Percutaneous vertebral augmentation is a successful means of relieving pain and reducing disability after vertebral compression fracture; however, the exact mechanism by which vertebral augmentation eliminates pain remains unproven. Most likely, pain relief is because of stabilization of microfractures. The biomechanical effects of vertebral fracture and subsequent vertebral augmentation therapy, however, are topics for continued investigation. Altered biomechanical stresses after treatment may affect the risk of adjacent fracture in an osteoporotic patient; that risk may be different after vertebral augmentation with cavity creation (balloon assisted vertebroplasty or kyphoplasty) when compared with vertebral augmentation without cavity creation (vertebroplasty). Polymethyl methacrylate cement used in these procedures may have an important effect on the load transfer and disk mechanics, and therefore, the variables of cement volume, formulation, and distribution should also be evaluated. Finally, the question of whether prophylactic treatment of adjacent intact levels is indicated must be considered.
The primary goal of percutaneous vertebral augmentation is to provide relief from vertebrogenic pain associated with a pathologic compression fracture or marrow infiltration. These processes may be related to either primary or secondary osteoporosis or benign or malignant neoplasm. Percutaneous vertebral augmentation may prevent further collapse of the fractured vertebral body, which leads to further loss of height, fractures at adjacent levels, and progressive kyphosis. In addition, patients with vertebral compression fracture have a 23% to 34% increase in mortality rate compared with patients without fracture; the most common cause of death in these patients is pulmonary disease, including chronic obstructive pulmonary disease and pneumonia.
Percutaneous vertebral augmentation is a successful means of relieving pain and reducing disability after vertebral compression fracture ; however, the exact mechanism by which vertebral augmentation eliminates pain remains unproven. Most likely, pain relief is due to stabilization of microfractures. The biomechanical effects of vertebral fracture and subsequent vertebral augmentation therapy, however, are topics for continued investigation. Altered biomechanical stresses after treatment may affect the risk of adjacent fracture in an osteoporotic patient; that risk may be different after vertebral augmentation with cavity creation (balloon assisted vertebroplasty or kyphoplasty) versus vertebral augmentation without cavity creation (vertebroplasty). Polymethyl methacrylate (PMMA) cement used in these procedures may have an important effect on the load transfer and disk mechanics, and therefore, the variables of cement volume, formulation, and distribution should also be evaluated. Finally, the question of whether prophylactic treatment of adjacent intact levels is indicated must be considered.
Biomechanics
A fundamental understanding of the regional biomechanics is essential when considering the osteoporotic spine and the effects of vertebral augmentation. Under physiologic conditions, load is shared by the vertebrae, disks, ligaments, facet joints, and, in the thoracic region, the ribs and sternum. Compressive load is generated by the weight of the body segments and the action of the trunk muscles. When devising experimental models of the spine, preservation of these nonosseous components is essential for the validity of some ex vivo models. Experimental models that study a functional unit of the spine comprising multiple vertebral body levels and their supporting structures may therefore be most relevant.
Two major factors likely contribute to anterior vertebral body stress and increased potential for adjacent level fractures after an initial vertebral compression fracture: anterior load shift and changes in load transfer through the intervertebral disk. Kyphosis from a vertebral compression fracture causes an anterior shift of the compressive load path in the fractured as well as the adjacent unfractured vertebral bodies by increasing the moment arm. In an osteoporotic vertebral body, this can increase peak stresses by up to 2.5 times. With endplate fracture, load transfer through the disk is altered as the volume of space occupied by the nucleus pulposus increases; the nucleus is then unable to increase pressure during flexion. Because of this loss of a cushion effect, the anterior annulus and apophyseal ring bear more load stress during flexion, potentially leading to increased risk of adjacent level fracture.
If the increasing kyphosis increases the risk of additional fractures, one might assume that reducing or preventing the worsening kyphosis may be beneficial. To determine the effect of thoracic vertebral compression fractures on kyphosis or on geometric alignment and shift of load path alignment, Gaitanis and colleagues performed a biomechanical study using human thoracic specimens. These specimens were also used to evaluate geometric and load path alignment after fracture reduction by balloon bone tamp and by spinal extension alone. Six fresh thoracic specimens of 3 adjacent vertebrae with intact adjacent soft tissues (a functional spine unit) were used as the model. In this study, the compressive load shifted anteriorly by 7.8 mm after a single fracture of the middle of the 3 vertebral elements or by 22% of the anteroposterior dimension of the endplate of the fractured vertebra. The supraadjacent vertebra demonstrated a 23% shift (7.9 mm), and the subjacent vertebra demonstrated an 18% shift (6.4 mm). After treatment of the fractured vertebra using a bone tamp, segmental kyphosis was corrected by 8.7° (66%) and vertebral kyphosis was corrected by 11° (85%). Although the load path was returned more posteriorly, it remained anterior to the prefracture load path; 56% of the postfracture change was recovered.
In the same study, cementation with only hyperextension corrected anterior vertebral deformity to near prefracture values; however, segmental kyphosis and middle height were not corrected. The investigators concluded that bone tamp inflation significantly reduced deformity of the vertebral body height and kyphosis and resulted in return of the load path to near prefracture alignment. Hyperextension alone improved vertebral body deformity and load path alignment, without restoring middle vertebral height and kyphotic deformity.
Correction of kyphosis of the fractured vertebral body does not necessarily correlate with overall kyphosis correction. Pradhan and colleagues performed a retrospective study of 65 patients who had undergone 1 to 3 level kyphoplasty, analyzing the pre- and postoperative radiographs. Height gain was maximal at the midvertebral body (39%, 6.4 mm) and less in the anterior vertebral body (15%, 3.1 mm). For single level kyphoplasty, vertebral kyphosis was reduced by 7.3°. However, segmental kyphotic deformity was reduced by only 2.4° at 1 level, 1.4° at 2 levels, and 1° at 3 levels above and below the treated vertebra. Most kyphosis correction obtained in this study was limited to the treated vertebral body; a phenomenon which the investigators suggested may be attributable to the absorptive properties of the intervertebral disk.
Risk of adjacent fracture
Adjacent level fractures certainly occur after vertebral augmentation; however, because the natural history of osteoporosis also demonstrates a high fracture rate in the same load-bearing zone, the cause of adjacent level fracture may not be easily ascertained.
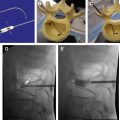
It is generally accepted that 20% of patients who suffer an initial vertebral compression fracture and are not treated with systemic osteoporosis therapy experience an additional vertebral compression fracture within 1 year. It is difficult to discriminate between the effect of vertebral augmentation and the powerful influence of natural history. The presence of a single osteoporotic vertebral compression fracture increases the risk of a new fracture by at least 5-fold. The presence of 2 or more osteoporotic vertebral compression fractures at baseline increases the risk of a new fracture by 12 times. According to the literature, the risk of new adjacent fractures with vertebroplasty ranges from 0% to 16%. For kyphoplasty, the risk ranges from 45% to 75% ( Fig. 1 ).
Studies on percutaneous vertebral augmentation to date have not stratified patients based on the extent and severity of osteoporosis. Many patients who present for percutaneous vertebral fracture reduction are not being managed for osteoporosis. Existing studies on percutaneous vertebral augmentation have not included the effect of posttreatment management, including bisphosphonates and physical therapy. In the setting of osteoporosis, the incidence of subsequent vertebral compression fracture may decrease after the initiation of bisphosphonate therapy.
In a study with 1-year follow-up, 24% of the patients (16 out of 66) treated with percutaneous vertebroplasty developed new compression fractures (a total of 26 new fractures). Half of these new fractures were adjacent to the treated vertebral bodies; however, the presence of more than 2 preexisting compression fractures was found to be the only independent risk factor for developing a new compression fracture.
In a prospective study of 25 patients with 34 fractures who were treated with percutaneous vertebroplasty and followed for 48 months, 13 patients (52%) developed at least 1 new vertebral fracture during follow-up. The odds ratio for a new compression fracture in the vicinity of a treated vertebra was 2.27 compared with 1.44 for a new fracture in the vicinity of an untreated vertebra and was not statistically significant.
To further complicate the analysis, patients with primary and secondary osteoporosis may have a different incidence of fracture after kyphoplasty than patients with primary osteoporosis. In a retrospective review, 22.6% of patients (26 of 115) demonstrated new compression fractures after kyphoplasty. Thirty-five percent of these patients had primary osteoporosis and 17% had steroid induced osteoporosis. The incidence of postkyphoplasty fracture was 11.25% (9 out of 80) in patients with primary osteoporosis. In contrast, the incidence of postkyphoplasty fracture in patients with secondary osteoporosis was 48.6% (17 out of 35), a statistically significant increase.
Mudano and colleagues performed a retrospective study to compare the risk of subsequent fracture in patients with an initially treated versus untreated vertebral compression fracture over 18 months. New compression fractures were defined as occurring 90 to 360 days after the index event and at a different level than the baseline fracture. Of the 48 treated patients, 51% had undergone vertebroplasty and 49% had undergone kyphoplasty. Information on bisphosphonate therapy was lacking. Risk of a subsequent fracture at a new level within 90 days was 5 times greater in treated patients than in the untreated comparison group. Incidence of subsequent vertebral compression fractures doubled at 360 days, by 18.8% in the treated group and 9.7% in the comparison group. At 360 days after the index fracture, 19% of treated patients had subsequent compression fractures compared with only 7% in the comparison group. Median time to new fracture was 2 months in the treatment group versus 3 months in the control group. All new fractures occurred within 3 levels of the index fracture. Fracture incidence after vertebroplasty and kyphoplasty were not compared.
Multiple studies have reported the incidence of subsequent fractures after vertebroplasty or kyphoplasty; extremely variable results may reflect the complexity of factors involved. In a retrospective review of 177 patients treated with percutaneous vertebroplasty over 2 years, 12.4% (22 patients) were found to have a total of 36 new compression fractures. Of these, 67% of the fractures occurred adjacent to previously treated vertebrae, and 33% (12) occurred in nonadjacent vertebrae. Of the 36 new compression fractures, 67% occurred within 30 days of initial treatment. It is important to note that this study involved a bipedicular approach in 60 (86%) of the 70 vertebroplasties performed, using an average of 9.14 mL of PMMA (ranging from 5–14.5 mL). In another study, 12.5% (3 out of 23) of treated patients experienced additional fractures at untreated levels within 15 to 18 months of vertebroplasty. In a retrospective review of patients treated with kyphoplasty, 26% (10 out of 38 patients) sustained new compression fractures over an average of 8-month follow-up.
Increased risk of adjacent level fracture in kyphoplasty as compared with vertebroplasty has been reported by Frankel, whose study included 36 patients with 46 compression fractures. Kyphoplasty was performed in 17 patients with 20 compression fractures, using an average of 4.65 mL cement. Ninety-five percent of the procedures were bilateral and 15% demonstrated cement extravasation. Vertebroplasty was performed in 19 patients with a total of 26 compression fractures, using an average of 3.78 mL cement. Nineteen percent of the procedures were bilateral with 7.7% cement extravasation. Pain improved in 90% of both groups. Within 90 days, 5 new adjacent fractures were seen in patients treated with kyphoplasty, whereas no new adjacent fractures were seen in those treated with vertebroplasty. The investigators concluded that vertebroplasty offers comparable pain relief with less cement and a unilateral approach and with significantly less risk of adjacent fracture.
Risk of adjacent fracture
Adjacent level fractures certainly occur after vertebral augmentation; however, because the natural history of osteoporosis also demonstrates a high fracture rate in the same load-bearing zone, the cause of adjacent level fracture may not be easily ascertained.
It is generally accepted that 20% of patients who suffer an initial vertebral compression fracture and are not treated with systemic osteoporosis therapy experience an additional vertebral compression fracture within 1 year. It is difficult to discriminate between the effect of vertebral augmentation and the powerful influence of natural history. The presence of a single osteoporotic vertebral compression fracture increases the risk of a new fracture by at least 5-fold. The presence of 2 or more osteoporotic vertebral compression fractures at baseline increases the risk of a new fracture by 12 times. According to the literature, the risk of new adjacent fractures with vertebroplasty ranges from 0% to 16%. For kyphoplasty, the risk ranges from 45% to 75% ( Fig. 1 ).
Studies on percutaneous vertebral augmentation to date have not stratified patients based on the extent and severity of osteoporosis. Many patients who present for percutaneous vertebral fracture reduction are not being managed for osteoporosis. Existing studies on percutaneous vertebral augmentation have not included the effect of posttreatment management, including bisphosphonates and physical therapy. In the setting of osteoporosis, the incidence of subsequent vertebral compression fracture may decrease after the initiation of bisphosphonate therapy.
In a study with 1-year follow-up, 24% of the patients (16 out of 66) treated with percutaneous vertebroplasty developed new compression fractures (a total of 26 new fractures). Half of these new fractures were adjacent to the treated vertebral bodies; however, the presence of more than 2 preexisting compression fractures was found to be the only independent risk factor for developing a new compression fracture.
In a prospective study of 25 patients with 34 fractures who were treated with percutaneous vertebroplasty and followed for 48 months, 13 patients (52%) developed at least 1 new vertebral fracture during follow-up. The odds ratio for a new compression fracture in the vicinity of a treated vertebra was 2.27 compared with 1.44 for a new fracture in the vicinity of an untreated vertebra and was not statistically significant.
To further complicate the analysis, patients with primary and secondary osteoporosis may have a different incidence of fracture after kyphoplasty than patients with primary osteoporosis. In a retrospective review, 22.6% of patients (26 of 115) demonstrated new compression fractures after kyphoplasty. Thirty-five percent of these patients had primary osteoporosis and 17% had steroid induced osteoporosis. The incidence of postkyphoplasty fracture was 11.25% (9 out of 80) in patients with primary osteoporosis. In contrast, the incidence of postkyphoplasty fracture in patients with secondary osteoporosis was 48.6% (17 out of 35), a statistically significant increase.
Mudano and colleagues performed a retrospective study to compare the risk of subsequent fracture in patients with an initially treated versus untreated vertebral compression fracture over 18 months. New compression fractures were defined as occurring 90 to 360 days after the index event and at a different level than the baseline fracture. Of the 48 treated patients, 51% had undergone vertebroplasty and 49% had undergone kyphoplasty. Information on bisphosphonate therapy was lacking. Risk of a subsequent fracture at a new level within 90 days was 5 times greater in treated patients than in the untreated comparison group. Incidence of subsequent vertebral compression fractures doubled at 360 days, by 18.8% in the treated group and 9.7% in the comparison group. At 360 days after the index fracture, 19% of treated patients had subsequent compression fractures compared with only 7% in the comparison group. Median time to new fracture was 2 months in the treatment group versus 3 months in the control group. All new fractures occurred within 3 levels of the index fracture. Fracture incidence after vertebroplasty and kyphoplasty were not compared.
Multiple studies have reported the incidence of subsequent fractures after vertebroplasty or kyphoplasty; extremely variable results may reflect the complexity of factors involved. In a retrospective review of 177 patients treated with percutaneous vertebroplasty over 2 years, 12.4% (22 patients) were found to have a total of 36 new compression fractures. Of these, 67% of the fractures occurred adjacent to previously treated vertebrae, and 33% (12) occurred in nonadjacent vertebrae. Of the 36 new compression fractures, 67% occurred within 30 days of initial treatment. It is important to note that this study involved a bipedicular approach in 60 (86%) of the 70 vertebroplasties performed, using an average of 9.14 mL of PMMA (ranging from 5–14.5 mL). In another study, 12.5% (3 out of 23) of treated patients experienced additional fractures at untreated levels within 15 to 18 months of vertebroplasty. In a retrospective review of patients treated with kyphoplasty, 26% (10 out of 38 patients) sustained new compression fractures over an average of 8-month follow-up.
Increased risk of adjacent level fracture in kyphoplasty as compared with vertebroplasty has been reported by Frankel, whose study included 36 patients with 46 compression fractures. Kyphoplasty was performed in 17 patients with 20 compression fractures, using an average of 4.65 mL cement. Ninety-five percent of the procedures were bilateral and 15% demonstrated cement extravasation. Vertebroplasty was performed in 19 patients with a total of 26 compression fractures, using an average of 3.78 mL cement. Nineteen percent of the procedures were bilateral with 7.7% cement extravasation. Pain improved in 90% of both groups. Within 90 days, 5 new adjacent fractures were seen in patients treated with kyphoplasty, whereas no new adjacent fractures were seen in those treated with vertebroplasty. The investigators concluded that vertebroplasty offers comparable pain relief with less cement and a unilateral approach and with significantly less risk of adjacent fracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree