into subcutaneous tissue
Breast Edema
1. Lymphatic obstruction: extensive axillary / intrathoracic lymphadenopathy, mediastinal / anterior chest wall tumor, axillary surgery, SVC syndrome, filariasis, intestinal lymphangiectasia
2. Skin disorder: psoriasis, burns
3. Generalized body edema: congestive heart failure (breast edema may be unilateral if patient in lateral decubitus position), hypoalbuminemia (renal disease, liver cirrhosis), fluid overload
Abnormal Uptake of Bone Agents within Breast
1. Breast carcinoma
2. Prosthesis
3. Drug-induced
MAMMOGRAPHIC RISK ASSESSMENT
for invasive breast carcinoma
A. NO INCREASED RISK
1. Nonproliferative lesions: adenosis, florid adenosis, apocrine metaplasia without atypia, macro- / microcysts, duct ectasia, fibrosis, mild hyperplasia (more than 2 but not more than 4 epithelial cells deep), mastitis, periductal mastitis, squamous metaplasia
2. Fibroadenoma
B. PROLIFERATIVE LESIONS WITHOUT ATYPIA
Relative risk increase: 1.5–2.0
1. Columnar cell change / hyperplasia = blunt duct adenosis
2. Moderate + florid solid / papillary hyperplasia without atypia
3. Sclerosing adenosis
4. Intraductal papilloma with fibrovascular core
5. Pseudoangiomatous stromal hyperplasia (PASH)
6. Radial sclerosing lesion
C. PROLIFERATIVE LESIONS WITH ATYPIA
Relative risk increase: 4–5
1. Atypical ductal hyperplasia (ADH)
2. Lobular neoplasia: separation based on degree of distension of affected terminal ductules:
(a) Atypical lobular hyperplasia (ALH)
(b) Lobular carcinoma in situ (LCIS)
BREAST LESION
Mammographic Evaluation of Breast Masses
True mass or pseudomass?
A. SIZE
› well-defined nodules < 1.0 cm are of low risk for cancer
› “most likely benign” nodules approaching 1 cm should be considered for ultrasound / aspiration / biopsy
B. SHAPE
› increase in probability of malignancy: architectural distortion > irregular > lobulated > oval > round
C. MARGIN / CONTOUR (most important factor)
› well-circumscribed mass with sharp abrupt transition from surrounding tissue is almost always benign
› “halo” sign of apparent lucency = optical illusion of Mach effect + true radiolucent halo is almost always (92%) benign but NOT pathognomonic for benignity
› microlobulated margin worrisome for cancer
› obscured margin may represent infiltrative cancer
› irregular ill-defined margin has a high probability of malignancy
› spiculated margin due to
(a) fibrous projections extending from main cancer mass
(b) previous surgery
(c) sclerosing duct hyperplasia (radial scar)
D. LOCATION
› intramammary lymph node typically in upper outer quadrant (in 5% of all mammograms)
› large hamartoma + abscess common in retro- / periareolar location
› sebaceous cyst in subcutaneous tissue
E. X-RAY ATTENUATION = DENSITY
› fat-containing lesions are never malignant
› high-density mass suspicious for carcinoma (density higher than for equal volume of fibroglandular tissue ← fibrosis)
F. NUMBER
› multiplicity of identical lesions decreases risk
G. INTERVAL CHANGE
› enlarging mass needs biopsy
H. PATIENT RISK FACTORS
› increasing age increases risk for malignancy
› positive family history
› history of previous abnormal breast biopsy
› history of extramammary malignancy
Focal Asymmetry
Definition:
= asymmetry confined to less than a quadrant
(a) lesion with definable borders only seen on 1 view
(b) lesion of similar shape on 2 orthogonal views lacking convex margins + conspicuity of a true mass
A real lesion may not be included in the field of view of the orthogonal view!
Cause:
1. Pseudolesion (in 2% of screening mammograms)
= summation artifact of overlapping breast tissue
2. Breast cancer
◊ A focal asymmetry is a malignancy in only 1–3%
◊ A developing / new focal asymmetry represents a malignancy in 6–27%
◊ In 9–38% missed cancers were retrospectively visible as a focal asymmetry
A 1-view lesion is of concern if associated with: outward convex margins / straight lines of architectural distortion or spiculation / microcalcifications / palpability
Dense fibroglandular tissue may obscure a real lesion on the orthogonal view!
Histo: invasive lobular carcinoma (in 33%), invasive ductal carcinoma
Well-circumscribed Breast Mass
◊ Well-defined nonpalpable lesions have a 4% risk of malignancy!
A. BENIGN
1. Cyst (45%)
2. Fibroadenoma
3. Sclerosing adenoma
4. Intraductal papilloma (intracystic / solid)
5. Galactocele
6. Sebaceous cyst
7. Pseudoangiomatous stromal hyperplasia
B. MALIGNANT
1. Medullary carcinoma
2. Mucinous carcinoma
3. Intracystic papillary carcinoma
4. Invasive ductal cancer not otherwise specified (rare)
5. Pathologic intramammary lymph node
6. Metastases to breast: melanoma, lymphoma / leukemia, lung cancer, hypernephroma
De Novo Mass in Woman > 40 Years of Age
1. Cyst
2. Papilloma
3. Carcinoma (10–20%)
(a) Invasive ductal carcinoma (not otherwise specified)
(b) Mucinous carcinoma
(c) Medullary carcinoma
(d) Intracystic papillary carcinoma
(e) Invasive papillary carcinoma
(f) Metaplastic carcinoma
(g) Malignant phyllodes tumor
(h) Adenoid cystic carcinoma
4. Sarcoma (rare)
5. Fibroadenoma (exceedingly rare)
6. Metastasis (extremely rare)
Fibrous Breast Lesion
1. Fibroadenoma
2. Phyllodes tumor
3. Sclerosing lobular hyperplasia
4. Pseudoangiomatous stromal hyperplasia
5. Diabetic mastopathy
6. Focal fibrosis
7. Fibromatosis
Fat-containing Breast Lesion
◊ Fat contained within a lesion usually proves benignity!
1. Lipoma
2. Galactocele
= fluid with high lipid content (last phase)
• during / shortly after lactation
3. Oil cyst= traumatic lipid cyst = fat necrosis
• site of prior surgery / trauma
4. Focal collection of normal breast fat
Mixed Fat- and Water-density Lesion
1. Fibroadenolipoma / hamartoma
2. Intramammary lymph node
3. Galactocele
4. Hamartoma = lipofibroadenoma = fibroadenolipoma
5. Small superficial hematoma
6. Cancer engulfing fat
√ irregular / spiculated margins]
Secretory Disease
1. Retained lactiferous secretions
= incomplete / prolonged involution of lactiferous ducts
√ branching pattern of fat density in dense breast (high lipid content)
2. Prolonged inspissation of secretion + intraductal debris
= Mammary duct ectasia
3. Galactocele
4. Plasma cell mastitis
Breast Lesion with Halo Sign
A. HIGH-DENSITY LESION
= vessels + parenchymal elements not visible in superimposed lesion
1. Cyst
2. Sebaceous cyst
3. Wart
B. LOW-DENSITY LESION
= vessels + parenchyma seen superimposed on lesion
1. Fibroadenoma
2. Galactocele
3. Cystosarcoma phylloides
Stellate / Spiculated Breast Lesion
= mass / architectural distortion characterized by thin lines radiating from its margins
› The majority of invasive breast cancers are stellate (stellate÷circular = 65÷35)
› 93% of all stellate lesions are malignant
Risk of malignancy:
› 75% for nonpalpable spiculated masses
› 32% for nonpalpable irregular masses
A. PSEUDOSTELLATE STRUCTURE
= SUMMATION SHADOW / ARTIFACT
caused by fortuitous superimposition of normal fibrous + glandular structures; unveiled by rolled views, spot compression views ± microfocus magnification technique
B. “BLACK STAR”
√ groups of fine straight / curvilinear fibrous strands bunched together like a broom
√ circular / oval lucencies within center
√ change in appearance from view to view
1. Radial scar = sclerosing duct hyperplasia (86%)
2. Sclerosing adenosis
3. Posttraumatic fat necrosis (11%)
C. “WHITE STAR”
√ individual straight dense spicules
√ central solid tumor mass
√ little change in different views
(a) malignant lesions
1. Invasive ductal carcinoma (65%) = scirrhous carcinoma
= desmoplastic reaction + secondary retraction of surrounding structures
• clinical dimensions > mammographic size
√ distinct central tumor mass with irregular margins
√ length of spicules increase with tumor size
√ localized skin thickening / retraction when spiculae extend to skin
√ commonly associated with malignant-type calcifications
2. Invasive lobular carcinoma (21%)
• palpable mass
√ lack of central tumor mass
3. Tubular carcinoma (9%)
4. Other (5%)
(b) benign lesions
1. Postoperative scar
• correlation with history + site of biopsy
√ scar diminishes in size + density over time
2. Postoperative hematoma
• clinical information
√ short-term mammographic follow-up confirms complete resolution
3. Breast abscess
• clinical information
√ high-density lesion with flamelike contour
4. Hyalinized fibroadenoma with fibrosis
√ changing pattern with different projections
√ may be accompanied by typical coarse calcifications of fibroadenomas
5. Granular cell myoblastoma
6. Fibromatosis
7. Extra-abdominal desmoid
mnemonic: STARFASH
Summation shadow
Tumor (malignant)
Abscess
Radial scar
Fibroadenoma (hyalinized), Fat necrosis
Adenosis (sclerosing)
Scar (postoperative)
Hematoma (postoperative)
Tumor-mimicking Lesions
1. “Phantom breast tumor” = simulated mass
(a) asymmetric density
√ scalloped concave breast contour
√ interspersed fatty elements
(b) summation artifact = chance overlap of normal glandular breast structures
√ failure to visualize “tumor” on more than one view
2. Silicone injections
3. Skin lesions
(a) Dermal nevus
√ sharp halo / fissured appearance
(b) Skin calcifications
√ lucent center (= clue)
√ superficial location (tangential views)
(c) Sebaceous / epithelial inclusion cyst
(d) Neurofibromatosis
(e) Biopsy scar
5. Lymph nodes
Frequency: 5.4% for intramammary nodes
Location: axilla, subcutaneous tissue of axillary tail, lateral portion of pectoralis muscle, intramammary (typically in upper outer quadrant)
√ ovoid / bean-shaped mass(es) with fatty notch representing hilum
√ central zone of radiolucency (fatty replacement of center) surrounded by “crescent” rim of cortex
√ usually < 1.5 cm (up to 4 cm) in size
√ well-circumscribed with slightly lobulated margin
US:
√ reniform hypoechoic rim with echogenic center
√ echogenic hilum for entry and exit of vessels
6. Hemangioma
Solid Breast Lesion by Ultrasound
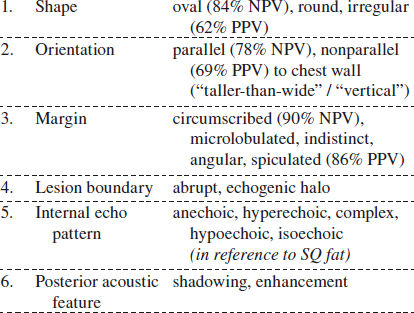
Morphologic Descriptors of Solid Benign Breast Mass
Posterior Acoustic Shadowing
1. Invasive carcinoma
2. Postoperative scar
3. Complex sclerosing lesion
4. Microcalcifications
5. Dense breast tissue
Posterior Acoustic Enhancement
1. Normal anatomic structure
2. Cyst: simple / complicated
3. Fibroadenoma
4. Nodular sclerosing adenosis
5. Papilloma
6. Complex cystic mass
7. Invasive ductal carcinoma
8. Lymphoma
Echogenic Breast Lesion
Incidence: 0.6–5.6% of breast masses
◊ Hyperechogenicity alone does not allow exclusion of malignancy!
A. Benign
1. Lipoma
2. Angiolipoma
3. Hematoma
4. Seroma
5. Fat necrosis
6. Silicone granuloma
7. Sebaceous / epidermal inclusion cyst
8. Abscess
9. PASH
10. Galactocele / lactating adenoma
11. Ductal ectasia
12. Apocrine metaplasia
An echogenic mass that correlates with a well-delineated radiolucent mass at mammo is benign!
B. Malignant
1. Invasive ductal carcinoma
2. Invasive lobular carcinoma
3. Metastasis
4. Lymphoma
5. Angiosarcoma
Breast carcinoma is RARELY purely echogenic!
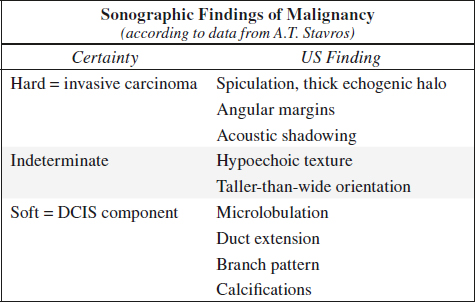
Malignant Sonographic Characteristics
◊ Approximately 5 malignant features are found per cancer. The combination of 5 findings increases the sensitivity to 98.4%!
√ spiculation = straight lines radiating perpendicularly from surface of tumor:
√ coarse spiculation (less common) = hypoechoic lines (= fingers of invasive tumor / DCIS) alternating with hyperechoic lines (= interface between tumor and surrounding tissue)
√ fine spiculation (more common):
√ hyperechoic spicules in fatty tissue
√ hypoechoic spicules in fibrous tissue
√ thick echogenic halo = spicules too small to resolve
√ angular margins = contour of junction between hypo- or isoechoic solid nodule and surrounding tissue at acute / obtuse / 90° angles
√ acoustic shadowing behind all / part of nodule (= desmoplastic reaction as host response to tumor)
√ taller-than-wide lesion (feature of small lesions)
= AP dimension greater than craniocaudal / transverse dimension
√ microlobulations = many small lobulations at surface of solid nodule (= duct distended with DCIS / cancerized lobule)
√ duct extension (= intraductal growth of breast cancer in single large duct extending toward nipple)
√ branch pattern (= intraductal growth of breast cancer in multiple small ducts extending away from nipple)
√ hypoechoic texture = central part of solid lesion markedly hypoechoic with respect to fat ← invasive tumor mass / fluid within tumor / acoustic shadow
√ punctate echogenic calcifications within hypoechoic duct extension / branch pattern / microlobulations (acoustic shadowing commonly not present)
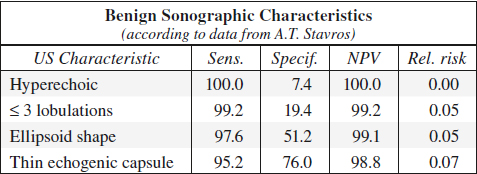
Benign Sonographic Characteristics
√ absence of any malignant characteristics
◊ A single malignant feature prohibits classification of a nodule as benign!
√ marked hyperechogenic well-circumscribed nodule compared with fat = normal stromal fibrous tissue (may represent a palpable pseudomass / fibrous ridge)
√ smooth well-circumscribed ellipsoid shape
√ 2–3 smooth well-circumscribed gentle lobulations
√ thin echogenic capsule
√ kidney-shaped lesion = intramammary lymph node
◊ If specific benign features are not found the lesion is classified as indeterminate!
Complex Cystic Breast Mass
= cyst with thick wall, thick septa, intracystic discrete solid components
Classification:
Type 1 thick outer wall ± thick internal septa
Type 2 one / more intracystic masses
Type 3 mixed cystic (> 50%) and solid components
Type 4 predominantly solid + eccentric cystic foci
(a) benign breast lesion
1. Fibrocystic changes: adenosis, sclerosing adenosis, apocrine metaplasia, cyst formation ± rupture, ductal ectasia
2. Intraductal / intracystic papilloma
3. Fibroadenoma
4. Breast varix
(b) atypical (high-risk) breast lesion
1. Atypical ductal hyperplasia
2. Atypical papilloma
3. Lobular neoplasia
(c) malignant breast lesion
1. DCIS
2. Infiltrating ductal carcinoma
3. Infiltrating lobular carcinoma
MALE BREAST DISEASE
Benign Male Breast Disease
1. Gynecomastia
2. Lipoma
3. Pseudoangiomatous stromal hyperplasia
4. Granular cell tumor
5. Fibromatosis / desmoid tumor
6. Myofibroblastoma
7. Schwannoma
8. Hemangioma
Malignant Male Breast Disease
A. CARCINOMA
1. Invasive ductal carcinoma
Incidence: 0.17% of all male breast cancers
Mean age: 59 years
√ microcalcifications in only 13–30%
2. Papillary carcinoma
3. Invasive lobular carcinoma
4. Adenoid cystic carcinoma
B. SARCOMA
1. Liposarcoma
2. Dermatofibrosarcoma
3. Pleomorphic hyalinizing angiectatic tumor
C. OTHERS
1. Basal cell carcinoma of nipple
2. Lymphoma / leukemia
= most common hematopoietic disease of the breast
√ axillary lymphadenopathy: unilateral in primary / bilateral in secondary breast lymphoma
3. Metastasis
BREAST CALCIFICATIONS
= deposits of calcium salts
(a) precipitated salts in accumulated fluid secreted by epithelial cells
b) in / on necrotic cells
(c) fibrous capsule of foreign object
Indicative of focally active process; often requiring biopsy
◊ 75–80% of biopsied clusters of calcifications represent a benign process
◊ 10–30% of microcalcifications in asymptomatic patients are associated with cancers
Composition: hydroxyapatite / tricalcium phosphate / calcium oxalate
Results of breast biopsies for microcalcifications:
(without any other mammographic findings)
(a) benign lesions (80%)
1. Mastopathy without proliferation 44%
2. Mastopathy with proliferation 28%
3. Fibroadenoma 4%
4. Solitary papilloma 2%
5. Miscellaneous 2%
(b) malignant lesions (20%)
1. Lobular carcinoma in situ 10% in 8% no spatial relationship to LCIS
2. Infiltrating carcinoma 6%
3. Ductal carcinoma in situ 4%
◊ A positive biopsy rate of > 35% is desirable goal!
A. LOCATION
(a) intramammary
1. Ductal microcalcifications
√ 0.1–0.3 mm in size, irregular, sometimes mixed linear + punctate
Occurrence: secretory disease, epithelial hyperplasia, atypical ductal hyperplasia, intraductal carcinoma
2. Lobular microcalcifications
√ smooth round, similar in size + density
Occurrence:
cystic hyperplasia, adenosis, sclerosing adenosis, atypical lobular hyperplasia, lobular carcinoma in situ, cancerization of lobules (= retrograde migration of ductal carcinoma to involve lobules), ductal carcinoma obstructing egress of lobular contents
N.B.: lobular and ductal microcalcifications occur frequently in fibrocystic disease + breast cancer!
(b) extramammary: arterial wall, duct wall, fibroadenoma, oil cyst, skin, etc.
B. SIZE
◊ Mammography detects calcifications > 100 µg; down to ~ 75 µg for spot magnification views
√ malignant calcifications usually < 0.5 mm; rarely > 1.0 mm
√ < 4–5 calcifications per 1 cm2 have a low probability for malignancy
D. MORPHOLOGY
(a) benign
1. Smooth round calcifications: formed in dilated acini of lobules
2. Solid / lucent-centered spheres: usually ← fat necrosis
3. Crescent-shaped calcifications that are concave on horizontal beam lateral projection = sedimented milk of calcium at bottom of cyst
4. Lucent-centered calcifications: around accumulated debris within ducts / in skin
5. Solid rod-shaped calcifications / lucent-centered tubular calcifications: formed within / around normal / ectatic ducts
6. Rimlike / eggshell calcifications in rim of breast cyst, fibrous wall of fat necrosis (“oil cyst”), pseudocapsule of fibroadenoma
7. Calcifications with parallel track appearance = vascular calcifications
(b) malignant
= calcified cellular secretions / necrotic cancer cells within ducts
√ calcifications of vermicular form, varying in size, of linear / branching shape
E. DISTRIBUTION
1. Clustered heterogeneous calcifications: adenosis, peripheral duct papilloma, hyperplasia, cancer
2. Segmental calcifications within single duct network: suspect for multifocal cancer within lobe
3. Regional / diffusely scattered calcifications with random distribution throughout large volumes of breast: almost always benign
F. TIME COURSE
malignant calcifications can remain stable for > 5 years!
G. DENSITY
Malignant Calcifications
1. Granular calcifications = resembling fine grains of salt
√ amorphous, dotlike / elongated, fragmented
√ grouped very closely together
√ irregular in form, size, and density
2. Casting calcifications = fragmented cast of calcifications within ducts
√ variable in size + length
√ great variation in density within individual particles + among adjacent particles
√ jagged irregular contour
√ ± Y-shaped branching pattern
√ clustered (> 5 per focus within an area of 1 cm2)
Benign Calcifications
1. Lobular calcifications = arise within a spherical cavity of cystic hyperplasia, sclerosing adenosis, atypical lobular hyperplasia
√ sharply outlined homogeneous solid spherical “pearl-like”
√ little variation in size
√ numerous + scattered
√ associated with considerable fibrosis
(a) adenosis
√ diffuse calcifications involving both breasts symmetrically
(b) periductal fibrosis
√ diffuse / grouped calcifications + irregular borders, simulating malignant process
2. Sedimented milk of calcium
Frequency: 4%
√ multiple bilateral scattered / occasionally clustered calcifications within microcysts
√ smudge-like particles (“cotton balls”) at bottom of cyst on vertical beam (CC image)
√ crescent-shaped on horizontal projection = “teacup-like” (ML / MLO image)
3. Plasma cell mastitis = periductal mastitis
√ sharply marginated calcifications of uniform density = intraductal form
√ sharply marginated hollow calcifications = periductal form
4. Peripheral eggshell calcifications
(a) with radiolucent lesion
› liponecrosis micro- / macrocystica calcificans (= fatty acids precipitate as calcium soaps at capsular surface) as calcified fat necrosis / calcified hematoma
◊ May mimic malignant calcifications!
(b) with radiopaque lesion
› degenerated fibroadenoma
› macrocyst
√ high uniform density in periphery
√ usually subcutaneous
√ no associated fibrosis
5. Papilloma
√ solitary raspberry configuration in size of duct
√ central / retroareolar
6. Degenerated fibroadenoma
√ bizarre, coarse, sharply outlined, “popcornlike” very dense calcification within dense mass (= central myxoid degeneration)
√ eggshell type calcification (= subcapsular myxoid degeneration)
√ heterogeneously grouped macrocalcifications with circumferential nature in postmenopausal woman
7. Arterial calcifications
√ parallel lines of calcifications
8. Metastatic calcifications
Cause: 2° hyperparathyroidism (in up to 68%)
Dermal Calcifications
Site: hair follicle, nevus, sebaceous cyst, lupus erythematosus, dermatomyositis, scar
Cause: inspissated material in sebaceous glands, secondary to chronic folliculitis
Location: most commonly visible in lower inner breast
Site: near periphery of skin surface (may project deep within breast even on 2 views at 90° angles)
Size: same size as skin pores
√ round lucent centered calcifications:
√ hollow radiolucent center (hair follicle)
√ linear orientation when caught in tangent
√ polygonal shape
Proof: superficial marking technique (= skin localization work-up)
Dystrophic Calcifications
= calcium deposits on / in necrotic material, cellular debris, devitalized tissue
| (a) skin: | lupus erythematosus, dermatomyositis, scar, parasite, breast implant |
| (b) foreign body: | suture, parasite, breast implant |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree