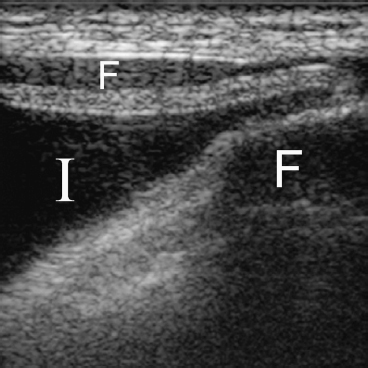
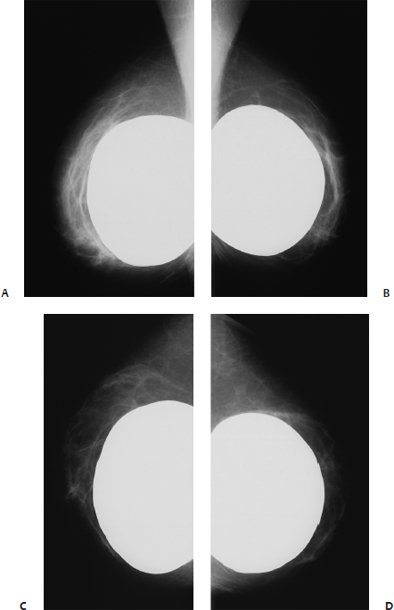
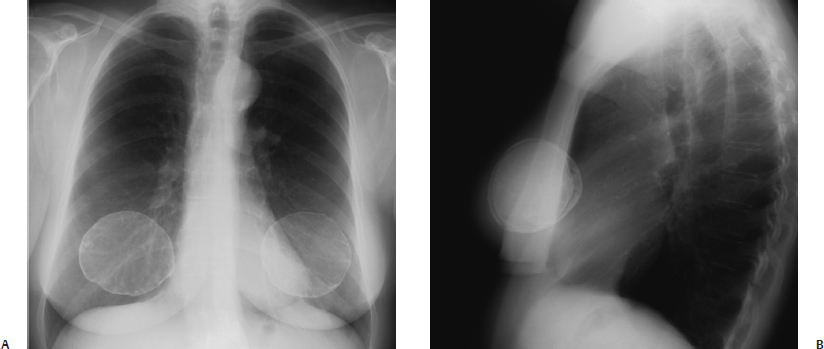
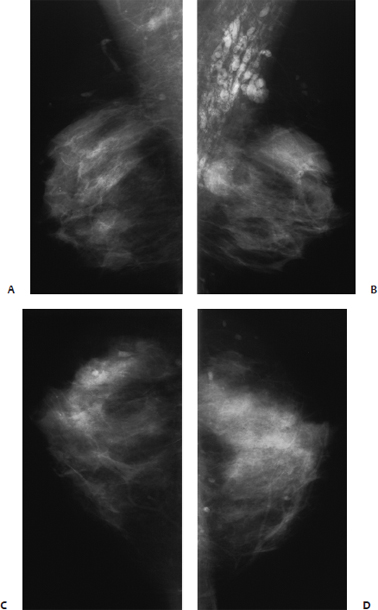
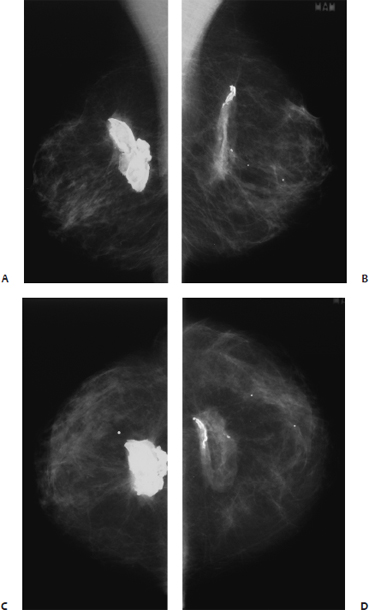
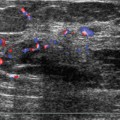
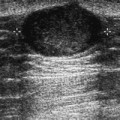
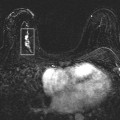
26 Augmentation Mammoplasty A 47-year-old woman presents with right breast pain. She had undergone bilateral breast augmentation 20 years prior to evaluation. • Right breast: swollen and firm • Left breast: normal exam Fig. 26.1 Bilateral subglandular implants are present. There is increased density associated with the posterior deep margin of the right implant (arrows). (A)Right MLO mammogram. (B) Left MLO mammogram. (C) Right CC mammogram. (D)Left CC mammogram. Frequency • 7 MHz Mass (Fig. 26.2) • Echogenicity: hypoechoic • Retrotumoral acoustic appearance: increased acoustic enhancement Fig. 26.2 Right transverse breast sonogram at the 10 o’clock position. The density identified in Fig. 26.1 corresponds to a complex hypoechoic fluid collection (F). The adjacent implant is anechoic (I). • Infected fluid • Implants are generally located either deep to the pectoralis muscle (retropectoral) or within the breast glandular tissue anterior to the pectoralis (subglandular). Subglandular implants generally obscure more breast parenchyma than subpectoral implants. To improve visualization of the parenchyma, Eklund or implant-displaced views should be routinely done in patients with implants. Although we always perform implant-displaced views, these views are not shown in this book unless they provide specific information for the case. • The main complications associated with implants include bleeding or hematoma, infection, capsule contracture, rupture, and silicone granulomas. Steinbach BG, Hardt NS, Abbitt PL, Lanier L, Caffee HH. Breast implants, common complications, and concurrent breast disease. Radiographics 1993;13:95–118 A 47-year-old woman presents for screening mammogram. • Normal exam Fig. 26.3 Bilateral implant views. The subpectoral implants are normal. (A) Right MLO implant view. (B) Left MLO implant view. (C) Right CC implant view. (D) Left CC implant view. • Normal implant • BI-RADS assessment category 1, negative • The advantage of subpectoral implants is that they interfere less with imaging the breast parenchyma and are associated with a lower rate of capsular contraction. Biggs TM, Yarish RS. Augmentation mammaplasty: retro-pectoral versus retromammary implantation. Clin Plast Surg 1988;15:549–555 Vazquez B, Given KS, Houston GC. Breast augmentation: a review of subglandular and submuscular implantation. Aesthetic Plast Surg 1987;11:101–105 A 49-year-old woman presents with chronic pain in her left breast. She received breast augmentation 10 years prior to evaluation. • Normal exam Fig. 26.4 The implants are subpectoral in location and normal in appearance. Pectoralis muscle (arrows). (A) Right breast T2-weighted with water saturation longitudinal MRI. (B) Bilateral breasts T2-weighted with water saturation transverse MRI. Fig. 26.5 Right breast T1-weighted with fat saturation longitudinal MRI. Pectoralis (arrows) is not well identified on this sequence. This sequence is excellent for identifying free silicone due to extracapsular rupture. • Normal implant • BI-RADS assessment category 1, negative • MRI is an excellent method to identify implant rupture. With an MRI T2-weighted series, the fibrous capsule and the implant shell are dark lines, which are normally inseparable except for normal folds of the shell. Silicone and water are bright on T2 series. If water saturation is added to the T2 sequence, then silicone will be brighter than water. This T2 method displays intracapsular rupture well. An alternative technique is an STIR series with water saturation which causes silicone to be bright. The silicone is easily identified either as free silicone or between the layers of the fibrous capsule and the shell of the prosthesis. Middleton MS. Breast implants and soft tissue silicone. In: Stark DD, Bradley WG, eds. Magnetic Resonance Imaging. 3rd ed. St. Louis: Mosby; 1999:335–353 A 66-year-old woman who had silicone injections over 40 years ago presents for annual mammogram. • Bilateral breasts: lobulated pattern in both breasts, which is more prominent in the upper outer quadrants Fig. 26.6 Both breasts exhibit high-density material posteriorly in breast parenchyma, in the lymph nodes, and within the pectoralis muscles. (A) Right MLO mammogram. (B) Left MLO mammogram. (C) Right CC mammogram. (D) Left CC mammogram. • Free silicone • BI-RADS assessment category 1, negative • Silicone was developed in the 1940s and injected into breasts for augmentation in the 1950s and 1960s. Unfortunately, silicone injections resulted in painful hardening of the breast, sloughing of skin, granulomatous hepatitis, and pulmonary embolism. The U. S. Food and Drug Administration banned these injections in 1965. • Mammographically, silicone injections result in high-density round or oval masses and architectural distortion. In the areas containing silicone, neoplasms may be hidden by the silicone masses. Ganott MA, Harris KM, Ilkhanipour ZS, Costa-Greco MA. Augmentation mammoplasty: normal and abnormal findings with mammography and US. Radiographics 1992;12:281–295 Leibman AJ, Sybers R. Mammographic and sonographic findings after silicone injection. Ann Plast Surg 1994;33:412–414 A 66-year-old woman presents with right breast pain and increasing “dimpling” at the edge of her augmentation scar. • Right breast: tenderness and subtle nodularity in the upper outer quadrant • Left breast: normal exam Fig. 26.7 In the upper outer quadrant of the right breast, there is a contour bulge, which is visible only on the MLO view. (A) Right MLO implant mammo-gram. (B) Right CC implant mammogram. Fig. 26.8 (A) Right breast T2-weighted longitudinal MRI. The superior edge of the implant demonstrates a contour deformity that corresponds to the mammographic abnormality. There is no evidence of capsular rupture. (B) Right breast T2-weighted trans-verse MRI. Normal folds extend from the lateral aspect of the implant. • Normal implant • BI-RADS assessment category 1, negative • About half of all implants demonstrate small focal contour deformities without rupture. Wrinkling is more common with saline implants compared with silicone prostheses. The most common location for contour deformities in silicone implants is the superior edge of the implant in the MLO view, as illustrated in this case. • Contour deformities should be differentiated from implant herniation. Both contour deformities and implant folds are normal findings of an intact implant. Herniation is when an intact implant shell is extruded through the fibrous capsule. Capsular herniation is distinguished from a contour bulge by identifying bunching of the implant at the location of the ruptured capsule. Destouet JM, Monsees BS, Oser RF, Nemecek JR, Young VL, Pilgram TK. Screening mammography in 350 women with breast implants: prevalence and findings of implant complications. AJR Am J Roentgenol 1992;159:973–978, discussion 979–981 Ganott MA, Harris KM, Ilkhanipour ZS, Costa-Greco MA. Augmentation mammoplasty: normal and abnormal findings with mammography and US. Radiographics 1992;12:281–295 Middleton MS. Breast implants and soft tissue silicone. In: Stark DD, Bradley WG, eds. Magnetic Resonance Imaging. 3rd ed. St. Louis: Mosby; 1999:335–353 A 57-year-old woman who had a right mastectomy 5 years ago with breast reconstruction using a subpectoral silicone implant is worried about her implant. • Right breast: implant smaller than left breast, otherwise normal • Left breast: normal exam Frequency • 7 MHz (Fig. 26.9) Fig. 26.9 Right transverse breast sonogram. The implant (I) wall is intact, but there is a thin fluid collection (F) outside the implant. • Normal implant • BI-RADS assessment category 1, negative • Small fluid collections of water may form outside the nonruptured implant. These collections are identifiable by sonography or MRI and should not be mistaken for signs of extracapsular rupture. Caskey CI, Hamper UM. Sonographic evaluation of breast implants. In: Sohn C, Blohmer JU, Hamper UM eds. Breast Ultra-sound. New York: Thieme; 1999:143–165 Middleton MS. Breast implants and soft tissue silicone. In: Stark DD, Bradley WG, eds. Magnetic Resonance Imaging. 3rd ed. St. Louis: Mosby; 1999:335–353 Reynolds HE. Evaluation of the augmented breast. Radiol Clin North Am 1995;33:1131–1145 A 66-year-old woman presents with angina. She has had breast implants for over 20 years. • Bilateral breasts: normal exam Fig. 26.10 Bilateral implants exhibit normal contours and shape. (A) Right MLO mammogram. (B) Left MLO mammogram. (C) Right CC mammogram. (D) Left CC mammogram. Fig. 26.11 Chest radiograph demonstrates round densities within the breasts, which represent the patient’s calcified implants. (A) Poster-oanterior (PA) chest radiograph. (B) Lateral chest radiograph. • Calcified implants • BI-RADS assessment category 2, benign finding • Implant calcification is common and generally not associated with a significant clinical problem. About 20% of all types of implants demonstrate at least a small amount of calcification. In a few cases, heavy calcification has been associated with severe capsular contracture, which has been labeled the Krakatau syndrome. This syndrome is named after the famous volcano in Indonesia because when this abnormal implant is removed, the breast exhibits a craterlike depression. Ganott MA, Harris KM, Ilkhanipour ZS, Costa-Greco MA. Augmentation mammoplasty: normal and abnormal findings with mammography and US. Radiographics 1992;12:281–295 Koide T, Katayama H. Calcification in augmentation mammoplasty. Radiology 1979;130:337–340 Steinbach BG, Hardt NS, Abbitt PL. Mammography: breast implants—types, complications, and adjacent breast pathology. Curr Probl Diagn Radiol 1993;22:39–86 Vuursteen PJ. The Krakatau syndrome; a late complication of retroglandular mammary augmentation. Br J Plast Surg 1992;45:34–37 A 64-year-old woman has a history of implant rupture 28 years ago. She removed her implants 15 years ago. • Bilateral breasts: multilobulated but stable Fig. 26.12 There are scattered small, oval, high-density masses in the breast parenchyma and numerous densities in the axilla. (A) Right MLO mammogram. (B) Left MLO mammogram. (C) Right CC mammogram. (D) Left CC mammogram. • Free silicone • BI-RADS assessment category 2, benign finding • Reasons for free silicone in the breast include silicone injections, ruptured implant, and escape of silicone from an intact implant elastomer shell (gel bleed). The elastomer shell is a semiporous membrane that allows silicone to flow into the surrounding tissues without rupture of the shell. The most common migration of free silicone is to the upper outer or upper medial soft tissues. Rarely, silicone will migrate to the breast or axilla from a distal injection site, such as the arm. Hayes MK, Gold RH, Bassett LW. Mammographic findings after the removal of breast implants. AJR Am J Roentgenol 1993;160:487–490 Middleton MS. Magnetic resonance evaluation of breast implants and soft-tissue silicone. Top Magn Reson Imaging 1998;9:92–137 Roux SP, Bertucci GM, Ibarra JA, Blatt G, Ashworth CR. Uni-lateral axillary adenopathy secondary to a silicone wrist implant: report of a case detected at screening mammography. Radiology 1996;198:345–346 A 60-year-old woman who has had removal of bilateral implants presents for her annual mammogram. • Normal exam Calcifications (Fig. 26.13) • Type: dystrophic Fig. 26.13 There are large dystrophic calcifications and scarring in the areas of the patient’s previous implants. (A) Right MLO mammogram. (B) Left MLO mammogram. (C) Right CC mammo-gram. (D) Left CC mammogram. • Scar
Case 26.1: Subglandular Implants—Infected Fluid
Case History
Physical Examination
Mammogram (Fig. 26.1)
Ultrasound
Pathology
Management
• BI-RADS assessment category 2, benign finding
Pearls and Pitfalls
Suggested Reading
Case 26.2: Subpectoral Implants
Case History
Physical Examination
Mammogram (Fig. 26.3)
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 26.3: Subpectoral Implants
Case History
Physical Examination
Other Modalities: MRI (Figs. 26.4 and 26.5)
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 26.4: Silicone Injections
Case History
Physical Examination
Mammogram (Fig. 26.6)
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 26.5: Normal Findings—Bulge
Case History
Physical Examination
Mammogram (Fig. 26.7)
Other Modalities: MRI (Fig. 26.8)
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 26.6: Normal Findings—Fluid
Case History
Physical Examination
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 26.7: Implant Calcifications
Case History
Physical Examination
Mammogram (Fig. 26.10)
Other Modalities: Chest Radiography (Fig. 26.11)
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 26.8: Changes after Implant Renewal—Residual Silicone
Case History
Physical Examination
Mammogram (Fig. 26.12)
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 26.9: Changes after Implant Renewal–Calcifications
Case History
Physical Examination
Mammogram
Pathology
Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree