Major criteria
Minor criteria
Regional RV akinesia, dyskinesia, or aneurysm and 1 of the following (end-diastole):
Regional RV akinesia or dyskinesia and 1 of the following (end-diastole):
PLAX RV OT >32 mm [corrected for body size (PLAX/BSA) >19 mm/m2]
PLAX RV OT ≥29 to <32 mm [corrected for body size (PLAX/BSA) ≥16 to <19 mm/m2]
PSAX RV OT ≥36 mm [corrected for body size (PSAX/BSA) ≥21 mm/m2]
PSAX RV OT ≥32 to <36 mm [corrected for body size (PSAX/BSA) ≥18 to <21 mm/m2]
Or RV fractional area change ≤33 %
Or RV fractional area change >33 to ≤40 %
15.3 Right Ventricular Dimensions
In ARVC, an enlarged RV is a common finding. RV outflow and inflow can be involved, but a short-axis dimension of >30 mm of the RV outflow tract (OT) had the highest sensitivity and specificity (89 and 86 %, respectively) for ARVC diagnosis) [3], and therefore RV OT measurement has become an integral part of the new diagnostic criteria. RV OT dimensions can be measured either in the parasternal long-axis view or in parasternal short-axis view (Figs. 15.1 and 15.2, Clip 15.1a, b). Measurements of RV basal and midcavity minor dimensions, longitudinal dimension, and end-diastolic and end-systolic areas (all obtained from a four-chamber apical view focused on the RV) are recommended by the RV echocardiographic guidelines [4], but such measurements correlate poorly with ARVC [3] and therefore are not ordinarily used for diagnostic assessment in ARVC patients.
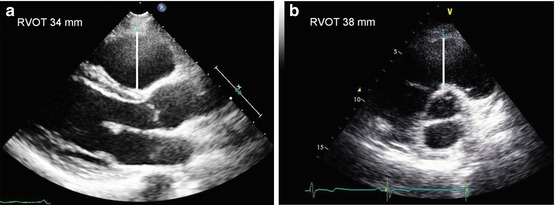

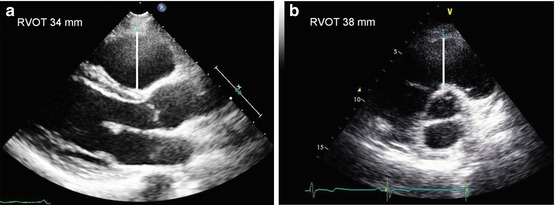
Fig. 15.1
Right ventricular outflow tract (RVOT) dimensions measured in parasternal long-axis view (34 mm) (a) and in parasternal short-axis view (38 mm) (b) in a patient with arrhythmogenic RV cardiomyopathy

Fig. 15.2
Patient with arrhythmogenic right ventricular (RV) cardiomyopathy and severely dilated RV. The RV outflow tract diameter measured in parasternal short axis view is 55.8 mm
15.4 Right Ventricular Systolic Function
Quantitative echocardiographic assessment of RV systolic function is problematic due to its complex geometry, which precludes imaging the inflow and outflow tracts in a single 2D plane and lack of standard methods for assessing RV volumes. Nonetheless, 2D echocardiography represents the first-line imaging technique available for screening patients with suspected ARVC and is of utmost importance when studying these patients, as cardiac magnetic resonance (CMR) is not highly available in most centers. CMR is considered the gold-standard technique for thorough evaluation of RV dimensions and function; however, its use is mainly reserved for equivocal cases (Chap. 22).
RV fractional area change (FAC) is one of the most commonly used 2D echocardiographic method to assess RV systolic function, as it correlates well with RV ejection fraction (EF) determined by CMR volumetric analysis and is superior to other 2D parameters [5, 6]. RV FAC is obtained in the four-chamber apical view (focused on the RV) by tracing the RV endocardium both in end diastole and end-systole from the annulus, along the free wall to the apex, and then back to the annulus, along the interventricular septum. Care must be taken to trace the free wall beneath the trabeculations. Impaired RV function, defined as RV FAC < 33 %, has been described in approximately two thirds of patients with ARVC and represents an important diagnostic parameter (Fig. 15.3, Clip 15.2a) [7, 8].
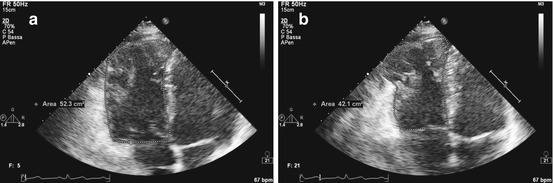
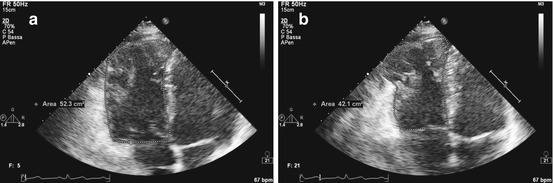
Fig. 15.3
Right ventricular (RV) fractional area change measurement from an apical four-chamber view in a patient with arrhythmogenic RV cardiomyopathy with severe RV dilation and pronounced aneurysms in the RV apex. RV end-diastolic area is 52.3 cmq (a), end-systolic area is 42.1 cmq (b), and fractional area change is 19 %
15.5 Right Ventricular Regional Assessment
RV localized WMA are a landmark of ARVC and reflect the patchy infiltration and substitution of normal myocardium with fibrofatty tissue. In the Revised Diagnostic Criteria of ARVC [2], the presence of localized akinetic, dyskinetic, or aneurysmal RV segments represents a major diagnostic criterion, emphasizing the importance of their recognition. Of note, with respect to the original 1994 International Task Force Criteria [9], hypokinesis is no longer considered a morphological diagnostic criteria due to its low specificity.
The typical echocardiographic appearance consists of localized aneurysmal bulges of the RV wall classically described in the “triangle of dysplasia,” namely the RV OT, apex, and basal subtricuspid area (Fig. 15.3 and Clips 15.2a, b, 15.3a–c, and 15.4a, b) [10]. However, in clinical practice, regional WMA may be found in all RV segments; therefore a complete assessment of RV using conventional and off-axis views must be conducted [11]. Parasternal RV inflow and outflow views are particularly useful for exploring the anterior wall of the RV OT and inferior and anterior walls of the RV inflow tract (Clip 15.5). RV free wall is better assessed from the RV-focused four- and two-chamber apical views and the four-chamber subcostal view.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree