A. Common hepatic duct
B. Main portal vein
C. Gastroduodenal artery
D. Inferior vena cava
E. Proper hepatic artery
F. Middle hepatic vein
A. Pneumobilia
B. Cholangiocarcinoma
C. Choledocholithiasis
D. Ascariasis
3 A 78-year-old man presents with right upper quadrant pain. There was positive maximum tenderness over the gallbladder during the ultrasound exam. What is the most likely diagnosis?

A. Acute cholecystitis
B. Acute hepatitis
C. Hepatic abscess
D. Adenomyomatosis
4 An intubated patient in the ICU with persistent fevers and leukocytosis was evaluated with right upper quadrant ultrasound as shown. Which of the following statements is true about acute acalculous cholecystitis (AAC)?

A. Emergent cholecystectomy is indicated.
B. AAC accounts for more than half of all cases of acute cholecystitis.
C. More than half of patients with AAC present in the outpatient setting.
D. Ultrasound is the most appropriate initial imaging study of choice for AAC even though it is less sensitive than cholescintigraphy.
5a An 18-year-old woman status post recent cholecystectomy presents with signs and symptoms of peritonitis. Based on the CT and MRCP shown below, what is the most likely diagnosis?

A. Bile leak
B. Pseudoaneurysm with active hemorrhage
C. Gallbladder remnant
D. Duplicated gallbladder
5b The patient in Question 5a underwent treatment including exploratory laparotomy to evacuate peritoneal fluid collections, drain placement, and antibiotics. After recovery, the drains were removed. Two months later, the patient presents with jaundice and the following MRCP. What is the diagnosis?

A. Recurrent bile leak
B. Cholangiocarcinoma
C. Sclerosing cholangitis
D. Benign stricture related to biliary injury
6 The most common cause of a benign biliary stricture is:
A. Prior hepatobiliary surgery
B. Primary sclerosing cholangitis
C. Recurrent pyogenic cholangitis
D. Pancreatitis
7 Three patients presented with right upper quadrant pain and underwent ultrasound and CT scan. Match the ultrasound image for each patient (1 to 3) with that patient’s corresponding CT image (A to C). Each option may be used only once.
A.

B.

C.

Patient 1:

Patient 2:

Patient 3:

8 Match the images of patients 1 to 3 with the type of choledochal cyst (A to E) according to the Todani classification. Each option may be used once, more than once, or not at all.
A. Type I
B. Type II
C. Type III
D. Type IV
E. Type V
Patient 1:

Patient 2:

Patient 3:

9 A 43-year-old man presents with epigastric pain. An ultrasound was performed, which demonstrated a 2 cm finding in the gallbladder. What is the most appropriate next step?

A. Six-month follow-up ultrasound exam, as the vast majority of gallbladder polyps are benign.
B. No follow-up is necessary, as this is tumefactive sludge.
C. Surgical consultation, as gallbladder polyps >1 cm carry a significant risk of being malignant and should be excised.
D. PET-CT, as surgical excision should be based on metabolic activity of the lesion.
10 For patients 1 to 3, match the right upper quadrant abdominal ultrasound imaging findings with the name of the artifact (A to D). Each option may be used once or not at all.
A. Twinkle artifact
B. Comet tail artifact
C. Mirror artifact
D. Ring down artifact
Patient 1: Image of the gallbladder.

Patient 2: Image of bowel near the liver.

Patient 3: Image of the kidney.

11 Based on the following ultrasound image from the previous question, what is the most likely diagnosis?

A. Adenomyomatosis
B. Emphysematous cholecystitis
C. Gallstones
D. Gallbladder carcinoma
A. Autoimmune hepatitis.
B. AIDS.
C. Inflammatory bowel disease.
D. Parasitic infection.
For each patient in Questions 13 to 18, select the most likely diagnosis (A to I). Each option may be used once, more than once, or not at all.
A. Gangrenous cholecystitis
B. Adenomyomatosis
C. Phrygian cap
D. Gallbladder laceration
E. Duodenal duplication cyst
F. Choledochal cyst
G. Dropped gallstone with abscess
H. Bouveret syndrome
I. Remnant gallbladder infundibulum
13 An 87-year-old woman with epigastric pain, fever, leukocytosis, and lactic acidosis. Coronal and sagittal CT images are shown.

15 A 70-year-old woman with recurrent episodes of abdominal pain. Two images from an MRCP are shown. Identify the structure indicated by the arrow.

16 A 61-year-old woman with right upper quadrant discomfort. Identify the structure indicated by the arrow.

17 A 57-year-old woman for evaluation of incidentally discovered gallbladder lesion. Axial and coronal MR images are shown.

18 An 86-year-old woman with right flank pain and nausea. The arrow points to an abnormality in the porta hepatis. Identify the disease process revealed on the images.

19 Three contrast-enhanced CT images of the right upper quadrant are shown. What is the most likely diagnosis?

A. Mirizzi syndrome
B. Gallbladder carcinoma
C. Metastatic periportal adenopathy
D. Klatskin tumor
20 Match the CT images of patients 1 to 5 with the best diagnosis or description of the finding (A to E). Each option may be used once, more than once, or not at all.
A. Pneumobilia
B. Portal venous gas
C. Periportal edema
D. Portal venous thrombosis
E. Biliary obstruction
Patient 1:

Patient 2:

Patient 3:

Patient 4:

Patient 5:

21 Match the images from the 99mTc hepatobiliary iminodiacetic acid (HIDA) scan images of patients 1 to 5 with the most likely diagnosis (A to E) among the options listed. Each option may be used once, more than once, or not at all.
A. Within normal limits
B. Acute high-grade bile duct obstruction
C. Bile leak
D. Acute cholecystitis
E. Chronic cholecystitis
Patient 1: Images at 57 to 60 minutes and 5 hours.

Patient 2: Image at 25 to 27 minutes.

Patient 3: Image at 57 to 60 minutes.

Patient 4: Anterior images with patient in right lateral decubitus position at 26 minutes and supine position at 30 minutes.

Patient 5: Images at 57 to 60 minutes and then 28 to 30 minutes after IV morphine injection.

22 A 64-year-old man presented with right upper quadrant pain. Images from his CT scan are shown. Which of the following features if present is most suggestive of gallbladder adenocarcinoma over perforated cholecystitis?

A. Abnormal enhancement of adjacent hepatic parenchyma
B. Gallbladder wall thickness >10 mm
C. 4-cm heterogeneously enhancing porta hepatis lymph node
D. Intrahepatic biliary dilatation
23a A 52-year-old man who immigrated from the Philippines presents with worsening right upper quadrant pain. An ultrasound and CT scan were performed. Images are shown of the right hepatic lobe, but similar findings were also seen in the left lobe. What is the finding?

A. Calcification in a branching pattern
B. Enhancing mass in a branching pattern
C. Focal fat in a branching pattern
D. Air in a branching pattern
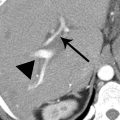
23b An MRI was performed in the same patient with images shown below. What is the most likely diagnosis?

T2W and T1W
A. Ischemic bowel with portal venous gas
B. Hepatocellular carcinoma with portal venous thrombus
C. Ascariasis
D. Recurrent pyogenic cholangitis
24a A 34-year-old patient presents with a CD4 count of 46/mm3. What is the most common infectious agent associated with these ERCP findings?

A. Kaposi sarcoma herpesvirus (human herpesvirus 8)
B. Cryptosporidium
C. Epstein-Barr virus (human herpesvirus 4)
D. Microsporidia
24b Which is the most common feature found in the majority of patients with AIDS cholangiopathy?
A. Papillary stenosis
B. Long extrahepatic bile duct stricture
C. Intrahepatic biliary stones
D. Biliary diverticula
25 The most common presentation of gallbladder carcinoma is:
A. A large mass replacing the gallbladder.
B. A polypoid lesion projecting into the lumen.
C. Focal wall thickening.
D. Diffuse wall thickening.
26 Which of the following statements is TRUE about the disease demonstrated on the following images?

A. The complex form of this disease is associated with congenital hepatic fibrosis.
B. This disease represents a multifocal cystic neoplasm.
C. This disease is curable with antibiotics.
D. Both intrahepatic and extrahepatic bile ducts are involved in this disease.
For patients presenting with jaundice in Questions 27 to 30, match the imaging findings with the most likely diagnosis (A to E). Each option may be used once, more than once, or not at all.
A. Ascariasis
B. Cholangiocarcinoma
C. Pancreatic ductal adenocarcinoma
D. Ampullary carcinoma
E. Choledocholithiasis
31 Match the MRCP images for patients 1 to 3 below with the correct description of biliary ductal anatomy (A to E).
A. Conventional biliary anatomy
B. Low and medial insertion of the cystic duct
C. Posterior right hepatic duct draining into left hepatic duct
D. Left hepatic duct draining into right hepatic duct
E. Biliary trifurcation
Patient 1:

Patient 2:

Patient 3:

32 A 70-year-old woman with shortness of breath was evaluated with a CT pulmonary angiogram shown on the left. For comparison, a contrast-enhanced CT previously performed 13 hours earlier is shown on the right. What is the gallbladder finding on the image on the left?

A. Acute cholecystitis
B. Milk of calcium
C. Vicarious excretion of contrast
D. Hydrops
33 A patient with a history of liver transplant with hepaticojejunostomy was evaluated with MRI. Normal arterial flow was identified at Doppler ultrasound. What is the most likely diagnosis?

A. Ischemic cholangiopathy
B. Choledocholithiasis
C. Multifocal cholangiocarcinoma
D. Recurrent primary sclerosing cholangitis
34 Match the biliary findings indicated by the arrows in patients 1 to 4 with the correct description (A to D). Each option may be used once, more than once, or not at all.
A. Pneumobilia
B. Surgical clip
C. Crossing vessel
D. Bile flow artifact
Patient 1:

Patient 2:

Patient 3:

Patient 4:

ANSWERS AND EXPLANATIONS
1 Answers:
1:A. Common hepatic duct
2:E. Proper hepatic artery
3:B. Main portal vein
This is the classic “Mickey Mouse” configuration of the structures demonstrated on abdominal ultrasound that make up the portal triad. This relationship is found in the porta hepatis at the margin of the hepatoduodenal ligament. The corresponding color Doppler image is shown below. The larger vessel is the portal vein (PV). In normal patients, the two “ears” representing the bile duct (BD) and the proper hepatic artery (HA) on the left are similar in size. With biliary obstruction, the dilated duct enlarges the right “ear.”

The extrahepatic common duct is normally ≤6 mm diameter (measured from inner wall to inner wall) in patients 60 years or younger, with an additional 1 mm caliber increase acceptable for each additional decade up to 10 mm. After cholecystectomy, patients are also allowed up to 10 mm. These measurements are guidelines and should be correlated with ancillary imaging findings as well as the clinical scenario to help determine if biliary obstruction is likely.
References: Brant WE. Chapter 36: Abdominal ultrasound. In: Brant WE, Helms CA (eds). Fundamentals of diagnostic radiology, 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2007:927–953.
Tirumani SH, Shanbhogue AK, Vikram R, et al. Imaging of the porta hepatis: spectrum of disease. Radiographics 2014;34(1):73–92.
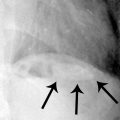
2 Answer C.Coronal and axial T2W images from an MRCP demonstrate two dark filling focal defects in a mildly prominent common bile duct. The axial image shows dependent location of the filling defect. Findings are consistent with choledocholithiasis. There is also cholelithiasis, with a stone seen in the gallbladder.
Up to one-third of patients with gallstones develop symptoms, which may include biliary colic, cholecystitis, cholangitis, or pancreatitis. Ultrasound is usually the initial imaging modality performed in patients with right upper quadrant pain and suspected biliary pathology. Choledocholithiasis accounts for the majority of cases of biliary obstruction, most often migrating from the gallbladder. Patients with suspected choledocholithiasis without direct visualization of a ductal stone on ultrasound may proceed to MRCP or ERCP for further evaluation.
MRCP has a high sensitivity of about 90% for choledocholithiasis, compared to 20% to 60% for ultrasound. The stones are visualized as dark filling defects surrounded by bright bile on the heavily T2W images of MRCP. The stones may be round or have a faceted appearance with angular margins. Stones impacted in the ampulla may be missed or misdiagnosed as ampullary lesions due to the lack of surrounding fluid. Tiny stones ≤3 mm may still be hard to detect even on thin-slice MRCP images, and patients may ultimately require ERCP for diagnosis and treatment.
Pneumobilia would appear as a ventral (nondependent) hypointensity with air–fluid level on axial images, highlighting the importance of careful correlation with axial images to make the distinction with choledocholithiasis. Cholangiocarcinoma or ampullary carcinoma may present as a soft tissue mass or a stricture. With ascariasis, the parasites can be seen in the bile duct as a linear filling defect.
References: Irie H, Honda H, Kuroiwa T, et al. Pitfalls in MR cholangiopancreatographic interpretation. Radiographics 2001;21(1):23–37.
Yeh BM, Liu PS, Soto JA, et al. MR imaging and CT of the biliary tract. Radiographics 2009;29(6):1669–1688.
3 Answer A.This patient has a constellation of findings consistent with acute (calculous) cholecystitis as follows:
- Sonographic Murphy sign is positive, with maximum tenderness during compression with the transducer over the gallbladder.
- The gallbladder is distended with shadowing gallstones (long black arrow) as well as sludge.
- The gallbladder wall is edematous with a striated appearance and measures >3 mm in thickness as delineated by the calipers.
- The gallbladder wall is hypervascular (short white arrows) on the color Doppler image, indicating inflammation.
- Pericholecystic fluid is identified (long white arrow).

Although the individual imaging features of acute cholecystitis (AC) on ultrasound are nonspecific, identification of multiple features increases diagnostic confidence. Meta-analyses reveal overall excellent (>80%) sensitivity and specificity of ultrasound for AC. A sonographic Murphy sign may be the most sensitive feature for AC, but specificity is relatively low. A positive Murphy sign in combination with cholelithiasis has been found to have a positive predictive value of about 90%, but it is not always possible to adequately assess for the Murphy sign in patients who have taken pain medication or have been sedated. Among the answer choices, acute hepatitis and adenomyomatosis can also cause gallbladder wall thickening, but they are less likely choices given this constellation of findings. Adenomyomatosis is usually an asymptomatic incidental finding. Other causes of diffuse gallbladder wall thickening are listed in the table below.
Patients with AC may present with right upper quadrant pain, fever, and leukocytosis. A gallstone that is persistently impacted in the cystic duct or gallbladder neck causes gallbladder obstruction and distention. Subsequently, inflammation of the gallbladder wall is induced by the accumulated bile salts or superinfection. AC can progress to life-threatening complications which are best evaluated by CT, including gas formation, gangrene, hemorrhage, and perforation. Definitive treatment for AC is cholecystectomy.
Causes of Diffuse Gallbladder Wall Thickening

References: ACR Appropriateness Criteria: right upper quadrant pain. American College of Radiology website. http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/RightUpperQuadrantPain.pdf. Published 1996. Updated 2013. Accessed August 2, 2015.
Hanbidge AE, Buckler PM, O’Malley ME, et al. From the RSNA refresher courses: imaging evaluation for acute pain in the right upper quadrant. Radiographics 2004;24(4):1117–1135.
O’Connor OJ, Maher MM. Imaging of cholecystitis. AJR Am J Roentgenol 2011;196(4):W367–W374.
4 Answer D.This patient has a sludge-filled gallbladder with no stones identified. There is borderline gallbladder wall thickening. In this critically ill patient, findings could represent acute acalculous cholecystitis (AAC). Cholescintigraphy with HIDA scan augmented with morphine reportedly has a higher sensitivity of 67% for AAC compared to ultrasound, which has sensitivity of 50%. Nevertheless, ultrasound is the most appropriate initial study for suspected acute cholecystitis (both calculous and acalculous) with a rating of 9 out of 10 as noted by the ACR Appropriateness Criteria, compared to 6 out of 10 for cholescintigraphy. The advantages of ultrasound over cholescintigraphy include technical considerations such as greater availability, shorter scan time, and lack of radiation. Ultrasound also has benefits of morphologic evaluation over cholescintigraphy allowing detection of gallstones, assessment of duct caliber, and identification of alternative diagnoses. HIDA scan should be still considered an important ancillary study for the diagnosis of acute cholecystitis in the setting of an equivocal ultrasound.
About 15% of cases of acute cholecystitis represent AAC. Patients are often seriously ill and have been hospitalized in the ICU for a prolonged period of time before the development of AAC. AAC rarely presents de novo in an outpatient setting. The diagnosis of AAC can be problematic and is one of exclusion because fever and leukocytosis are nonspecific signs in the at-risk patient population. These patients frequently have other conditions that can cause gallbladder wall thickening. It may not be possible to assess for a sonographic Murphy sign because of patient intubation and use of analgesics and sedatives.
AAC has a higher morbidity and mortality than conventional acute calculous cholecystitis. Rapid progression to gangrene and perforation contributes to a high mortality of up to 65%. Percutaneous cholecystostomy with drainage catheter placement can be both diagnostic and therapeutic. It is generally safer than performing an emergent cholecystectomy in a critically-ill patient and can be an effective temporizing measure until patients can proceed to cholecystectomy.
References: ACR Appropriateness Criteria: right upper quadrant pain. American College of Radiology website. http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/RightUpperQuadrantPain.pdf. Published 1996. Updated 2013. Accessed August 2, 2015.
Bennett GL. Chapter 77: Cholelithiasis, cholecystitis, choledocholithiasis, and hyperplastic cholecystoses. In: Gore RM, Levine MS (eds). Textbook of gastrointestinal radiology, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2015:1348–1391.
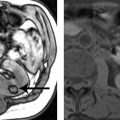
5a Answer A.The patient’s CT and MRCP show a collection of fluid and gas in the cholecystectomy bed. There is no high density or extravasation of IV contrast to suggest pseudoaneurysm or active hemorrhage. A collection in the gallbladder fossa after recent cholecystectomy is not uncommon and may be a postoperative finding that resolves spontaneously. However, in a patient with signs and symptoms of peritonitis, this collection could represent a bile leak or abscess that requires intervention. A gallbladder remnant may be left behind if adhesions or variant anatomy prevents complete removal of the gallbladder but should be small rather than filling the length of the gallbladder fossa. A duplicated (accessory) gallbladder is a very rare congenital anomaly that should not be a primary consideration and presumably would have been recognized and removed at cholecystectomy.
If the diagnosis is unclear, an HIDA scan may be useful to confirm a bile leak. MRCP with a hepatobiliary agent such as gadoxetate disodium (Eovist, Bayer HealthCare Pharmaceuticals) has also been used to help diagnose and localize bile leaks, as 50% of this contrast agent is taken up by hepatocytes and excreted into the biliary system. Extravasation of this contrast outside the biliary tree in the hepatobiliary phase would indicate a bile leak. Treatment of bile leaks may involve a combination of endoscopic, percutaneous, and surgical intervention.
References: Melamud K, LeBedis CA, Anderson SW, et al. Biliary imaging: multimodality approach to imaging of biliary injuries and their complications. Radiographics 2014;34(3):613–623.
Raman SP, Fishman EK, Gayer G. Chapter 81: Postsurgical and traumatic lesions of the biliary tract. In: Gore RM, Levine MS (eds). Textbook of gastrointestinal radiology, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2015:1348–1391.
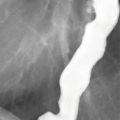
5b Answer D.Two months later, the MRCP and the following ERCP show a high-grade obstruction (arrow) at the biliary hilum near the cholecystectomy clips with intrahepatic biliary ductal dilation. There is no surrounding fluid collection on the MR or extravasation on the ERCP to indicate a recurrent bile leak. (The round area of contrast on the ERCP represents contrast in the duodenum.) Given the time course and the preceding events, this is consistent with a benign stricture complicating the recent biliary injury rather than development of cholangiocarcinoma or sclerosing cholangitis.

The most common locations for postcholecystectomy strictures are at the junction of the cystic duct with the common duct and at the biliary hilum. Although these strictures are benign, they can be difficult to manage. Treatment includes ERCP for stent placement, but recurrence is common. Surgical intervention with hepaticojejunostomy may eventually be required.
References: Katabathina VS, Dasyam AK, Dasyam N, et al. Adult bile duct strictures: role of MR imaging and MR cholangiopancreatography in characterization. Radiographics 2014;34(3):565–586.
Raman SP, Fishman EK, Gayer G. Chapter 81: Postsurgical and traumatic lesions of the biliary tract. In: Gore RM, Levine MS (eds). Textbook of gastrointestinal radiology, 4th ed. Philadelphia, PA: Elsevier/Saunders; 2015:1348–1391.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree