Percutaneous lumbar discectomy is a proven alternative to the more invasive open discectomy used to treat patients who experience discogenic pain. Estimated to cost the United States health care system more than $20 billion a year, discogenic leg pain represents the primary cause of health care expenditure. Taken together, back pain and discogenic leg pain result in more days lost than any other combined illnesses and injuries. Annular breakdown and tears are common discogenic sources that produce pain, and are usually treated with microdiscectomy by orthopedic surgeons and neurosurgeons. Open discectomy has been considered to be the gold standard for relieving pressure on nerve roots. By decompressing the nerve root from the disc, neurologic function is usually restored and pain is relieved. Recurrent disc herniations may and typically do occur because of the annular violation that results from the surgical procedure.
Estimated to cost the United States health care system more than $20 billion a year, discogenic leg pain represents the primary cause of health care expenditure. Taken together, back pain and discogenic leg pain result in more days lost than any other combined illnesses and injuries.
Annular breakdown and tears are common discogenic sources that produce pain, and are usually treated with microdiscectomy by orthopedic surgeons and neurosurgeons. Open discectomy has been considered to be the gold standard for relieving pressure on nerve roots. By decompressing the nerve root from the disc, neurologic function is usually restored and pain is relieved. Recurrent disc herniations may and typically do occur because of the annular violation that results from the surgical procedure.
Many percutaneous procedures that specifically focus on disc herniation have been developed over the last several decades. These procedures have included chemonucleolysis, automated/manual percutaneous nucleotomy, laser treatments, intradiscal thermal annuloplasty and, more recently, nucleoplasty and Dekompressor. All these procedures are designed to reduce intradiscal pressure, so that the protruded disc area can retract back into place, given that there is enough elastogenicity to allow recovery.
Anatomy
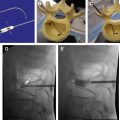
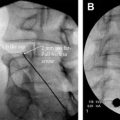
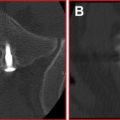
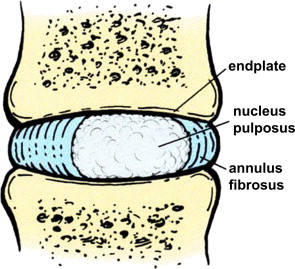
A central cartilaginous fibrous ring having sensitive nerve endings surrounding the outer rim anatomically comprises the intervertebral disc. The nucleus is bordered superiorly and inferiorly by dense cartilage and bony endplates from the respective vertebral surfaces ( Fig. 1 ).
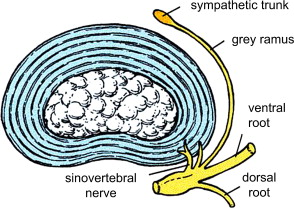
Composed of an inner and outer layer, the annulus is loosely attached to the anterior longitudinal ligament and is strongly attached to the posterior longitudinal ligament. This structure explains why axial back pain results when a central-disc protrusion occurs. The pain occurs when the fibers pull away from their attachments because of the ligamentous displacement from the annulus and the vertebral body. The nucleus, a notochordal remnant that is relatively avascular in the adult and is not significantly innervated, acts as a cushion. The annulus is a highly innervated structure in which the sinu-vertebral nerve wraps around the posterior aspect. Substance P and unmyelinated C fibers have been shown to be present in the annulus ( Fig. 2 ).
The intervertebral disc functions to provide a surface area to distribute stress absorption and motion restriction. The annulus serves to contain the nuclear material and to restrict longitudinal and rotational motion between spinal segments. Fibers in the annulus are arranged in variable directions in each fibrous layer to provide support in multiple directions. Approximately 20 of these are arranged anteriorly and 12 to 15 are arranged posteriorly.
Intervertebral discs in spinal pain
It is thought that discogenic pain originates from the sinu-vertebral nerves that innervate the outer annulus of the discs. Discogenic pain is provoked by any factor that produces an inflammatory response from the chemical mediators in the disc. Phospholipase A and prostaglandins are known irritants to the outer nerve supply and thereby produce pain and inflammation. Typically seen when axial loading results in pain during standing and extending the spine, discogenic pain is described as stabbing, knifelike, or burning in nature.
There are many theories about the exact pathophysiology of the pain mechanism, but most revolve around pathologic tears of the posterior annulus of the disc and mechanical or chemical stimulation of nociceptive receptors, located in and around the posterior annulus fibrosus, relayed through the sinu-vertebral nerve.
Present therapy, which has remained unchanged for many years, includes rest, relaxation, anti-inflammatory agents, and application of ice to the affected areas. Limited exercise, stretching, and aquatic body posturing are then introduced. If the pain does not improve with conservative measures, interventional therapies such as trigger injections, nerve conduction blockade, and central nervous system blocks (ie, epidural steroids, radiofrequency ablation, and sympathetic blockade) may have a place in the course of treatment.
If surgical intervention is needed to restore normal nerve function, it should only be considered when a neurologic deficit causes loss of reflexes, sensory deficits, or weakness. This surgical intervention may be a minimally invasive microdiscectomy, laminectomy, or foraminotomy or an extensive fusion. Other considerations include morbidity, cost, loss of work time, rehabilitation, the possibility of developing chronic pain, and medication dependency.
Intervertebral discs in spinal pain
It is thought that discogenic pain originates from the sinu-vertebral nerves that innervate the outer annulus of the discs. Discogenic pain is provoked by any factor that produces an inflammatory response from the chemical mediators in the disc. Phospholipase A and prostaglandins are known irritants to the outer nerve supply and thereby produce pain and inflammation. Typically seen when axial loading results in pain during standing and extending the spine, discogenic pain is described as stabbing, knifelike, or burning in nature.
There are many theories about the exact pathophysiology of the pain mechanism, but most revolve around pathologic tears of the posterior annulus of the disc and mechanical or chemical stimulation of nociceptive receptors, located in and around the posterior annulus fibrosus, relayed through the sinu-vertebral nerve.
Present therapy, which has remained unchanged for many years, includes rest, relaxation, anti-inflammatory agents, and application of ice to the affected areas. Limited exercise, stretching, and aquatic body posturing are then introduced. If the pain does not improve with conservative measures, interventional therapies such as trigger injections, nerve conduction blockade, and central nervous system blocks (ie, epidural steroids, radiofrequency ablation, and sympathetic blockade) may have a place in the course of treatment.
If surgical intervention is needed to restore normal nerve function, it should only be considered when a neurologic deficit causes loss of reflexes, sensory deficits, or weakness. This surgical intervention may be a minimally invasive microdiscectomy, laminectomy, or foraminotomy or an extensive fusion. Other considerations include morbidity, cost, loss of work time, rehabilitation, the possibility of developing chronic pain, and medication dependency.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree