Characteristics
Left ventricle
Dimensions: globally dilated (LV end-diastolic diameter >117 % predicted value corrected for age and BSA)
Wall thickness: normal or mildly increased with eccentric hypertrophy
Geometry: increased sphericity
Systolic function: reduced (LV EF <45 % and/or fractional shortening <25 %) with diffuse hypokinesis
Diastolic function: frequently impaired; RFP
Dyssynchrony: present, especially if severe LV dysfunction and LBBB
Right ventricle
In case of biventricular involvement, RV dilation and dysfunction are possible
Atria
Bi-atrial dilation is frequent
Mitral valve
Functional MR is frequent and due to annular dilation and apical tethering
Tricuspid valve
Functional TR is frequent, with pulmonary hypertension and RV dilation and/or dysfunction
5.2 Left Ventricular Dimensions, Geometry, and Systolic Function
The LV is typically globally dilated and dysfunctioning, with diffuse hypokinesis (Clip 5.1). LV dilation may precede LV dysfunction in some cases [1]. It is therefore crucial to precisely assess LV dimensions and index the measurements according to body surface area (BSA). The standard measures include LV end-diastolic diameter, assessed from the parasternal long-axis view (Clip 5.2, diagnostic criteria for DCM is LV end-diastolic diameter >117 % predicted value corrected for age and BSA), and LV volumes from apical four- and two-chamber views [1].
Patients with hypokinetic LV without severe dilation (i.e., LV end-diastolic diameter within 15 % of normal values) are defined as having mildly dilated cardiomyopathy (CMP) [3, 4] (Clip 5.3) and are considered to be within the spectrum of DCM. In advanced cases with severe LV dilation and systolic dysfunction, the LV geometry is altered, becoming more spherical (Figs. 5.1 and 5.2; Clips 5.4a, 5.4b, and 5.5). The so-called LV remodeling is characterized by an increased short-axis/long-axis ratio (sphericity index) [5]. This geometric abnormality contributes to LV systolic dysfunction by increasing LV wall stress and reducing contractility, and it can worsen functional MR.
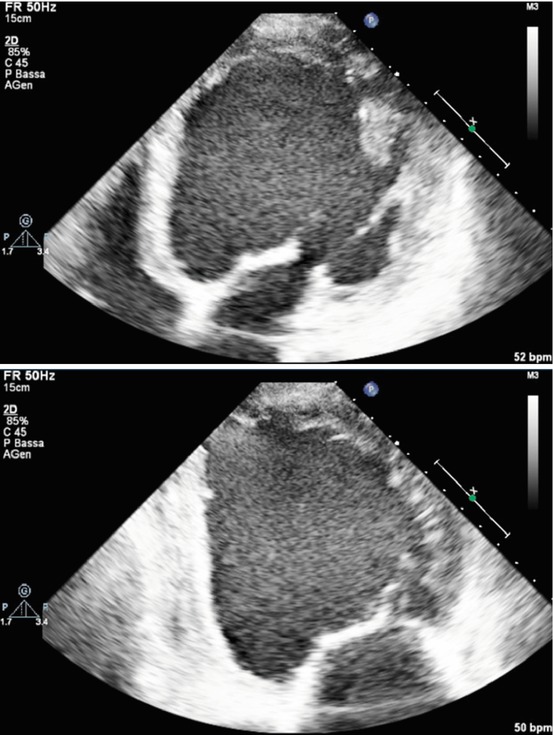
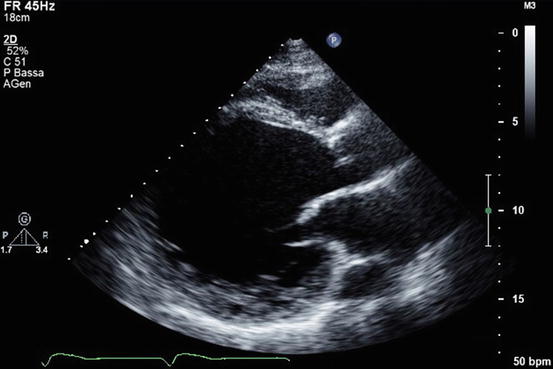
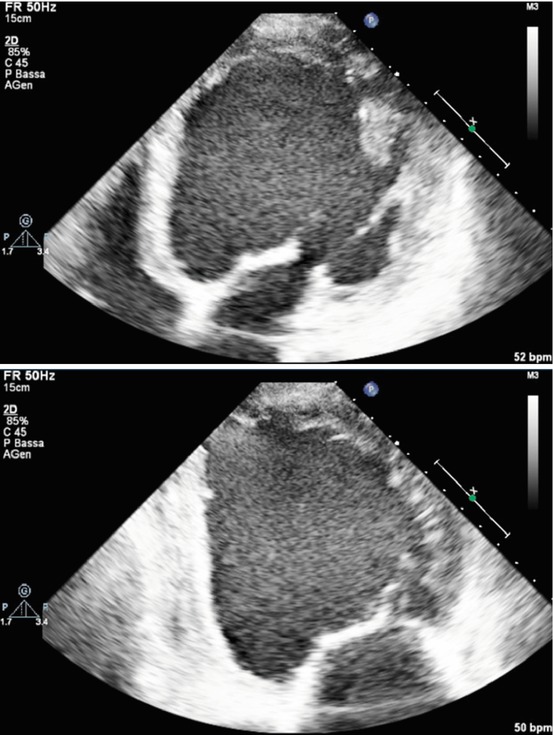
Fig. 5.1
Apical four-chamber (upper panel) and two-chamber (lower panel) views – end-diastolic frames – of a patient with advanced dilated cardiomyopathy with severe left ventricular (LV) dilation and systolic dysfunction and LV remodeling, resulting in a spherical LV geometry
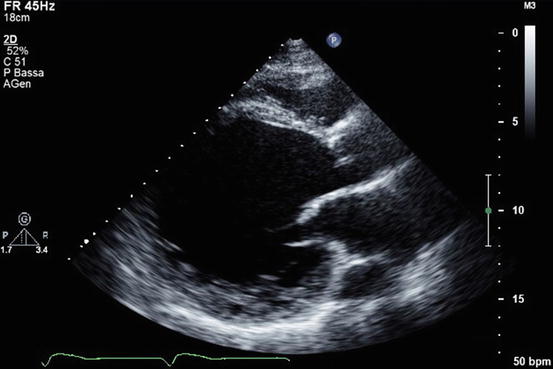
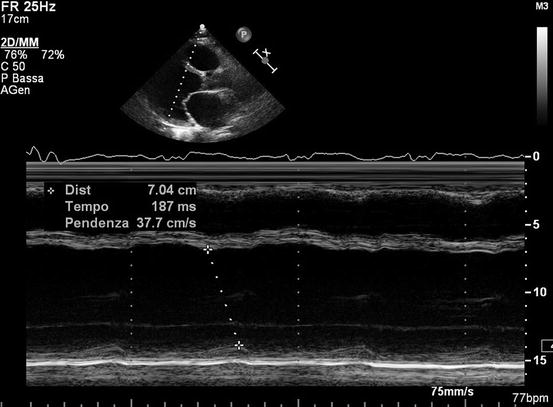
Fig. 5.2
Parasternal long-axis view showing a severely remodeled left ventricle
LV wall thickness is usually normal or only mildly increased in DCM. Severe LV hypertrophy excludes the diagnosis of DCM and suggests the presence of other types of CMP, such as hypertrophic, infiltrative, or hypertensive CMP with hypokinetic evolution (Table 5.2). However, even in the presence of normal LV wall thickness, LV mass is often increased due to LV dilation (eccentric hypertrophy with increase in volume/mass ratio and radius/thickness ratio) [6].
Table 5.2
Echocardiographic features useful in the differential diagnosis of dilated cardiomyopathy
LVH | WMA/aneurysm | RV dysfunction | Mild LV dilatation | |
|---|---|---|---|---|
Hypertensive CMP | + | − | − | + |
End-stage HCM | + | − | ± | + |
Myocarditis | ± | + | ± | + |
ARVC (bi-ventricular) | − | + | + | + |
Ischemic CMP | − | + | ± | − |
Tako-tsubo CMP | − | + | ± | ± |
TIC | − | − | ± | + |
Infiltrative/storage CMP | + | − | ± | + |
An essential echocardiographic feature for the diagnosis of DCM is global LV systolic dysfunction, i.e., a significantly depressed LV ejection fraction (EF) (usual diagnostic cutoff <45 %) [1]. Accurate measurement of LV systolic function is pivotal in DCM patients given the fact that many therapeutic decisions rely on this parameter, such as the indication for implantable cardioverter defibrillator (ICD) or cardiac resynchronization therapy (CRT). In case of bad image quality, when <80 % of the endocardial border is visualized (or more than two contiguous segments are not visualized), the use of contrast agents is indicated for LV opacification and better evaluation of LV volumes and EF (Clip 5.6) [7].
Another useful index for LV function assessment in this population is the myocardial performance index, or Tei index – i.e., the ratio of the LV isovolumic contraction + relaxation times and ejection time. This is a Doppler parameter that provides a global evaluation of systolic and diastolic function of both ventricles [8]. Furthermore, stroke volume (and cardiac output) can be derived either from LV end-diastolic and end-systolic volumes or from the area of the LV outflow tract (OT) × OT velocity time integral from pulsed-wave (PW) Doppler recordings. This parameter can be useful in selected patients to noninvasively identify a low output state. Finally, dP/dt is an additional index of systolic function that measures the rise in intraventricular pressure during early systole in patients with MR. It appears less dependent on loading conditions than LV EF. However, its usefulness in DCM is not yet defined.
Considering regional wall motion assessment, DCM is usually characterized by global hypokinesis. Regional wall motion abnormalities (WMA) with coronary artery distribution suggest the presence of coronary artery disease (Table 5.2). However, in some DCM cases, regional wall motion is heterogeneous, with akinetic or dyskinetic segments (more frequently anterior or apical) and better contractility usually in the posterior and lateral segments [9]. In rare cases, the presence of LV aneurysm can be found, generally in association with global hypokinesis and significant LV dysfunction. These forms are called idiopathic LV aneurysms and are considered to be within the spectrum of DCM, although without a clear etiopathogenic explanation (Clips 5.7a and 5.7b) [10]. The possibility of previous myocarditis or left-dominant arrhythmogenic CMP must be considered (Table 5.2).
In the presence of severe LV dilation and dysfunction, there is a high probability of spontaneous echocontrast and intracavitary thrombi formation, with risk of embolization (Clips 5.8a and 5.8b). Contrast agents can be useful in this setting, particularly in differentiating thrombi from artefacts.
Finally, in muscular dystrophies associated with DCM, such as Duchenne and Becker types, echocardiography can be normal in the initial phase of the disease, or there can be regional WMA, typically located in the posterolateral and posterobasal regions. With disease progression and fibrosis extension, LV dilation and dysfunction become manifest and can be associated with MR owing to involvement of the posterior papillary muscle. An early diagnosis of cardiac involvement has been reported using dobutamine stress echocardiography [11], tissue Doppler imaging (TDI) [12], and tissue characterization [13].
5.3 Left Ventricular Diastolic Function
LV diastolic dysfunction is often present in DCM. Evaluation of diastolic function is complex as it is influenced by many variables [14]. It is therefore important to consider various indices of diastolic function.
It is well known that diastolic dysfunction stages begin with impaired relaxation at Doppler interrogation of transmitral flow and progress to a restrictive filling pattern (RFP) that denotes high LV filling pressure and LV stiffness (Fig. 5.3) [15]. In DCM, high diastolic pressure and LV stiffness may be due to several factors [16], such as structural myocardial alterations (LV fibrosis), LV cavity dilatation, and ventricular interdependence, with pericardial restraint in case of biventricular involvement and biatrial dilatation [17]. The pseudonormal pattern is an intermediate stage that can represent a worsening from impaired relaxation or an improvement of reversible RFP after optimal treatment [14]. It can be identified by the response of the mitral flow pattern to Valsalva maneuver [18] and the pattern of the pulmonary venous Doppler curve [14, 19].
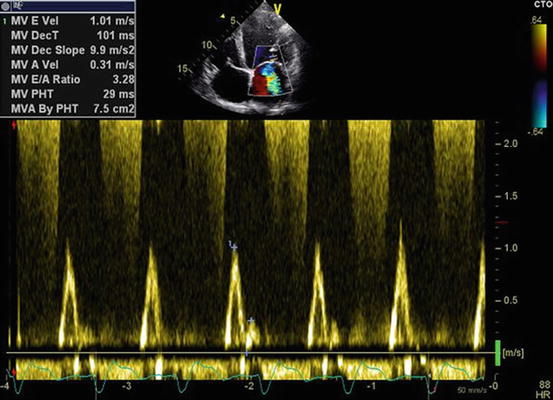
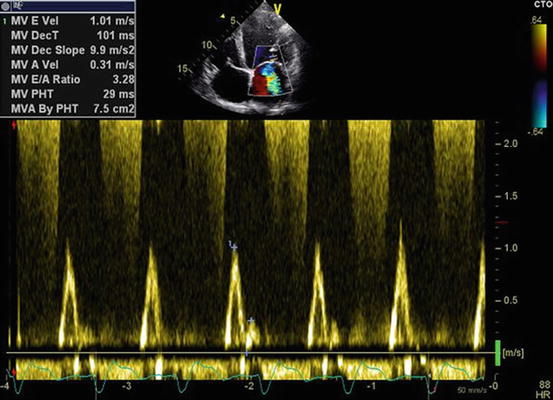
Fig. 5.3
Pulsed-wave Doppler interrogation of transmitral flow showing a restrictive filling pattern (E-wave velocity 1 m/s, A-wave velocity 0.31 m/s, E/A ratio 3.3, E-wave deceleration time 101 ms)
5.4 Left Ventricular Dyssynchrony
Evaluation of LV mechanical dyssynchrony in DCM patients with heart failure (HF), severe LV dysfunction, and left bundle branch block (LBBB) has been widely studied and principally applied to identify potential responders to CRT (Clip 5.9). LV dyssynchrony (i.e., uncoordinated LV wall contraction) results in further reduction of LV function and other negative consequences, such as worsening of functional MR. Therefore, several echocardiographic indices of intraventricular dyssynchrony have been studied, the earliest based on 2D echocardiography and M-mode imaging [20].
Visual estimation of the rocking motion of the apex (apical rocking) is a simple LV mechanical dyssynchrony marker that combines both functional and temporal myocardial inhomogeneities [21]. Moreover, septal flash, defined as an abnormal septal motion on M-mode imaging traces that occurs during the preejection period, has been used as a sign of LBBB-induced dyssynchrony [22]. Another simple M-mode index of LV dyssynchrony is the septal to posterior wall motion delay, which is measured in the parasternal long-axis view at the papillary muscle level (Fig. 5.4).