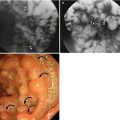
Fig. 3.1
A papilloma in a 63-year-old man. On esophagography (a), a large esophageal diverticulum with internal filling defect (arrows) is noted, and near the diverticular neck, there is a persistent mucosal lesion (arrowheads). On CT scan (b), the mucosal lesion is not visualized near the diverticulum. On endoscopy, a wartlike excrescence (black arrows) is found near the neck of the diverticulum (c), and there is a bezoar (white arrows) in the diverticulum (d)
3.3.2 Esophageal Hyperplastic Polyp
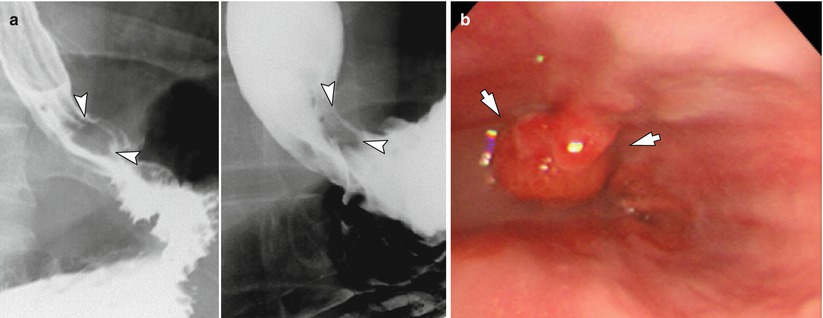
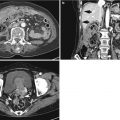
Fig. 3.2
A hyperplastic polyp in a 45-year-old man. A nodule with relatively smooth contour (arrowheads) is persistently seen in the distal esophagus, near the gastroesophageal (GE) junction on esophagography (a). On EGD (b), an approximately 2.5 cm polyp (arrows) is observed, and the patient underwent endoscopic mucosal resection. Histology specimen revealed granulation tissue with ulceration and foveolar epithelial hyperplasia, which was suggestive of hyperplastic polyp
3.3.3 Esophageal Submucosal Polyp
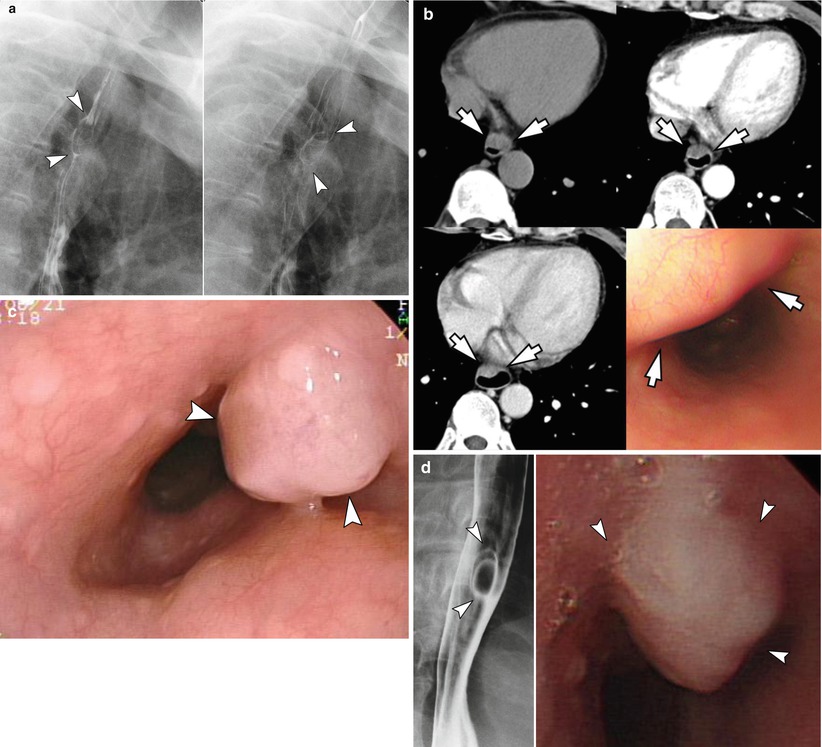
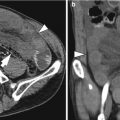
Fig. 3.3
An esophageal submucosal polyp in a 70-year-old man. On esophagography (a) and CT (b), an approximately 1.8 cm luminal protruding lesion is noted in the upper esophagus (arrowheads). No mucosal lesion is demonstrated. On endoscopy (c), a Yamada type III polyp with slightly pale mucosa is found (arrowheads). On biopsy, the specimen shows acanthotic squamous epithelium. On follow-up esophagography after 5 years and endoscopy after 7 years (d), the lesion does not show significant change (arrowheads)
3.3.4 Esophageal Leiomyoma: EUS, Volume Rendering Image of 3D CT Esophagography
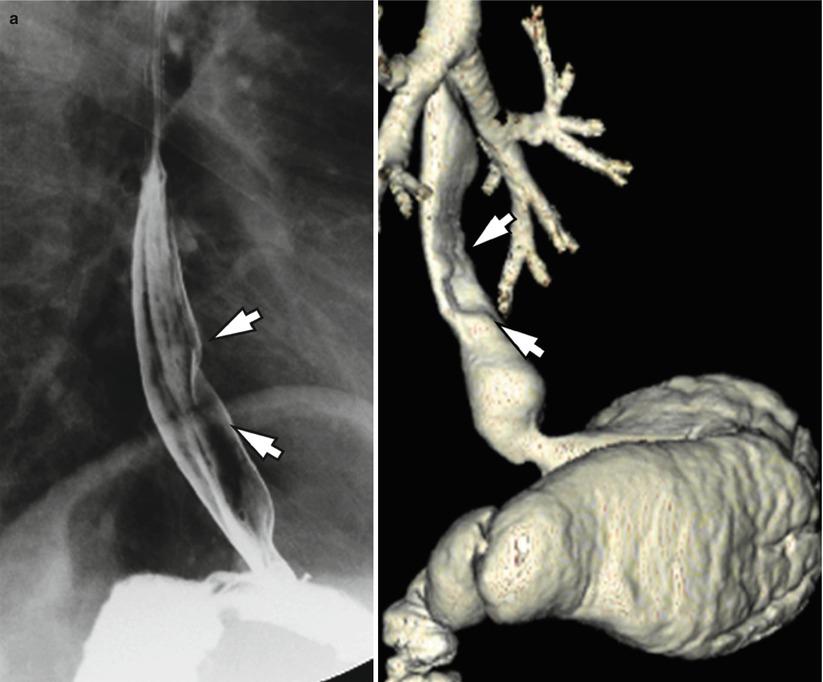
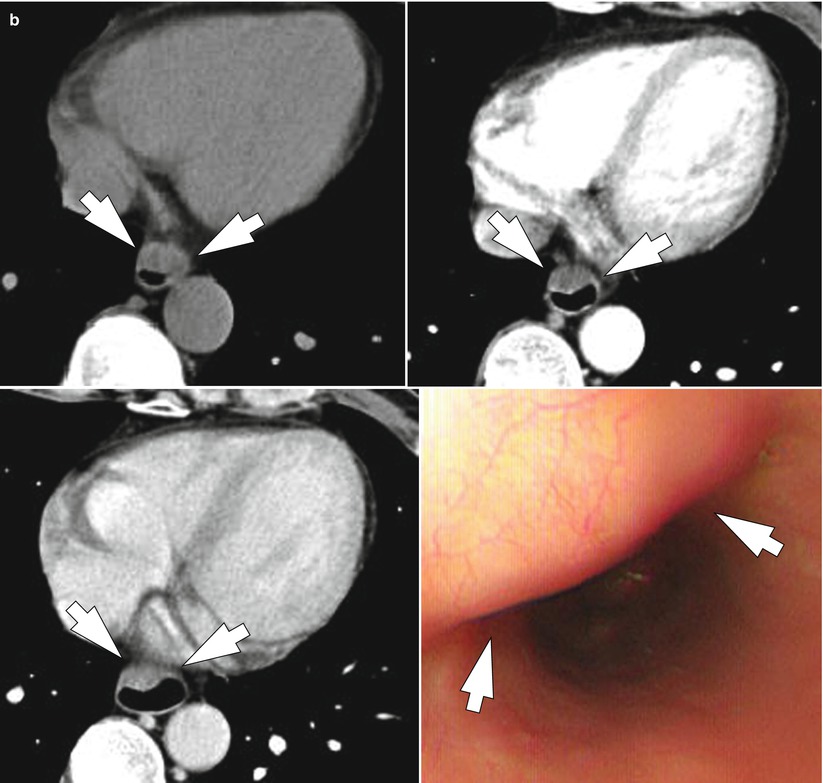
Fig. 3.4
An esophageal leiomyoma in a 57-year-old man. On esophagography (a, left) and three-dimensional (3D) CT esophagography (a, right), there is an eccentric filling defect in the lower esophagus. On CT scan (b), the mass shows gradual enhancement, but hypovascularity on precontrast phase (top left), arterial phase (top right), and portal venous phase (bottom left). On EGD (bottom right), a smooth contoured mass without mucosal change is noted (arrows). The mass was surgically confirmed as a leiomyoma
3.3.5 Esophageal Duplication Cyst
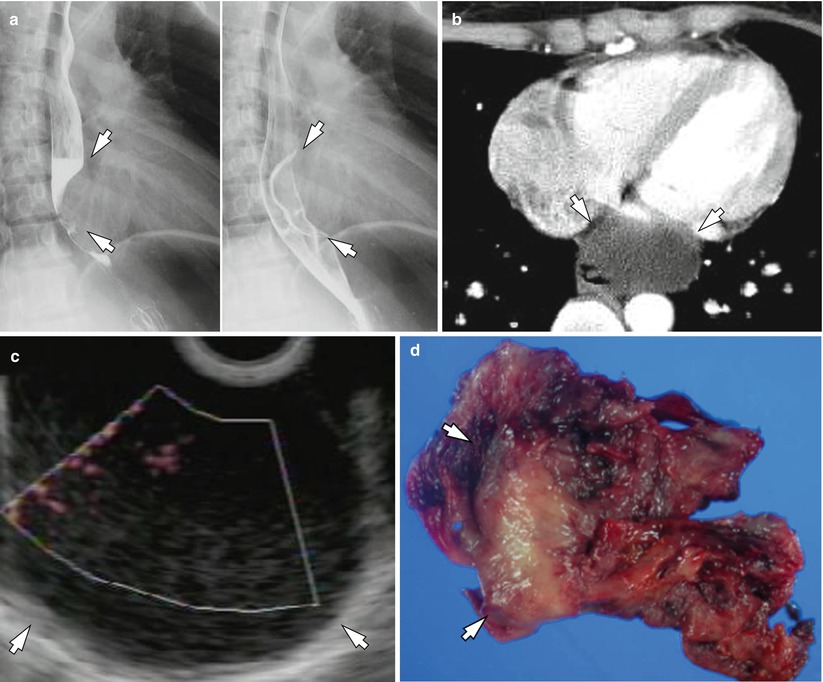
Fig. 3.5
A duplication cyst in a 39-year-old woman. An approximately 3 cm filling defect with smooth margin (arrows) is observed in the lower esophagus on esophagography (a). There is no mucosal lesion on esophagography. On CT scan (b), 3 cm low-attenuating mass is seen in the posterior mediastinum. Hounsfield unit (HU) of the mass is around 10~15 which is suggestive of its cystic nature. On EUS (c), an approximately 3 cm hypoechoic mass is observed. After resection (d), the mass was confirmed as a duplication cyst
3.3.6 Esophageal Retention Cyst
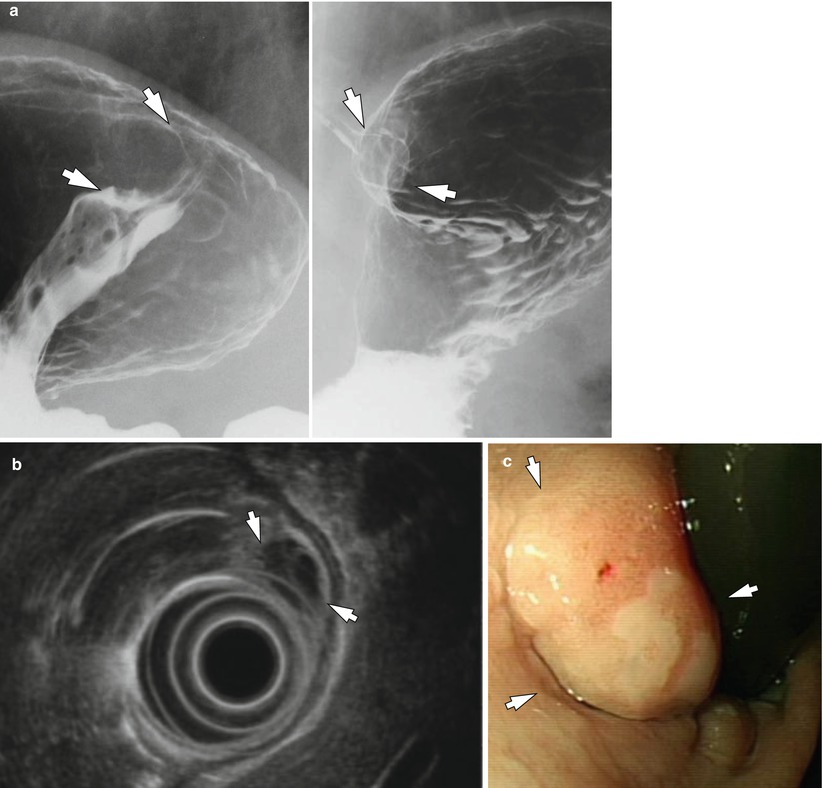
Fig. 3.6
A retention cyst in a 72-year-old man. On UGIS (a), approximately 1.5 cm polypoid lesion is seen near GE junction (arrows). The mass shows smooth margin and hypoechogenicity on EUS (b, arrows) and no mucosal lesion is seen on EGD (c). The mass was histologically confirmed as a retention cyst after resection
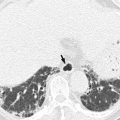
3.3.7 Esophageal Cavernous Hemangioma
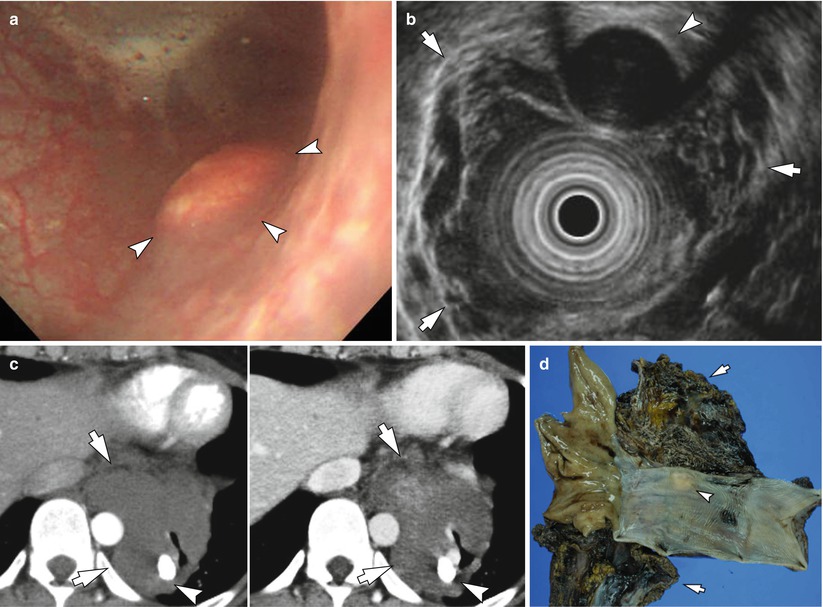
Fig. 3.7
An esophageal hemangioma in a 37-year-old woman. On EGD (a), there is a small broad-based submucosal tumor (arrowheads). On EUS (b), the lesion shows hypoechogenicity (arrowhead) and diffuse esophageal wall thickening is suspected (arrows). Diffuse wall thickening of distal esophagus is seen on chest CT (c): it shows gradual enhancement on dynamic phases (arrows) and small calcification (arrowhead) is seen, which is thought to be a phlebolith. After resection, the specimen (d) shows approximately 9 × 6 × 4 cm soft tissue with spongelike appearance including hemorrhage (arrows). The soft tissue surrounded the esophagus was confirmed as a cavernous hemangioma involving submucosa, proper muscle, and adventitia. A small yellowish nodule (arrowhead) was confirmed as a calcified fibrotic nodule with heterotopic ossification
3.3.8 Esophageal Granular Cell Tumor
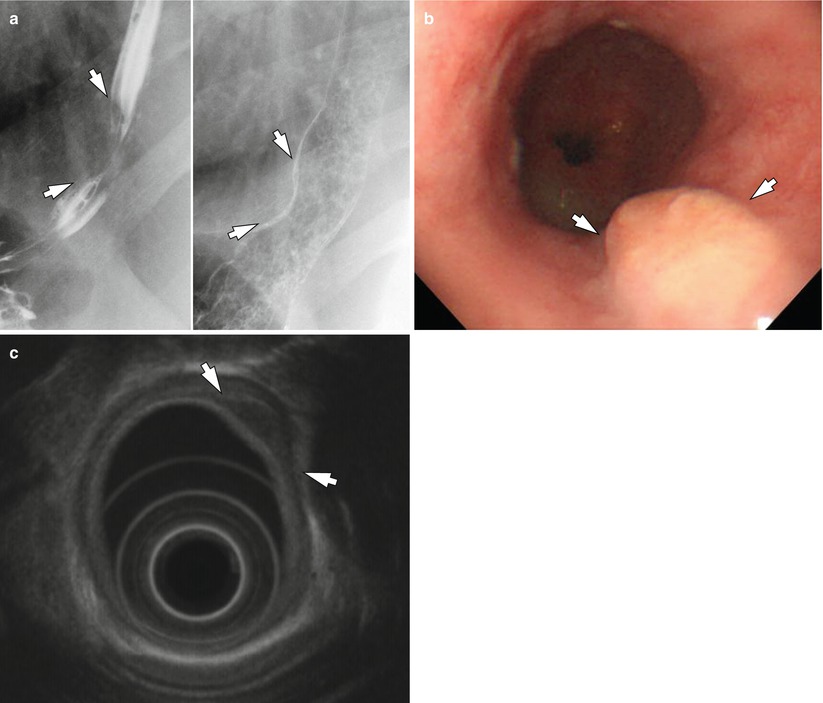
Fig. 3.8
A granular cell tumor in a 50-year-old woman. On esophagography (a), there is an eccentric esophageal wall deformity without mucosal lesion (arrows). EGD (b) reveals a broad-based polyp without mucosal abnormality (arrows). On EUS (c), the tumor arises from submucosal layer (arrows). After resection, the tumor was proven to be a granular cell tumor
3.3.9 Esophageal Gastrointestinal Tumor (GIST) with Low Malignant Potential
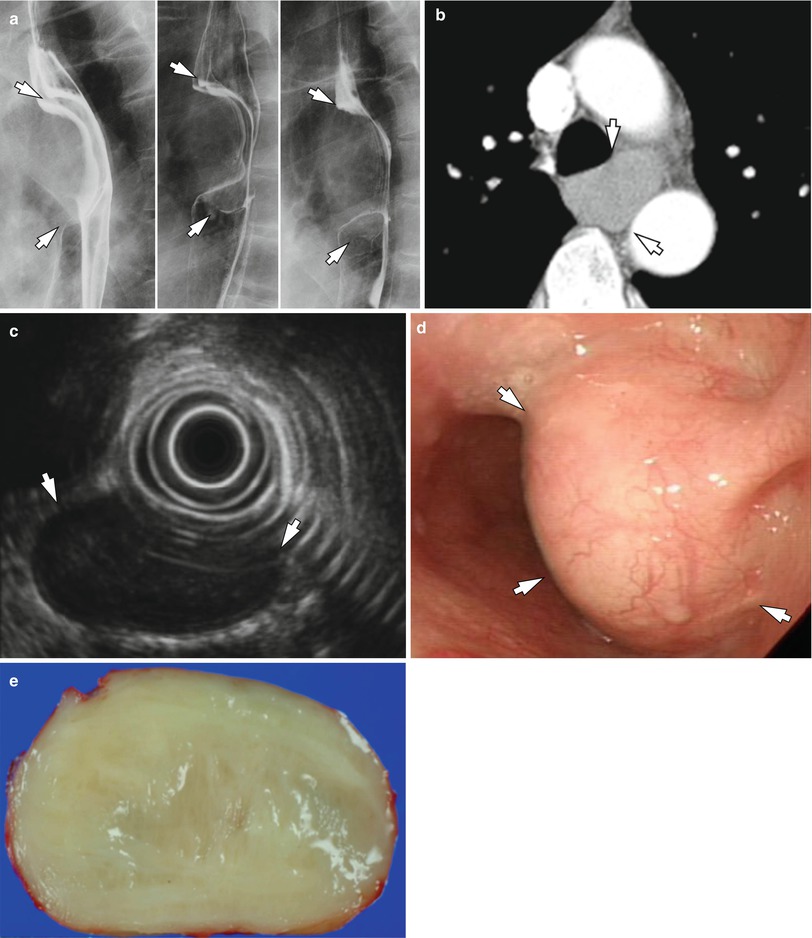
Fig. 3.9
An esophageal gastrointestinal stromal tumor (GIST) in a 54-year-old man. A smooth contour deformity (arrows) of the esophagus is noted on esophagography (a): the mucosa is intact. On CT scan (b), the approximately 3 cm hypovascular tumor is seen in the esophagus, just below the aortic arch (arrows). On EUS, an approximately 3 cm submucosal hypoechoic tumor (arrows) is found (c) and there is no mucosal abnormality on EGD (d). A yellowish round tumor (e) was resected and it was confirmed as a GIST which had low malignant potential
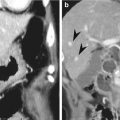
3.3.10 Esophageal Malignant GIST
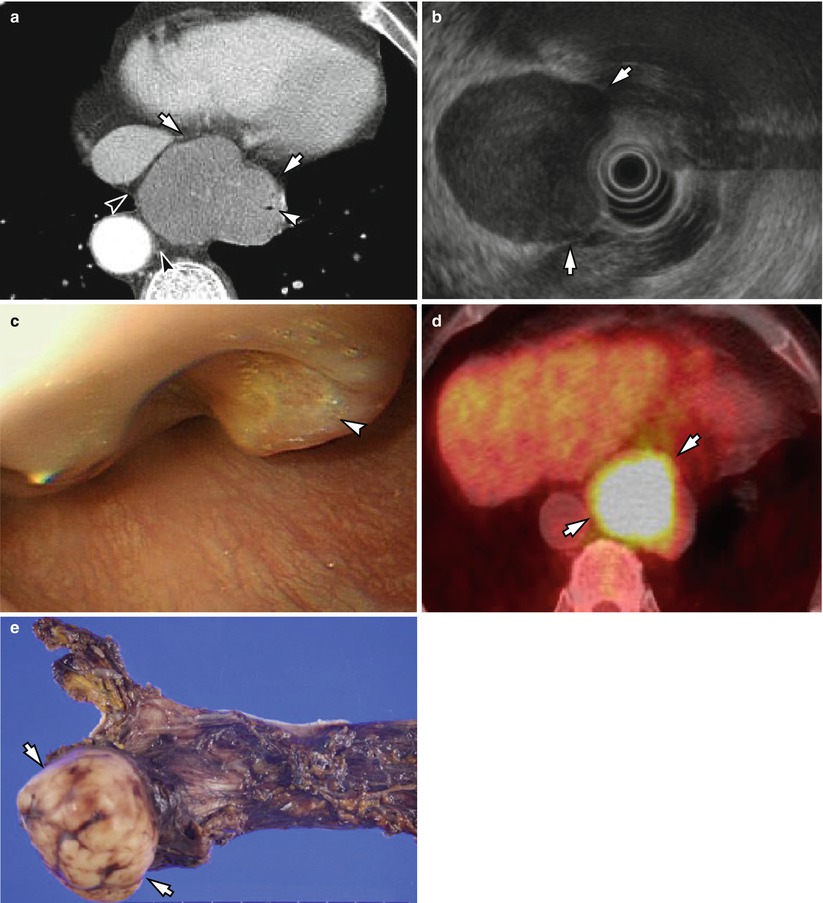
Fig. 3.10
An esophageal malignant GIST in a 77-year-old man. On chest CT scan, an approximately 6 cm eccentric submucosal tumor (arrows) is seen (a). Pinpoint esophageal narrowing is observed (white arrowhead), but fat planes between the aorta and IVC are preserved (black arrowheads). On EUS (b), a 6 cm hypoechoic tumor (arrows) is seen, which arises from proper muscle layer. On EGD (c), the mass shows intact mucosa, but superficial ulcer is observed in some areas (arrowhead), and the mass shows significant hypermetabolic uptake (arrows) on FDG-PET (d). An approximately 6 cm encapsulated mass with ulcer was resected (e), and it was confirmed as a GIST with high risk of tumor progression (mitotic count, 36/50HPF)
3.3.11 Esophageal Schwannoma
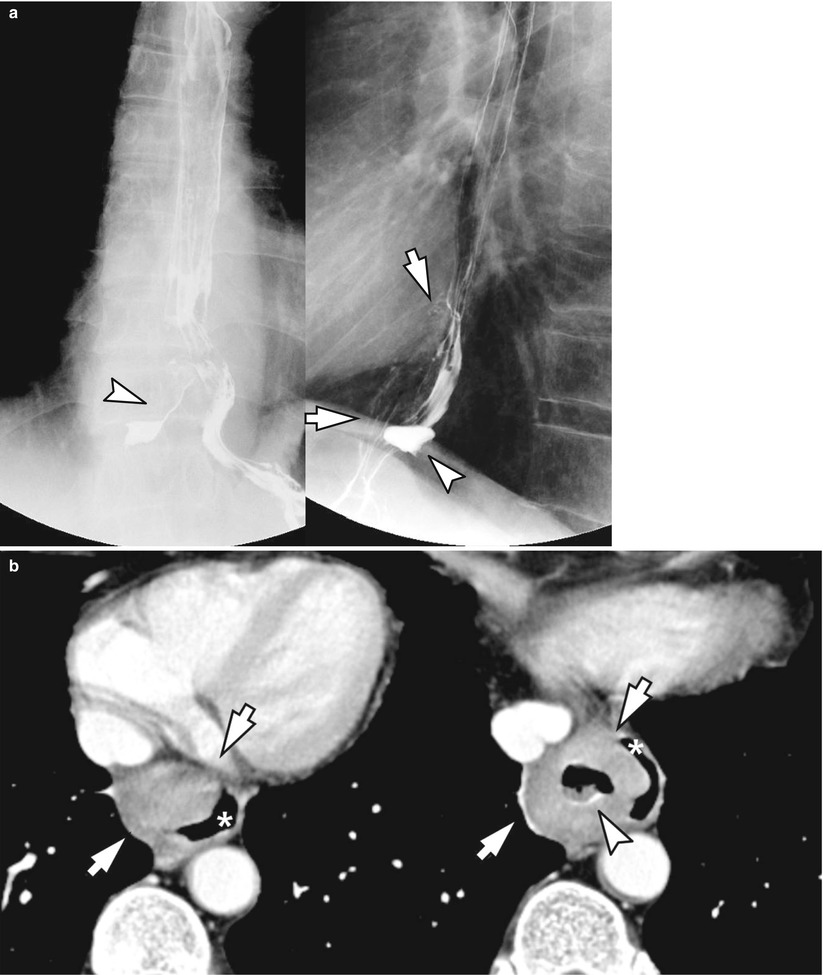
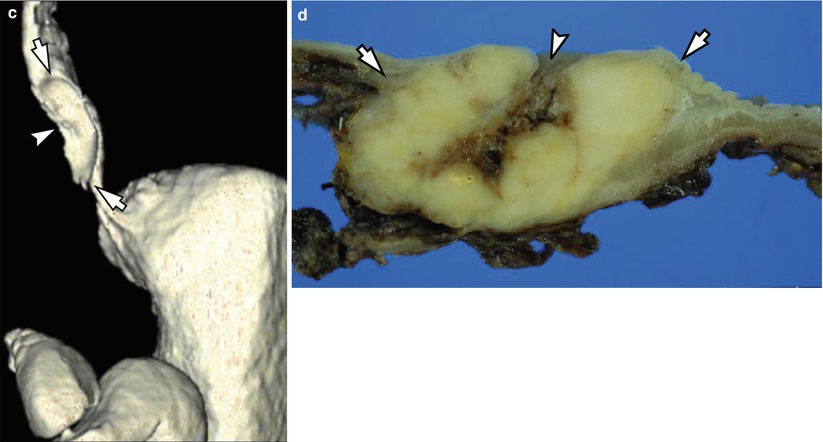
Fig. 3.11
An esophageal schwannoma in a 77-year-old man. On esophagography (a), an eccentric contour deformity of the lower esophagus is seen (arrows), and contrast media filling is also noted (arrowheads), which is suggestive of the presence of the ulcer in the tumor. Chest CT scan (b) reveals a submucosal tumor (arrows) which displaced the esophageal lumen (asterisk), and the tumor has central ulcer (arrowhead) which communicated with the esophageal lumen. On 3D CT esophagography (c), the submucosal tumor (arrows) is demonstrated in the lower esophagus, and the central ulcer is clearly seen (arrowhead). The surgical specimen (d) shows a well-demarcated yellow solid tumor (arrows) with central ulcer (arrowhead), and it was confirmed as a schwannoma involving the submucosa and proper muscle layer
3.3.12 Plexiform Schwannoma
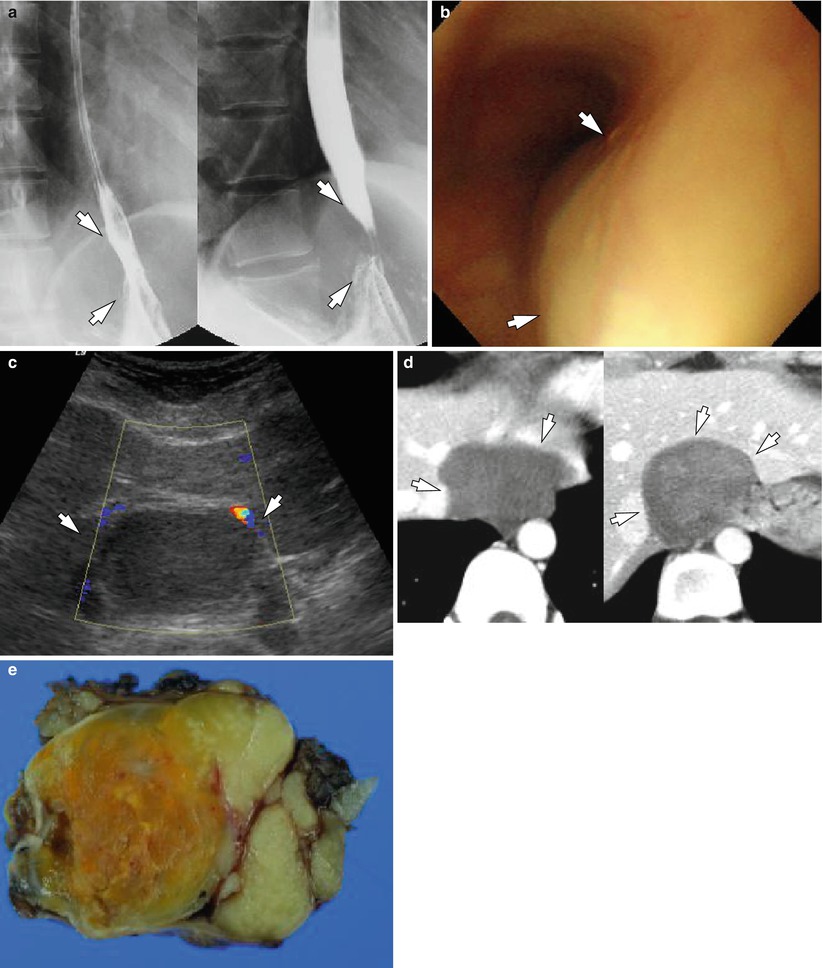
Fig. 3.12
A plexiform schwannoma in a 40-year-old woman, mimicking esophageal submucosal tumor. On esophagography (a), there is an approximately 3 cm mild indentation (arrows) of the lower esophagus, near the GE junction. On EGD (b), a mild bulging contour (arrows) is observed, but neither mucosal lesion nor definite mass was demonstrated. On abdominal US (c), an approximately 5.5 cm homogeneous hypoechoic mass (arrows) is seen, and it shows hypovascularity with pliable margin (arrows) on CT (d). During the resection, the mass was easily divided from the esophagus. The encapsulated grey to yellowish multilobulating mass was confirmed as a plexiform schwannoma (e)
3.3.13 Malignant Peripheral Nerve Sheath Tumor Invading Esophagus
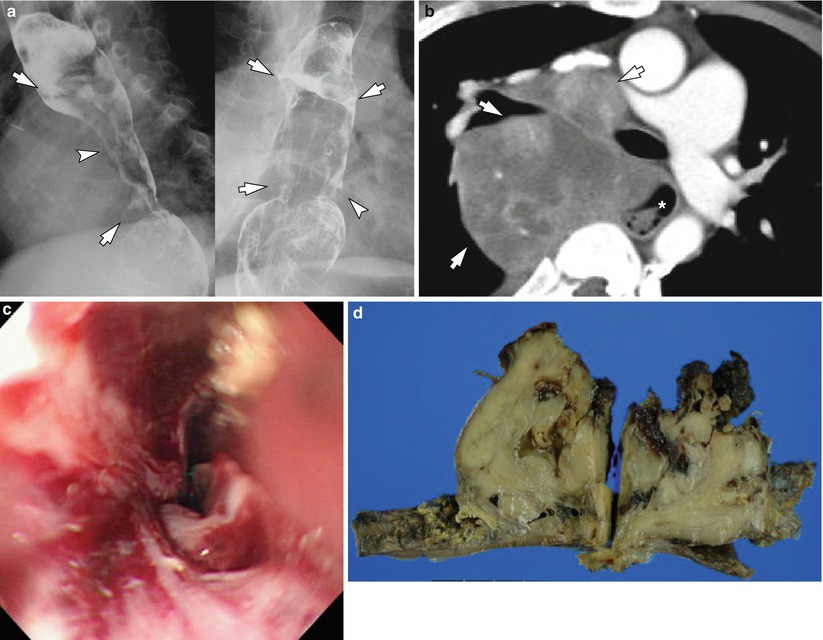
Fig. 3.13
A malignant peripheral nerve sheath tumor in a 35-year-old man with neurofibromatosis. On esophagography (a), a long segmental filling defect with relatively smooth contour (arrows) is seen, and slightly irregular margin (arrowheads) is noted in the distal esophagus, which suggests the presence of invasion or ulceration of the mass. On chest CT scan (b), an approximately 10 cm heterogeneously enhancing mass (arrows) is shown in the mediastinum, invading the pulmonary arteries, bronchus, and esophagus (asterisk). A diffuse esophageal luminal narrowing from UI 25 cm to the distal esophagus is found on EGD, and hyperemic mucosa is seen (c). During esophageal resection, the tumor was attached to the vagus nerve, and it was not separable from the esophagus. The specimen was confirmed as a grade III malignant peripheral nerve sheath tumor, involving the esophageal mucosa (d)
3.3.14 Early Esophageal Cancer (pT1a): Depressed
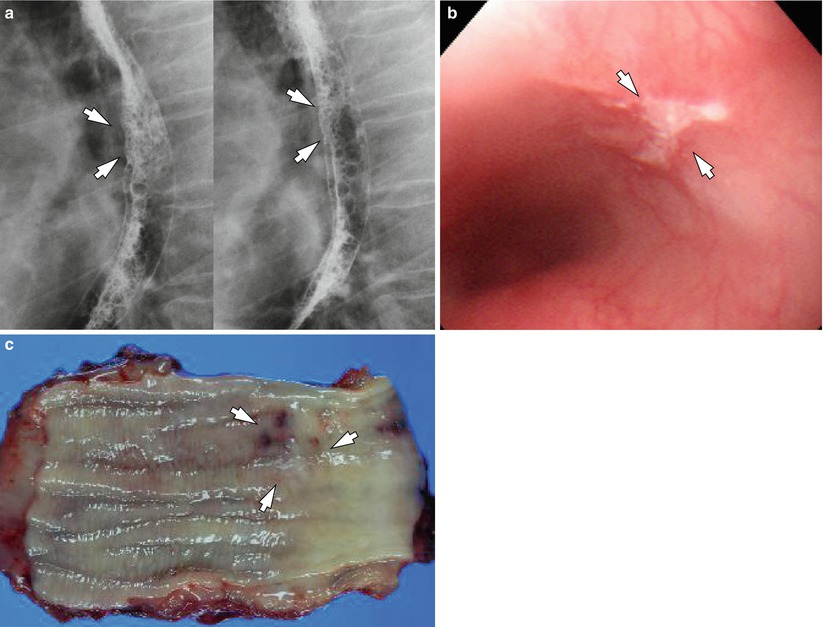
Fig. 3.14
An early esophageal cancer in a 78-year-old man. On esophagography (a), a shallow ulcer (arrows) is seen in the distal esophagus. EGD (b) reveals a shallow ulcer (arrows) in the distal esophagus with subtle fold convergence. After Ivor-Lewis operation, the specimen shows an 1 cm2 depressed lesion (arrows) in the distal esophagus with mucosal congestion due to previously performed endoscopic biopsy (c). It was confirmed as a squamous cell carcinoma (pT1a)
3.3.15 Early Esophageal Cancer (pT1a): Shallow Ulcer
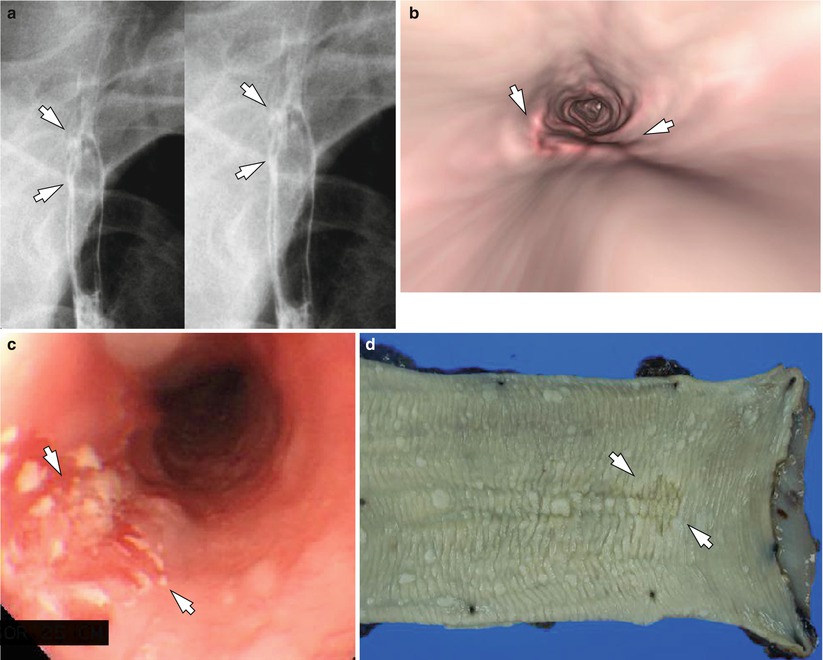
Fig. 3.15
An early esophageal cancer in a 70-year-old man. An approximately 1.2 cm superficial ulcer (arrows) is seen on esophagography (a). On endoluminal view of esophageal CT scan (b), a depressed lesion in the esophagus (arrows) is shown, and on EGD (c), an ill-defined hyperemic shallow depressed lesion is shown (arrows). After resection, the approximately 1.5 cm depressed lesion in the esophagus (d, arrows) was confirmed as a superficial squamous carcinoma (pT1a)
3.3.16 Early Esophageal Cancer (pT1a): Polypoid
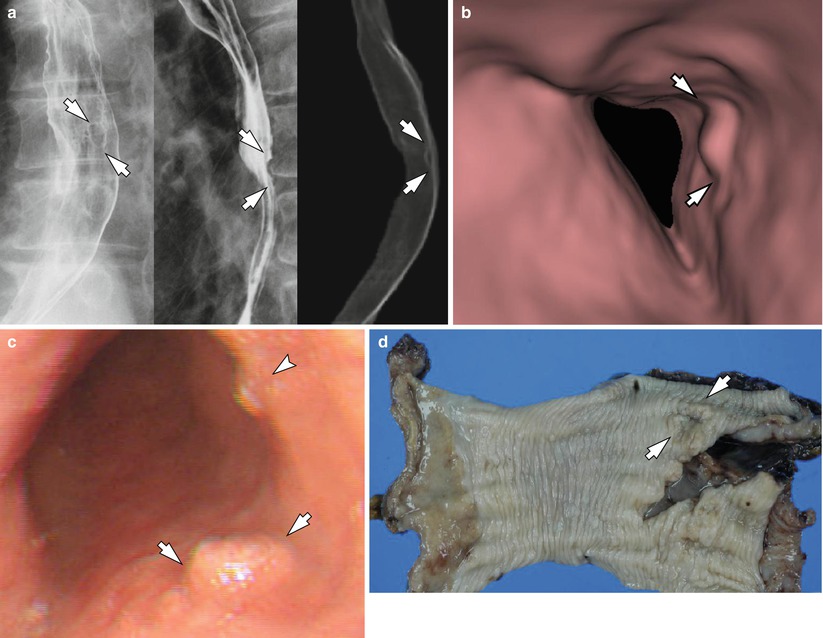
Fig. 3.16




An early esophageal cancer in a 77-year-old man. Esophagography (left, middle) and 3D CT esophagography (right) shows a small elevated lesion (arrows) in the mid esophagus (a). On endoluminal view of CT esophagography, a small polypoid nodule (arrows) is seen in the same level of the esophagus (b). EGD (c) reveals the small polypoid nodule (arrows) and surrounding smaller nodules (arrowhead). After operation, an approximately 2.2 cm superficial squamous carcinoma (d, arrows) invading muscularis mucosa was confirmed (pT1a)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree