Berylliosis
Jud W. Gurney, MD, FACR
Key Facts
Terminology
Strong lightweight element with a high melting point, used in alloys in wide variety of industries
Inhalation causes 2 pulmonary syndromes: Acute chemical pneumonitis and chronic granulomatous lung disease
Imaging Findings
Pattern identical to sarcoidosis; however
Ground-glass opacities more common
Lymphadenopathy not as prominent
Resolution: Ground-glass opacities replaced by microcysts or septal lines
Hilar or mediastinal adenopathy (40%), always associated with lung disease
In sarcoidosis, adenopathy typically regresses as lung disease worsens; not seen with berylliosis
Top Differential Diagnoses
Sarcoidosis
Langerhans Cell Granulomatosis
Silicosis
Clinical Issues
History of beryllium exposure, latent period of 1 month to 40 years (average 10-15 years)
10% of patients with acute disease go on to develop chronic disease
Skin rash, poor wound healing, papular or vesicular rash (itchy)
10% develop renal calculi from hypercalcemia
Beryllium known pulmonary carcinogen; cancer usually develops in patients after acute berylliosis
TERMINOLOGY
Abbreviations and Synonyms
Acute berylliosis, chronic berylliosis, Salem sarcoidosis
Definitions
Beryllium: Strong lightweight element with high melting point, used in alloys in wide variety of industries
Inhalation causes 2 pulmonary syndromes: Acute chemical pneumonitis and chronic granulomatous lung disease
IMAGING FINDINGS
General Features
Best diagnostic clue
Pattern identical to sarcoidosis; however
Ground-glass opacities more common
Lymphadenopathy not as prominent
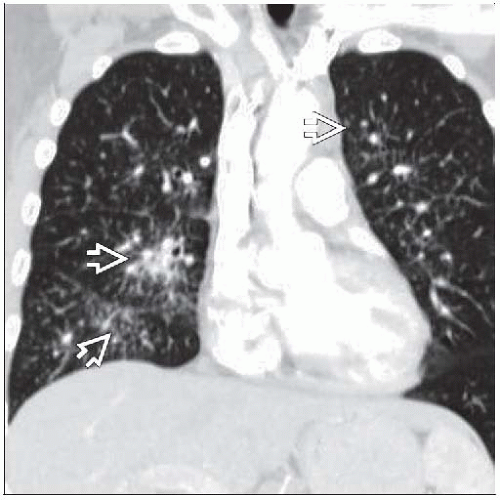
Patient position/location: Primarily mid lung with tendency to upper lobe fibrosis with chronic disease
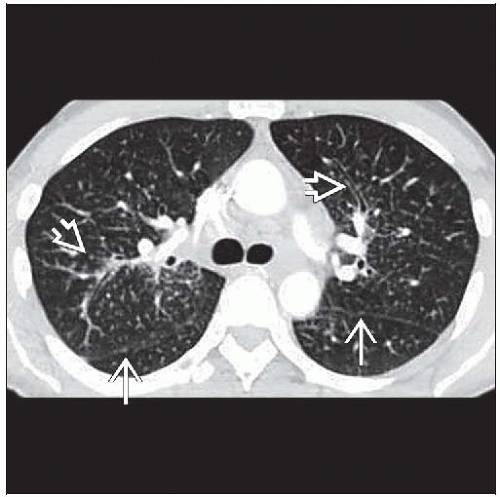
CT Findings
Normal in up to 25% with proven disease
Morphology
Identical pattern to sarcoid
Ground-glass opacities more common
Nodules (65%) > ground-glass opacities (55%) > septal lines (50%)
Nodules may aggregate into progressive massive fibrosis (PMF) (5%)
Nodules may calcify
Upper zonal pleural thickening due to pseudoplaques (aggregation of subpleural nodules)
Distribution
Nodules lie along bronchovascular bundles, peripheral septa, subpleural lung, and fissures (50%)
Honeycombing in advanced disease (5%), typically worse in upper lung zones
Evolution
Successful treatment
Ground-glass opacities either resolve over 3 months or
Replaced by microcysts or septal lines
Other
Hilar or mediastinal adenopathy (40%), always associated with lung disease
Nodes: May have diffuse or eggshell calcification
Intense calcification in 10%
Radiographic Findings
Radiography
Acute
Requires overwhelming exposure
Noncardiogenic pulmonary edema within 72 hours of exposure
Slowly resolves within 1 to 4 weeks, 10% develop chronic disease
Subacute
Onset in weeks with lower exposures
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree