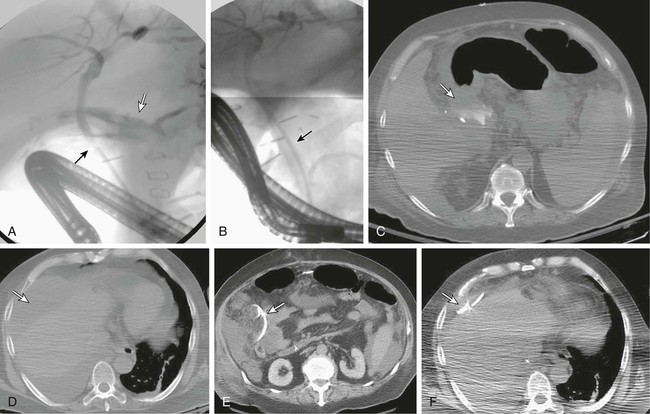
Orthotopic liver transplantation (OLT) is a critical therapeutic alternative for managing patients with progressive liver failure and selected patients with hepatocellular carcinoma. Refinements in surgical technique, improved immunosuppressive agents, and the evolution of minimally invasive image-guided procedures have allowed 5-year survival rates to approach 85%.1–3 The most common source of a replacement organ is a deceased donor. Usually the whole liver is used as the allograft, but the donor organ can be split, with the right lobe or right lobe and medial segment of the left lobe donated to an adult and the left lateral segment given to a child.4–6 Unfortunately, there remains a critical shortage of donor organs when compared with the number of patients on the liver transplant waiting list. This shortage of organs stimulated the development of using right and left hepatic lobes from living donors with matching ABO blood types for urgent transplantation. Despite the use of living donors, the availability of organs falls well short of the demand, and up to 50% of potential recipients die while awaiting transplantation.7,8 As with any complex surgical procedure, complications after orthotopic liver transplantation are not infrequent and occur in both the acute postoperative period and months to years later. The most common source of significant complications in a liver transplant patient is the biliary tract.9–12 To understand the types of complications that occur, thorough comprehension of the surgical anatomy is essential. The type of biliary anastomosis created depends on several factors,13,14 including whether a whole cadaveric liver or a split liver has been used, the condition of the recipient’s bile duct, and whether it is an adult or pediatric patient receiving the allograft. The CDCD anastomosis may be performed over a T-tube. If a T-tube is placed, postoperative bile production can be monitored and the biliary tree can be investigated easily by T-tube cholangiography. Moreover, the presence of the T-tube may make the anastomosis technically easier to create. However, because of complications associated with T-tube placement, as well as biliary leakage after tube removal, many centers have abandoned routine T-tube placement during creation of a CDCD anastomosis.15–17 A recent meta-analysis suggests that biliary complications may not be increased by T-tube insertion, however, and suggests the incidence of biliary strictures may be reduced.18 When a CDCD anastomosis is not the optimal surgical option, a CDJ or hepaticojejunostomy is constructed.19,20 These anastomoses are created by attaching the end or obliquely cut side (to create a larger channel) of the common bile duct or common hepatic duct to the side of a loop of jejunum pulled up to the region of the porta hepatis in a Roux-en-Y configuration. This maneuver requires surgical closure of the free end of the jejunal loop adjacent to the biliary anastomosis, as well as distal jejunojejunostomy to maintain continuity of the alimentary tract. Numerous variations in biliary anatomy exist, with so-called normal anatomy being present in only 57% of patients.20 “Normal” anatomy is considered to be a common hepatic duct bifurcating into left and right hepatic ducts, and the right duct subsequently bifurcating into anterior and posterior segmental ducts. A trifurcation of the common hepatic duct into left, right anterior segmental, and right posterior segmental ducts is observed in 12%. Other common variations include origin of the right anterior or posterior segmental ducts from either the common hepatic duct or the left hepatic duct. Rarely, the right posterior or anterior segmental duct joins the cystic duct prior to its entry into the extrahepatic bile duct. When variant biliary anatomy is present in the right lobe of the donor organ and it is desirable to create anastomoses to the recipient bile duct, unconventional anastomoses may be required, including the donor segmental right hepatic duct anastomosed to the recipient’s left hepatic duct or cystic duct.21,22 As an alternative, separate biliary-enteric anastomoses to a Roux-en-Y loop can be created. In some cases, the segmental duct is ligated, and that segment of the liver subsequently atrophies. When living donor transplantation is being considered, presurgical evaluation of the potential donor is performed so that the biliary and vascular anatomy can be delineated prior to transplantation. Accurate assessment of the biliary anatomy is critical in living donor transplantation because a biliary injury potentially has great significance. Complications related to the biliary tree are encountered in 4.4% of donor hepatectomies.23 The optimal method for preoperative anatomic evaluation of potential living hepatic donors remains to be defined. The ideal technique would clearly delineate the hepatic arteries, portal veins, hepatic veins, bile ducts, and hepatic parenchyma without requiring contrast media or ionizing radiation. Although magnetic resonance imaging (MRI) and MR angiography (MRA) potentially fulfill some of these requirements, delineation of small hepatic arteries and diminutive biliary radicles can be problematic.24 Three-dimensional reconstruction renderings will usually provide adequate information for surgical planning. A more detailed biliary evaluation would be advantageous, but the risks associated with retrograde cholangiography are considered excessive for routine evaluation of a healthy living donor. The surgical anastomosis between the donor biliary tract and the recipient may be technically difficult to create. Moreover, the biliary system is sensitive to ischemia and may be damaged either by prolonged preservation before transplantation or by problems with either hepatic arterial and possibly portal venous flow.25 Despite refinements in surgical technique, biliary complications continue to be a common source of morbidity in the transplant patient. In a systematic review of 14,359 transplants, biliary complications were observed in 12% of deceased donor recipients and 19% of live donor grafts.11 Two major types of complications related to the biliary tract are observed: bile leak and biliary obstruction. In a patient with a CDCD anastomosis performed over a T-tube, seepage through the T-tube choledochostomy is the most common cause of a bile leak.26 This type of leak is usually identified on routine postoperative T-tube cholangiography. Initial treatment consists of opening the T-tube to gravity drainage, which is curative in up to 60% of patients.27 If this is unsuccessful, endoscopic sphincterotomy may be useful. Bile leaks may also develop when the T-tube is removed 3 to 6 months after the transplant operation. Immunosuppression often prevents formation of a connective tissue tract to allow bile to drain freely into the peritoneal cavity. Retrograde stent placement or percutaneous transhepatic drainage coupled with percutaneous drainage of the biloma controls the leak in most patients. However, up to a third of these patients require operative intervention with surgical revision for closure.28 Because of the aforementioned problems related to T-tubes, some centers have elected to perform the CDCD anastomosis without T-tube insertion. In a study by Randall et al.,29 a group of 59 patients who had T-tubes placed were compared with 51 patients who underwent CDCD anastomoses without T-tubes. This comparison revealed no difference in biliary complication rates or survival. Bile leaks that occur at the anastomotic site (Fig. 139-1) may be difficult to manage conservatively. The principles of nonoperative management of bile leaks include (1) exclusion of hepatic artery thrombosis or stenosis, (2) drainage of any associated bilomas or abscesses, (3) diversion of bile flow, (4) eradication of any coexistent infection, and (5) optimization of the nutritional status of the patient. Patency of the hepatic artery should be confirmed in all patients with a bilious postoperative collection. This is usually accomplished with duplex ultrasound though MRA, or CTA may be used when the ultrasound examination is inconclusive. When hepatic artery thrombosis (HAT) is detected, retransplantation may be required. Kaplan et al.30 reported percutaneous drainage in 15 patients with hepatic artery occlusion; 11 required retransplantation, and 4 were managed for more than 30 months with indwelling drainage catheters. Management of bilomas in a transplant patient is identical to that in a nontransplant patient, and consists of image-guided percutaneous drainage for accessible collections in the majority of patients. The most common area in which a biloma develops is adjacent to the extrahepatic biliary system in the subhepatic space. However, the bile may track and accumulate some distance from the site of leakage. The right subphrenic space is not an uncommon site, particularly if the size of the allograft is poorly matched to the configuration of the right subphrenic space. The right subphrenic space offers unique challenges for percutaneous drainage because of its location. Frequently a choice must be made between a transhepatic approach, which can potentially lead to damage to the allograft, and a transpleural approach, which may potentially contaminate the pleural space. Overall, percutaneous drainage of postoperative bile collections in a liver transplant patient carries high success and low complication rates.31 With these principles, it may be possible to treat anastomotic leaks nonoperatively. Osorio et al.15 reported successful healing of 14 of 17 CDCD anastomotic leaks; 3 of 17 CDCD anastomoses that were entirely dehiscent required operative revision. In this same series, only 3 of 9 bile leaks originating from CDJ anastomoses healed with conservative therapy. Patients with split-liver transplants (either deceased or living donor) deserve special consideration.32–34
Biliary Complications Associated with Liver Transplantation
Surgical Anatomy of the Biliary Anastomosis
Whole Liver
Split Liver
Biliary Complications
Bile Leak
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Biliary Complications Associated with Liver Transplantation