MULTILOCULAR CYSTIC HEPATIC LESIONS
A. CONGENITAL
1. Polycystic liver disease
B. NEOPLASTIC
1. Biliary cystadenoma / ~carcinoma
2. Hepatocellular carcinoma
3. Cystic metastasis: neuroendocrine tumor, melanoma, GIST, mucinous colorectal / mucinous ovarian carcinoma; treated metastasis
4. Inflammatory myofibroblastic tumor
5. Mesenchymal hamartoma
C. INFECTIOUS
1. Pyogenic abscess
2. Amebic abscess
3. Echinococcal cyst
D. TRAUMATIC
1. Intraparenchymal hematoma
2. Biloma
ATTENUATION OF CYSTIC HEPATIC LESIONS
1. Simple hepatic cyst -10 – 10 HU
2. Hematoma (acute) 40 – 60 HU
3. Clotted blood 45 – 70 HU
4. Biloma 0 – 15 HU
5. Pyogenic abscess 0 – 45 HU
6. Hydatid mother cyst 3 – 30 HU
7. Hydatid daughter cyst lower than mother cyst
6. Amebic abscess 10 – 20 HU
◊ Density measurements in general are of little help due to variability of cyst content and change over time!
Solitary Echogenic Liver Mass
mnemonic: Hyperechoic Focal Masses Affecting the Liver
Hematoma, Hepatoma, Hemangioma, Hemochromatosis, Hepatoblastoma
Fatty infiltration, Focal nodular hyperplasia, Fibrosis
Metastasis
Adenoma
Lipoma
Solid Liver Lesion with Cystic Degeneration
1. Hepatocellular carcinoma / adenoma
2. Fibrolamellar carcinoma
3. Intrahepatic cholangiocarcinoma
4. Angiosarcoma
5. Epithelioid hemangioendothelioma
6. Lymphoma
7. Metastatic disease
Liver Mass Surrounded by Echogenic Rim
1. Metastasis: esp., cystic pancreatic endocrine tumor
2. Adenoma
3. Hemangioma
Multiple Liver Lesions
A. BENIGN TUMOR
1. Cavernous hemangioma
2. Adenoma
3. Regenerating hepatic nodules
4. Biliary microhamartomas
B. INFECTION
1. Multiple abscesses / microabscesses
2. Mycobacterial + fungal infection
3. Inflammatory pseudotumors
C. CONGENITAL
1. Polycystic disease
2. Caroli disease
D. MALIGNANCY
1. Metastases (most common malignant liver tumor)
2. Multifocal hepatoma
3. Lymphoma
E. OTHER
1. Sarcoidosis
2. Simple cysts
3. Langerhans cell histiocytosis (echogenic nodules)
4. Multifocal fat deposition
Bull’s-eye Lesions of Liver
1. Candidiasis (in immunocompromised)
2. Metastases
3. Lymphoma, leukemia
4. Sarcoidosis
5. Septic emboli
6. Other opportunistic infections
7. Kaposi sarcoma
Miliary Hepatosplenic Lesions
1. Tuberculosis
2. Metastases
3. Fungal infections
4. Sarcoidosis
5. Lymphoma
Fat- / Lipid containing Liver Mass
1. Lipoma
2. Angiolipoma
3. Angiomyolipoma: eg, tuberous sclerosis
4. Hepatocellular carcinoma
5. Hepatocellular adenoma
6. Liposarcoma metastasis
7. Malignant teratoma metastasis (+ calcifications)
8. Focal fatty change
9. Focal nodular hyperplasia (rare)
10. Regenerative & dysplastic nodules
11. Fat packing
Cystic Liver Lesion
A. NONNEOPLASTIC
1. Congenital hepatic cyst
2. Hematoma
3. Echinococcal cyst
4. Liver abscess
5. Fibropolycystic liver disease
6. Intrahepatic pseudocyst
7. Biloma
B. NEOPLASTIC
1. Mesenchymal hamartoma
2. Undifferentiated (embryonal) sarcoma
3. Malignant mesenchymoma
4. Biliary cystadenoma / cystadenocarcinoma
◊ < 5% of intrahepatic cysts are of biliary origin!
5. Lymphangioma
6. Necrotic ischemic neoplasm: HCC, giant cavernous hemangioma
7. Cystic metastasis: ovarian / gastric carcinoma
Fibropolycystic Liver Disease
= unique group of entities with derangement of embryonic biliary ductal plate development surrounding portal vein
◊ Coexistence of hepatic + renal anomalies
A. SMALL INTERLOBULAR BILE DUCTS
1. Congenital hepatic fibrosis
2. Biliary hamartomas
Associated with: autosomal recessive (juvenile) polycystic kidney disease
B. MEDIUM-SIZED BILE DUCTS
1. Autosomal dominant polycystic disease
Associated with: autosomal dominant (adult) polycystic kidney disease
C. LARGE INTRAHEPATIC BILE DUCTS
1. Caroli disease
D. LARGE EXTRAHEPATIC BILE DUCTS
1. Choledochal cyst
Liver Mass with Capsule
1. Hepatocellular carcinoma
2. Hepatocellular adenoma
3. Focal nodular hyperplasia (thin incomplete capsule)
Liver Mass with Capsular Retraction
1. Cholangiocarcinoma
2. Fibrolamellar carcinoma
3. Epithelioid hemangioendothelioma
4. Confluent hepatic fibrosis
or any hepatic malignancy
Disease of Hepatic Capsular & Subcapsular Region
A. INFECTION / INFLAMMATION
1. Perihepatitis
2. Parasites: fascioliasis, paragonimiasis, sparganosis
→ penetration of intestinal wall → migration through peritoneal cavity → perforation of liver capsule with initially subcapsular infestation
B. METASTATIC DISEASE
(a) seeded metastasis: ovarian cancer
(b) invasion via perihepatic ligaments: cancer of stomach, duodenum, pancreas, colon, anterior abdominal wall
(c) direct invasion from adjacent organ: cancer of stomach, gallbladder, adrenal gland, kidney
C. PSEUDOLESION OF ALTERED HEMODYNAMICS
1. Third inflow
2. Arterioportal shunt
3. Compression of liver
4. Portal vein obstruction
5. Hepatic vein / IVC obstruction
6. Hepatic infarction
7. Intrahepatic vascular shunt: superior vein of Sappey, umbilical + paraumbilical veins, right posterior portal vein, venovenous surface collaterals
D. OTHERS
1. Focal fat sparing / focal fat infiltration
2. Confluent hepatic fibrosis
Hyperintense Liver Mass on T1WI
◊ Usually due to lipid, hemorrhage or melanin!
1. Hepatocellular adenoma
2. Hepatocellular carcinoma
3. Regenerative & dysplastic nodule
4. Melanoma
5. Hemorrhage (methemoglobin), hemorrhagic tumor
6. Focal fat deposit, lipoma
7. Cyst with high protein content
8. Thrombosed hemangioma (rare)
9. Paramagnetic contrast agents + iodized oil
Hypointense Liver Lesion on T2WI
A. ABSOLUTE
› blood degradation products
» acute intracellular deoxyhemoglobin
» subacute intracellular methemoglobin
» chronic intracellular iron ferritin / hemosiderin
1. Hepatocellular adenoma ← internal bleeding
2. Hepatocellular carcinoma ← internal bleeding
3. Metastasis
4. Focal nodular hyperplasia ← intratumoral hemolysis
5. Nodular regenerative hyperplasia
6. Peliosis hepatis ← hemorrhage in large vascular spaces
7. Hematoma
› iron (intracellular paramagnetic Fe3+)
1. Siderotic nodule
2. Dysplastic nodule
3. HCC
› copper (= divalent paramagnetic copper)
1. Wilson disease
2. HCC
3. Focal nodular hyperplasia
› macromolecules ← restricted motion of water bound to protein
» smooth muscle
1. Leiomyoma
2. Angiomyolipoma
» fibrosis
1. Fibrolamellar HCC
2. Intrahepatic cholangiocarcinoma
3. HCC
4. Metastasis of adenocarcinoma
5. Focal nodular hyperplasia
6. HCA
» mucin (= desiccated mucinous secretions)
1. Metastasis
» fibrinogen (intracytoplasmic inclusions = fibrinogen in dilated rough endoplasmic reticulum)
1. HCC
» keratin
1. Metastasis
» melanin ← presumably related to higher melanin levels or to old hemorrhage
1. Malignant melanoma
2. Metastasis
› necrosis (coagulative = dehydrated necrosis)
1. Metastasis
2. Solitary necrotic nodule
3. HCC
4. HCA
› calcium
1. Granuloma
2. Healed inactive hydatid cyst
3. Fibrolamellar HCC
4. Metastasis: mucinous cancer of colon, stomach, breast, ovary / osteo- and chondrosarcoma
5. HCA
6. Teratoma
B. RELATIVE
› fat (= macroscopic intratumoral fat)
1. Hepatocellular adenoma
2. Hepatocellular carcinoma
3. Lipoma
4. Angiomyolipoma
5. Focal nodular hyperplasia
Liver Mass on Diffusion-Weighted Imaging
= quantification of water diffusion + microcapillary blood perfusion ← based on incoherent intravoxel motion
A. Tissue with restricted diffusion (↓ ADC)
1. Tumor: usually lower ADC for malignant lesion
2. Cytotoxic edema
B. Tissue with less restricted diffusion (↑ ADC)
= tissue of low cellularity / with disrupted cell membranes
1. Cyst
2. Hemangioma
3. Treated nonviable / necrotic tumor
Uptake of Superparamagnetic Iron Oxide Particles
Action: preferential entrapment by Kupffer cells
1. Focal nodular hyperplasia
2. Well-differentiated HCC
3. Dysplastic nodule
4. Hepatic adenoma
Enhancement Characteristics of Liver Mass
Hypovascular Liver Lesion
= less dense than adjacent liver parenchyma during arterial + portal venous phase
Hypo- / NONENHANCING BENIGN LIVER LESION
1. “To small to characterize” implies unreliable density measurement
› small metastasis = low probability
› microabscesses = clinically obvious
› biliary hamartoma = usually multiple
2. Hepatic cyst
3. Caroli disease
4. ADPKD
5. Abscess
6. Hydatid cyst
7. Biliary cystadenoma
8. Regenerating / dysplastic nodule
9. Lipoma
10. Bile duct hamartoma
12. Sarcoidosis
13. Histoplasmosis
HYPOENHANCING MALIGNANT LIVER LESION
1. Metastasis to liver
2. Lymphoma
3. Cholangiocarcinoma
Low-density Hepatic Mass with Enhancement
1. Hepatocellular carcinoma
2. Hypervascular metastases
= lesions that may be obscured after contrast injection: pheochromocytoma, carcinoid, melanoma
3. Cavernous hemangioma
4. Focal nodular hyperplasia with central fibrous scar
5. Hepatic adenoma
Ring-enhancing Targetlike Liver Mass
1. Metastasis
2. Abscess
3. Cholangiocarcinoma
4. Treated HCC
5. Epithelioid hemangioendothelioma
6. Confluent hepatic fibrosis
7. Giant atypical cavernous hemangioma
RIM ENHANCEMENT
1. Biliary cystadenoma / ~ adenocarcinoma
2. Hematoma (some)
√ bright on T1WI ← subacute hematoma
√ dark on T2WI ← hemosiderin of chronic hematoma
Hypervascular Liver Mass
√ detected during hepatic arterial + portal venous phase
A. BENIGN
1. Focal nodular hyperplasia
2. Hepatocellular adenoma
3. Hemangioma (Type 1)
B. MALIGNANT
(a) Primary malignant liver tumor
1. Hepatocellular carcinoma
2. Hemangioendothelioma
3. Angiosarcoma
(b) Hypervascular liver metastases
HYPERVASCULAR MASS IN NORMAL LIVER
1. Small hemangioma (Type 1)
2. Focal nodular hyperplasia
3. Hepatocellular adenoma
4. Metastasis
HYPERVASCULAR MASS IN CHRONIC LIVER DISEASE
1. Hepatocellular carcinoma
2. Nodular regenerative hyperplasia
3. Mimickers:
AVM, FNH, hemangioma, dysplastic nodule, transient hepatic intensity difference
HYPERVASCULAR MASS WITH CENTRAL SCAR
1. Focal nodular hyperplasia
2. Giant cavernous hemangioma
3. Fibrolamellar carcinoma of liver
4. Well-differentiated hepatocellular carcinoma
5. Hypervascular metastasis
6. Intrahepatic cholangiocarcinoma
NODULE-WITHIN-NODULE ENHANCEMENT
1. Focus of early HCC within dysplastic nodule
√ moderately high SI on T2WI within nodule of generally low SI
√ marked arterial enhancement on T1WI
PERIPHERAL WASHOUT SIGN
1. Metastasis: carcinoid, breast, colon, stomach
√ hypointense peripheral rim relative to center (best seen 10 minutes after contrast administration)
DELAYED PHASE-ENHANCING LESION
1. Hemangioma
2. Intrahepatic cholangiocarcinoma
3. Peliosis hepatis
Hepatic Calcification
A. INFECTION (most common cause)
1. Granulomatous disease: tuberculosis (48%), histoplasmosis, brucellosis, coccidioidomycosis
√ calcium involves entire lesion
2. Echinococcal cyst (in 10–20%)
√ curvilinear / ring calcification
3. CMV, toxoplasmosis, Pneumocystis carinii
4. Chronic granulomatous disease of childhood
5. Old pyogenic / amebic abscess
6. Schistosomiasis
√ turtleback / tortoise shell calcifications
7. Cysticercosis, filariasis, paragonimiasis, Armillifer infection, dracunculiasis
8. Syphilitic gumma
B. VASCULAR
1. Hepatic artery aneurysm
2. Portal vein thrombosis
3. Hematoma
C. BILIARY
1. Hepatolithiasis = intrahepatic calculi
2. Recurrent pyogenic cholangitis
3. Ascariasis
4. Clonorchiasis
D. BENIGN TUMORS
1. Congenital cyst
2. Cavernous hemangioma
√ large coarse centrally located calcification (in 10–20%)
3. Hepatocellular adenoma
4. Capsule of regenerating nodules
5. Infantile hemangioendothelioma
E. PRIMARY MALIGNANT TUMOR
1. Fibrolamellar carcinoma (calcified in 15–25%)
2. Hepatocellular carcinoma
3. Hepatoblastoma (10–20%)
4. Intrahepatic cholangiocarcinoma (in 18%)
√ calcification accompanied by desmoplastic reaction
5. Epithelioid hemangioendothelioma
6. Cystadenocarcinoma
F. METASTATIC TUMOR
1. Mucin-producing neoplasm: carcinoma of colon, breast, stomach
2. Ovarian carcinoma (psammomatous bodies)
3. Melanoma, thyroid carcinoma, pleural mesothelioma, chondro- and osteosarcoma, carcinoid, leiomyosarcoma, neuroblastoma
mnemonic: 4H TAG MAP
Hepatoma
Hemochromatosis
Hemangioma
Hydatid disease
Thorotrast
Abscess
Granulomas (healed)
Metastases
Absent mnemonic
Porcelain gallbladder
Spontaneous Hepatic Hemorrhage
A. RUPTURE OF PRIMARY HYPERVASCULAR NEOPLASM
1. Hepatocellular carcinoma (86%)
2. Hepatocellular adenoma (6%)
3. Hepatic hemangioma (3%)
4. Hepatic metastasis: lung, RCC, melanoma (1%)
5. Focal nodular hyperplasia
6. Amyloidosis
7. Peliosis hepatis
8. Angiomyolipoma
(b) COAGULATION DISORDER
1. Cirrhosis (4%)
(c) SYNDROMIC HEMOLYSIS
1. HELLP syndrome
Colloid Shift
= increased uptake of injected colloid by bone marrow
A. HEPATIC DYSFUNCTION
1. Cirrhosis
2. Hepatitis
3. Chronic passive congestion
B. AUGMENTED PERFUSION of spleen + bone marrow
1. Hematopoietic disorders
2. Long-term corticosteroid therapy
Focal Hot Liver Lesion
1. IVC / SVC obstruction
√ increased perfusion of quadrate lobe located at posterior aspect of medial segment left hepatic lobe (collateral pathway via umbilical vein)
2. Budd-Chiari syndrome
√ “increased” perfusion of caudate lobe ← actually decrease of activity elsewhere in liver
3. FNH (varying amount of Kupffer cells)
√ hot (DIAGNOSTIC) / cold / isoactive with surrounding parenchyma
4. Regenerating nodules of cirrhosis
Focal Liver Defects
A. NEOPLASTIC
(a) primary liver tumor: hepatoma, hemangioma, hepatic adenoma, FNH
(b) metastases: 85% sensitive, 75–80% specific for lesion > 1–2 cm
B. INFECTIOUS DISEASE / ABSCESS
C. BENIGN CYST
D. TRAUMA (= hematoma)
E. PSEUDOTUMOR = normal variant
mnemonic: L-CHAIM
Lymphoma
Cyst
Hematoma
Abscess
Infarct
Metastasis
Mottled Hepatic Uptake
1. Cirrhosis
2. Acute hepatitis
3. Lymphoma
4. Amyloidosis
5. Granulomatous disease: sarcoidosis, fungal, viral, parasitic
6. Chemo- / radiation therapy
PORTA HEPATIS
Spectrum of Disease of Porta Hepatis
A. VASCULAR
1. Main portal vein (MPV): thrombosis, stenosis, aneurysm, gas
2. Common hepatic artery (CHA): thrombosis, stenosis, aneurysm
B. BILE DUCTS
1. Cholangiocarcinoma
2. Intrabiliary metastasis
Origin: lung, breast, gallbladder, colon, testis, prostate, pancreas, melanoma, lymphoma
3. Benign biliary stricture
4. Choledochal cyst
C. LYMPH NODES
1. Benign reactive lymph nodes
2. Noninfectious inflammatory disease
3. Infectious disease
4. Metastasis
5. Lymphoma
6. Posttransplant proliferative disease
D. NERVES
1. Schwannoma = neurilemmoma
2. Neurofibroma
3. Neurofibrosarcoma
E. CONNECTIVE TISSUE
1. Rhabdomyosarcoma
2. Granulocytic sarcoma
F. MISCELLANEOUS
2. Porta hepatis fluid collection see below
3. Periportal fat deposition
Low-density Mass in Porta Hepatis
1. Choledochal cyst
2. Hepatic cyst
3. Pancreatic pseudocyst
4. Enteric duplication
5. Hepatic artery aneurysm
6. Biloma
7. Embryonal rhabdomyosarcoma of biliary tree
Porta Hepatis Fluid Collection
Cause: orthotopic liver transplantation, trauma, cholecystectomy, other biliary injury
1. Biloma
2. Hematoma
3. Abscess
4. Seroma
Enlarged Lymph Nodes of Porta Hepatis
Location: along anterior and posterior to portal vein + hepatoduodenal ligament
Normal size: < 6 mm
A. LIVER DISEASE
1. Hepatitis B and C
2. Cirrhosis
B. INFECTION / INFLAMMATION
1. Tuberculosis
2. Autoimmune diseases
3. Sarcoidosis
C. MALIGNANCY
1. Metastasis: esophagus, stomach, pancreas, gallbladder, liver, biliary tree, breast, lung, kidney
√ may be associated with hepatic metastasis
√ compression / thrombosis of portal vein
2. Lymphoma
Defects in Porta Hepatis on Liver Scintigram
1. Normal variant ← thinning of hepatic tissue overlying portal veins + gallbladder
2. Biliary causes: dilatation of bile ducts, gallbladder hydrops
3. Enlarged portal lymph nodes
4. Metastases
5. Hepatic cyst
6. Hepatic parenchymal disease (= pseudotumor)
7. Hepatic compression by adjacent extrinsic mass
8. Postsurgical changes following cholecystectomy
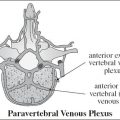
LIVER CIRCULATION
Liver perfusion
Dual blood supply: normally hepatic artery 25% + portal vein 75%
PV ↓ and HA ↑: cirrhosis & portal hypertension, portal vein thrombosis (bland, malignant), PV compression (adenopathy in porta hepatis)
PV ↑ and HA ↓: postprandial state, HA stenosis (orthotopic liver transplant) / thrombosis, HA encasement (pancreatic cancer)
Global Heterogeneous Hepatic Enhancement
1. Passive hepatic congestion
2. Budd-Chiari Syndrome
3. Hereditary hemorrhagic telangiectasia
4. Peliosis hepatis
Transient Hepatic Parenchymal Enhancement
= HYPERPERFUSION ABNORMALITIES OF LIVER
= TRANSIENT HEPATIC ATTENUATION DIFFERENCE (THAD LESION) = TRANSIENT HEPATIC INTENSITY DIFFERENCE (THID)
= attenuation difference of liver appearing during dynamic bolus-enhanced CT
√ patchy area of transient high attenuation during early arterial phase
√ fading with return to normal during portal venous phase
√ peripheral location, triangular shape, straight margins
√ presence of normal vessels coursing through lesion
Cause: imbalance between hepatic arterial + portal venous supply ← decreased portal blood flow, formation of intrahepatic arterioportal shunts, increased aberrant drainage through hepatic veins
A. LOBAR / SEGMENTAL
1. Portal vein obstruction: portal vein thrombosis, tumor invasion, surgical ligation
2. Cirrhosis with arterioportal shunt
3. Hypervascular gallbladder disease
B. SUBSEGMENTAL
1. Obstruction of peripheral portal branches
2. Percutaneous needle biopsy + drainage procedure / ethanol ablation
3. Acute cholecystitis + cholangitis
C. SUBCAPSULAR
(a) due to peripheral parenchymal compression
1. Rib compression
2. Perihepatic peritoneal implants
3. Pseudomyxoma peritonei
4. Perihepatic fluid collections
(b) idiopathic (unexplained)
D. PSEUDOLESION
= systemic venous blood flow draining into hepatic sinusoids = third hepatic inflow
1. Accessory cystic vein of gallbladder fossa
2. Aberrant right gastric vein
3. Capsular veins
4. Parabiliary venous system
5. Epigastric-paraumbilical venous system
E. RETICULAR-MOSAIC PATTERN
1. Cirrhosis
2. Hereditary hemorrhagic telangiectasia
3. Hepatic vein obstruction
Arterioportal Shunt
= organic / functional communication between high-pressure hepatic arterial branch + low-pressure portal venous system at level of trunk / sinusoids / peribiliary venules
√ small nodular peripheral nonspherical focus isoattenuating with aorta during arterial phase → isoattenuating to liver during portal phase
√ for peripheral arterioportal shunt transient wedge-shaped subsegmental area of enhancement during arterial phase → normal parenchymal attenuation during portal venous phase
Pathophysiology:
(a) shunted contrast material enhances a focal area of liver parenchyma before adjacent parenchyma is enhanced via the usual splanchnic route
(b) large shunt may cause arterialized hepatofugal flow in portal vein detectable by Doppler ultrasound
Cause:
A. CONGENITAL
1. Hereditary hemorrhagic telangiectasia
1. Cirrhosis
√ normal SI on T1WI + T2WI
√ pseudolesion = small peripheral subcapsular wedge-shaped area of transient homogeneous enhancement during arterial phase of CECT
√ pseudolesion remains stable / resolves spontaneously over time
2. Primary hepatic neoplasm: HCC (63%), hemangioma, cholangiocarcinoma
√ abnormal SI on T1WI + T2WI with growth on follow-up
√ transient wedge-shaped area of increased attenuation / intensity on arterial phase CECT / CEMR = Transient Hepatic Parenchymal Enhancement
√ enhancement of portal vein branch ± main portal vein from periphery without enhancement of splenic vein / superior mesenteric vein
3. Secondary hepatic neoplasm: metastasis
4. Hepatic trauma: blunt abdominal trauma, iatrogenic trauma (biopsy, percutaneous abscess drainage, transhepatic biliary drainage, ethanol injection)
5. Rupture of hepatic artery pseudoaneurysm into portal vein
Small arterioportal shunts 2° to cirrhosis either remain stable or resolve spontaneously, whereas those 2° to HCC generally demonstrate growth at follow-up.
Route of fistulous communication:
1. Macroscopic fistula
2. Transsinusoidal = between microscopic interlobular arteriole + portal venule
3. Transvasal = via tumor thrombus
4. Transtumoral = via draining vein from a hypervascular tumor
5. Transplexal / peribiliary = via capillary network surrounding bile ducts
DDx: HCC (hypoattenuated during portal venous and parenchymal phase; growth after repeat imaging in 6 months)
HEPATIC ARTERY
Hepatic Artery Enlargement
A high RI is not specific for liver disease; therefore, it is less meaningful as an isolated finding than is a low RI.
1. Cirrhosis → compensatory response to decreased portal venous flow
2. Intrahepatic arteriovenous shunting
(a) vascular neoplasm
(b) hepatic artery-portal vein fistula
Cause: biopsy, trauma
√ turbulent high-velocity low-resistance flow
√ soft-tissue bruit (= random assignment of color in perivascular soft tissue due to tissue vibration)
√ arterialized frequently retrograde flow in portal vein
3. Hereditary hemorrhagic telangiectasia
√ large tortuous feeding arteries with high velocity + aliased flow
√ multiple dilated vessels (representing AVMs)
√ large draining veins
√ areas of fatty change + fibrosis
4. Chronic active hepatitis
Elevated Hepatic Artery Resistance (RI > 0.7)
A. PHYSIOLOGIC
1. Postprandial state
2. Advanced age of patient
B. PATHOLOGIC
1. Chronic hepatocellular disease
2. Hepatic venous congestion
(a) acute: generalized peripheral vasoconstriction
(b) chronic: cardiac cirrhosis
3. Transplant rejection
An RI that is too high may be the result of a postprandial state, advanced patient age, or diffuse distal microvascular disease with a wide variety of causes including chronic liver disease due to cirrhosis or chronic hepatitis.
Decreased Hepatic Artery Resistance (RI < 0.55)
A. PROXIMAL ARTERIAL NARROWING
1. Transplant stenosis
2. Atherosclerotic disease
3. Arcuate ligament syndrome
B. DISTAL VASCULAR SHUNT
1. Cirrhosis with portal hypertension
2. Posttraumatic / iatrogenic
3. Hereditary hemorrhagic telangiectasia
An RI that is too low may be the result of
› proximal stenosis or
› distal vascular shunting (arteriovenous / arterioportal fistulas) as seen in severe cirrhosis;
› trauma (including iatrogenic injury); or
› Osler-Weber-Rendu syndrome.
Hepatic Artery Aneurysm
= 2nd most common type of splanchnic aneurysm = up to 20% of visceral aneurysms
Cause:
1. Atherosclerosis
2. Fibromuscular dysplasia
3. Collagen vascular disease
4. Trauma: penetrating, blunt, iatrogenic (liver transplant)
5. Mycotic aneurysm
6. Tumor-related aneurysm
7. Vasculitis (multiple aneurysms): polyarteritis nodosa
• abdominal pain (55%), gastrointestinal hemorrhage (46%)
Site: common hepatic artery (in up to 63%)
Cx: aneurysm rupture → hemobilia / hemoperitoneum (20–35% mortality rate)
Rx: endovascular stenting (89% success rate)
HEPATIC VEINS
Dampening of Hepatic Vein Doppler Waveform
= dampened oscillations of hepatic veins resembling portal vein flow ← “shielding” of hepatic veins from activity of right atrium = decreased phasicity
= “portalization” of hepatic vein flow pattern
√ drop of a wave of hepatic venous waveform below baseline
A. INCREASED LIVER TISSUE STIFFNESS
1. Liver cirrhosis
2. Various parenchymal abnormalities of liver: fatty liver, diffuse metastatic liver disease
B. INTRINSIC / EXTRINSIC VENOUS OBSTRUCTION
1. Budd-Chiari syndrome intrahepatic / suprahepatic obstruction
2. Hepatic venoocclusive disease
3. Inferior vena cava obstruction
4. Extrinsic compression of hepatic veins
5. Right-sided CHF
Irregular Flow Pattern in Hepatic Veins
1. Arrhythmia
2. Turbulent blood flow
3. Technical / patient factors: sedated patient, mechanical ventilation, SOB
Pulsatile Hepatic Doppler
= D wave greater than S wave
1. Tricuspid regurgitation
2. Right heart failure
PORTAL VEIN
Abnormal Portal Venous Flow
Pulsatile Portal Vein
= waveform pulsatility with > ²/³ change from peak velocity to minimum velocity
Pathophysiology: transmission of abnormal pressure to sinusoids via hepatic veins / arteries
A. INCREASED VENOUS PRESSURE IN SINUSOIDS (sinusoids connect portal vein with hepatic arteries and hepatic veins)
√ dilated hepatic veins
1. Tricuspid regurgitation
√ decreased S wave in hepatic venous Doppler
2. Right-sided CHF without tricuspid regurgitation
√ tall a and v waves in hepatic venous Doppler
B. ARTERIOVENOUS SHUNT
1. Arteriovenous shunt in severe cirrhosis
√ compressed hepatic veins
2. Hepatic artery-portal vein fistula
3. Portal-to-hepatic vein fistula
4. Hereditary hemorrhagic telangiectasia (rare) → arteriovenous fistulas
Slow Portal Venous Flow
Pathophysiology: back pressure limits forward velocity
Cause:
Portal hypertension: peak velocity < 16 cm/sec
(a) prehepatic: portal vein thrombosis
(b) intrahepatic: cirrhosis from any cause
(c) posthepatic: right-sided heart failure, tricuspid regurgitation, Budd-Chiari syndrome
Hepatofugal (Retrograde) Portal Venous Flow
= waveform below the baseline
Pathophysiology: back pressure exceeds forward pressure with flow subsequently reversing direction
Cause: severe portal hypertension from any cause
Absent / Aphasic Portal Venous Flow
A. STAGNANT PORTAL VENOUS FLOW
1. Severe portal hypertension with neither hepatopetal nor hepatofugal flow → at risk for portal vein thrombosis
B. OCCLUSION OF PORTAL VEIN
√ cavernous transformation = development of collateral vessels in / around occluded portal vein
1. Bland portal vein thrombus
2. Malignant invasion of portal vein (= tumor thrombus)
√ “thread & streak” sign = color signal with arterial (pulsatile) waveform within thrombus
Periportal Hypoattenuating Halo
= accumulation of lymph around the portal tract
1. Edema: CHF, acute hepatitis, hepatic venoocclusive disease
2. Infiltration: lymphoma, extramedullary hematopoiesis
3. Lymphatic dilatation ← obstruction in porta hepatis by enlarged nodes / mass / in liver transplant
4. Hemorrhage (asymmetric involvement)
5. Fat accumulation
Periportal Lymphedema
= ill-defined hypodensity at porta hepatis / hypodensity parallel to portal vein
1. Acute hepatitis
2. Cirrhosis
3. Hepatic venoocclusive disease
4. Liver / bone marrow transplant
5. Overhydration
6. Blunt abdominal trauma ± liver injuries
7. Chronic congestive heart failure
8. Cardiac tamponade
9. Malignancy: hepatic / retroperitoneal
Portosystemic Shunt
A. EXTRAHEPATIC PORTOSYSTEMIC SHUNT
(a) congenital (rare)
(b) acquired (most common)
Cause: portal venous hypertension
B. INTRAHEPATIC PORTOSYSTEMIC SHUNT (rare)
C. ARTERIOPORTAL SHUNT
D. PERSISTENT DUCTUS VENOSUS
Portal Venous Stenosis
Cause:
1. Tumor encasement: locally recurrent periampullary cancers = pancreatic carcinoma, hepatocellular carcinoma, cholangiocarcinoma, metastasis
2. Inflammation: acute pancreatitis
3. Surgical complication: liver transplantation (1%), partial hepatectomy, pancreaticoduodenectomy
4. Radiation therapy
√ focal segment of vessel narrowing ± poststenotic dilatation
√ inhomogeneous peripheral subcapsular increase in arterial inflow during hepatic arterial phase
√ secondary portal hypertension → increased number and size of collaterals
US:
√ focal color aliasing
√ accelerated flow across stenosis = 4-fold velocity gradient
√ spectral broadening of waveform (= poststenotic turbulence)
Cx: portal venous hypertension with massive intractable ascites + recurrent variceal bleeding
Rx: balloon angioplasty, stent placement
Portal Venous Gas
◊ Should be considered a life-threatening event and sign of bowel infarction + gangrene until proved otherwise!
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree