Asif Saifuddin
Bone Tumours (1)
Benign Tumours and Tumour-Like Lesions of Bone
General Characteristics of Bone Tumours
Bone tumours may be benign or malignant, and are currently classified according to the World Health Organisation Classification of 2002.1 The pre-biopsy diagnosis of a bone tumour depends upon several features, including patient age, lesion location and finally the radiological characteristics. The latter allows an assessment of rate of growth (generally indicative of benignity or malignancy) and underlying histological subtype, based predominantly upon patterns of matrix mineralisation (Table 47-1).
TABLE 47-1
Classification of Primary Benign Bone Tumours
| Cartilage tumours | |
| Osteogenic tumours | |
| Fibrogenic tumours | |
| Fibrohistiocytic tumours | |
| Giant cell tumour | |
| Vascular tumours | |
| Smooth muscle tumours | |
| Lipogenic tumours | |
| Neural tumours | |
| Miscellaneous lesions |
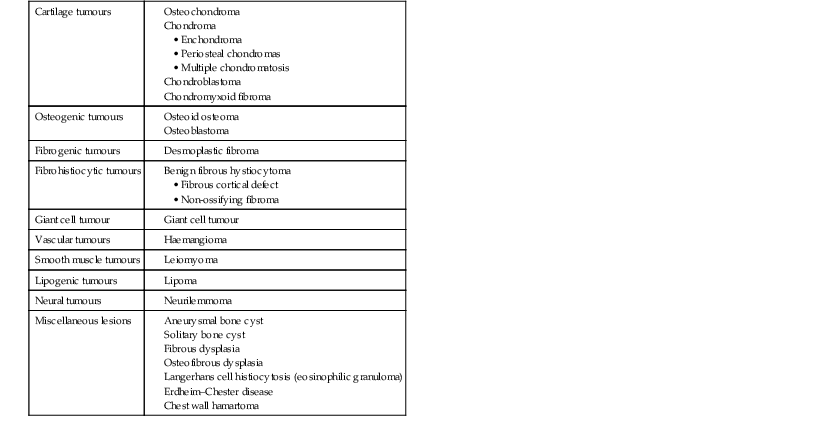
Modified from WHO 2002 Classification.1
Age at Presentation
Patient age is of huge importance in suggesting a differential diagnosis of a focal bone lesion. Primary bone tumours are rare below the age of 5 years and over the age of 40 years, with the exception of myeloma and chondrosarcoma. Metastases are the commonest lesions over the age of 40 years.
Radiological Assessment of Bone Tumours1
Location
The location of the lesion within the skeleton (appendicular, axial) and within the individual bone (epiphysis, metaphysis, diaphysis; intramedullary, intracortical, surface) must be considered in detail when discussing individual tumours, since it has a considerable influence on differential diagnosis.
Rate of Growth
When considering rate of growth, the most important feature is the lesion margin. In benign and low-grade malignant neoplasms, this margin is sharp (geographical; Type 1). Type 1A has a rim of sclerosis between the lesion and the host bone (Fig. 47-1A), Type 1B is a very well defined lytic lesion but with no marginal sclerosis (Fig. 47-1B), while Type 1C has a slightly less sharp, non-sclerotic margin (Fig. 47-1C). Type 2 is moth-eaten destruction, which represents the next most aggressive pattern and is characterised by multiple lucent areas measuring 2–5 mm in diameter separated by bone which has yet to be destroyed (Fig. 47-2). Type 3 is permeative destruction, which is the most aggressive pattern and is composed of multiple coalescing small ill-defined lesions 1 mm or less in diameter with a zone of transition of several centimetres (Fig. 47-3). Radiographs inevitably underestimate the extent of medullary involvement, which is more clearly shown on magnetic resonance imaging (MRI).
Regions with apparently intact cortex may show extracortical tumour masses. This phenomenon often leads, in highly malignant tumours such as Ewing’s sarcoma, to ‘cortical saucerisation’ as the tumour, temporarily restrained by the periosteum, erodes back through the cortical bone.
Benign or low-grade malignant neoplasms tend to remain within the medullary cavity until late in their development. Typically, the cortex is not destroyed, but slow erosion of its endosteal surface (endosteal scalloping) together with periosteal new bone formation results in expansion of bone (Fig. 47-1A). Conversely, high-grade malignant tumours commonly extend through the cortex by the time of presentation, resulting in cortical destruction and an adjacent extraosseous mass (Fig. 47-3).
Periosteal Reaction2
Periosteal reaction is of various types with none being pathognomonic of any particular tumour: rather, the type helps to indicate the aggressiveness of the lesion. A thick, well-formed (solid) periosteal reaction (Fig. 47-4A) indicates a slow rate of growth but not necessarily a benign tumour, since it may be seen with chondrosarcoma. Laminated periosteal reaction (Fig. 47-4B) indicates subperiosteal extension of tumour, infection or haematoma. Lesions demonstrating periodic growth may show a multi-laminated pattern (Fig. 47-4C). A Codman’s triangle indicates the limit of subperiosteal tumour in a longitudinal direction (Fig. 47-4B). Vertical (sunburst spiculation or ‘hair-on-end’) types of periosteal reaction are seen with the most aggressive tumours such as osteosarcoma (Fig. 47-4D) and Ewing’s sarcoma. However, the most rapidly growing lesions may not be associated with any radiographically visible periosteal response, since mineralisation of the deep layer of periosteum can take 2 weeks.
Matrix Mineralisation
The matrix of a tumour represents the extracellular material produced by the tumour cells within which the cells lie. Certain tumours produce characteristic radiographically visible matrix mineralisation, which allows the histological cell type to be predicted. Chondral calcifications are typically linear, curvilinear, ring-like, punctate or nodular (Fig. 47-5A). Osseous mineralisation is cloud-like and poorly defined (Fig. 47-5B), whereas diffuse matrix mineralisation in benign fibrous tumours produces the characteristic ‘ground-glass’ appearance (Fig. 47-5C), seen most commonly in fibrous dysplasia. Some neoplasms, such as adenocarcinoma metastases, can provoke reactive mineralisation, whereas calcifications within an intraosseous lipoma are due to associated fat necrosis. Also, some bone sarcomas may develop on underlying calcified bone infarcts.
CT and MRI in Diagnosis and Staging
CT is excellent for demonstrating the presence of radiographically occult matrix mineralisation and the persistence of a thin cortical shell, indicating that the tumour still lies deep to the periosteum. CT also plays a major role in the investigation of cortical thickening, allowing the demonstration of the cause, such as the nidus of an osteoid osteoma or a stress fracture.
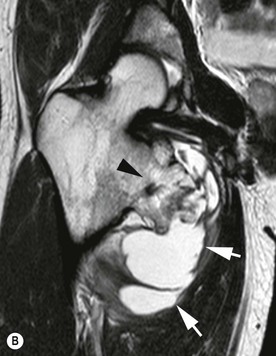
The major role of MRI is in local staging, particularly for high-grade malignant tumours such as osteosarcoma, where the intraosseous extent, identification of ‘skip’ lesions and relationship to the neurovascular bundle and adjacent joint can all be assessed with great accuracy.3 Such information is vital for planning surgical management, be it limb salvage or amputation. Dynamic contrast-enhanced MRI has been advocated for determining chemotherapeutic response, but its role in routine patient management is unclear.
In the presence of a purely lytic lesion, several MRI features may help in further lesion characterisation.4 The presence of profound low signal intensity (SI) on T2*-weighted gradient-echo images indicates chronic haemorrhage and may be seen with giant cell tumour. MRI is very sensitive to the presence of fluid–fluid levels (FFLs) and the degree of FFL change is related to histological diagnosis.5 Lesions that are completely filled with FFLs are almost always aneurysmal bone cysts (ABCs). MRI can also demonstrate a fatty matrix, as seen with haemangioma and intraosseous lipoma. The vascular nature of renal metastases has been demonstrated by the presence of the ‘flow-void’ sign.6 MRI is very sensitive to reactive medullary and soft-tissue oedema, which characterises certain lesions such as osteoid osteoma, osteoblastoma, chondroblastoma and Brodie’s abscess.7
Bone scintigraphy plays little role in the diagnostic work-up of a suspected primary bone tumour, with the possible exception of osteoid osteoma or osteoblastoma, particularly in the spine. However, scintigraphy is still useful for the identification of skeletal metastases, although this role has recently been challenged by whole-body MRI.8
The position of techniques such as MR spectroscopy, positron emission tomography (PET) and computed tomography PET (CT-PET) in the management of suspected bone tumours is as yet unclear, while whole-body diffusion-weighted MRI (WBDWI) is highly sensitive for the identification of skeletal metastases.9 Finally, the use of ultrasound10 and CT11 for image-guided needle biopsy is well established, while MR-guided biopsy has also been developed for targeting subtle marrow lesions.12
Benign Bone Tumours
Benign bone tumours are currently classified according to the 2002 World Health Organisation system based on their cell of origin1 (Table 47-1).
Cartilage Tumours
Osteochondroma13
Recent genetic studies indicate that osteochondroma is a true neoplasm, which may also arise following radiotherapy and accounts for 20–50% of benign bone tumours. Osteochondromas present from 2 to 60 years, but the highest incidence is in the second decade, with a male-to-female ratio of 1.4–3.6 : 1.
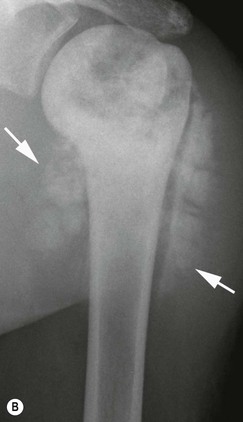
Long bones are commonly affected, especially around the knee (~40%), the commonest locations being the distal femur, proximal humerus, proximal tibia and proximal femur. The commonest flat bones affected are the ilium and scapula. Lesions may be classified as either pedunculated, when they have a thin stalk that typically points away from the adjacent joint, or sessile when they arise from a broad base. They are typically metaphyseal in location.
Diaphyseal aclasis (hereditary multiple exostoses, HME) constitutes an uncommon autosomal dominant disorder in which the exostoses may be larger than the solitary variety and may lead to shortening or deformity of the affected limbs. The metaphyses in this condition are also typically widened and dysplastic (Fig. 47-6).
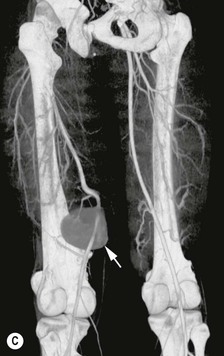
Osteochondromas present with mechanical problems such as an enlarging mass, pressure on adjoining structures (muscles, nerves, vessels), or rarely with fracture of the bony stem. Mechanical irritation of overlying soft tissues may result in adventitial bursa formation, which can mimic sarcomatous degeneration. MRI is highly accurate in the assessment of symptomatic osteochondromas.14 The incidence of chondrosarcomatous change in the cartilage cap is very small in a solitary osteochondroma (probably <1%), while malignant degeneration in diaphyseal aclasis is approximated at 3–5%.
Radiological Features
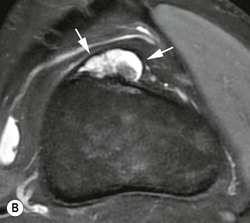
The lesion appears as an outgrowth from the normal cortex, with which it is continuous. Pedunculated lesions have a long slim neck (Fig. 47-7A), whereas sessile lesions have a broad base from the bone of origin (Fig. 47-7B). Continuity between the medullary cavity of the lesion and that of the underlying bone is essential for the diagnosis and is best demonstrated on either CT or MRI (Fig. 47-8A). The cartilage cap is optimally demonstrated on axial proton density-weighted (PDW) or T2W fast spin-echo (FSE) MRI, when the hyperintense cartilage contrasts well against the adjacent iso-/hypointense muscle (Fig. 47-8A) and it should not exceed 2-cm thickness in adults. The cartilage cap can also be visualised and measured on ultrasound where it appears hypoechoic in contrast to the brightly reflective bone surfaces. Complications associated with OC include bursa formation (Fig. 47-8B), neurovascular compromise and, rarely, pseudoaneurysm (Fig. 47-8C).
(En)Chondroma13
(En)Chondroma is an intramedullary neoplasm comprising lobules of benign hyaline cartilage and is the second commonest benign chondral lesion after osteochondroma, accounting for approximately 8% of all primary bone tumours and tumour-like lesion in a large biopsy series. However, the true prevalence of enchondromas is unknown since the majority are asymptomatic. Incidental enchondromas have been identified in approximately 3% of routine knee MRI studies. Enchondromas affect the tubular bones of the hands and feet in 40–65% of cases and present either when they become symptomatic due to increasing size, as pathological fracture (in 60% of cases) or as incidental findings. The majority arise in the proximal phalanges (40–50%), followed by the metacarpals (15–30%) and middle phalanges (20–30%). The small bones of the feet are involved in 7% of cases. Approximately 25% are found in the femur, tibia and humerus, while other sites are very rare. The age range is 10–80 years, with most presenting in the second to fourth decades. There is equal prevalence among both genders.
Radiological Features
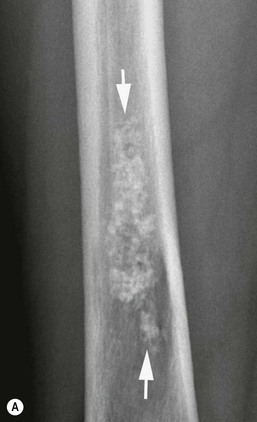
Most enchondromas arise centrally in the phalanges and metacarpals. Lesions are typically metaphyseal or diaphyseal, with epiphyseal location accounting for approximately 8%. Enchondromas are often eccentric and 75% are solitary. They are typically well-circumscribed, lobular or oval lytic lesions, which may expand the cortex (Fig. 47-9A). Size at presentation ranges from 10 to 50 mm. Chondral-type mineralisation may be identified within the matrix.
The term ‘enchondroma protuberans’ has been used to describe an eccentrically placed enchondroma with an associated extraosseous component which is usually covered by a thin shell of intact cortical bone (Fig. 47-9B). Most cases arise in the fingers or toes and they may be difficult to distinguish from periosteal chondroma, although this may not be clinically relevant since both lesions have the same management.
The differentiation between a relatively large enchondroma and a grade 1 chondrosarcoma can be difficult. Lesion size above 5–6 cm and deep endosteal scalloping are suggestive of chondrosarcoma,15 but prominent scalloping can also be seen with an eccentrically placed chondroma, which has been termed an ‘endosteal chondroma’. However, this differentiation may not be of clinical relevance, since both can be treated in the same way, with either careful clinical and imaging follow-up, or curettage with cementation. Low-grade chondral tumours have characteristic MRI features, showing a lobular margin with intermediate T1-weighted signal intensity (T1W SI) (Fig. 47-10A) and T2-weighted/short tau inversion recovery (T2W/STIR) hyperintensity without surrounding reactive oedema (Fig. 47-10B). Matrix mineralisation manifests as punctate areas of signal void. A hypointense rim and septations may also be seen, the latter showing enhancement following IV gadolinium contrast medium.13
Less Common Varieties of Chondroma
Periosteal Chondroma.16
These are rare lesions affecting children and young adults and are located in the metaphyses of tubular bones, most commonly the proximal humerus followed by the femur and tibia. They are also seen in the small bones of the hands and feet, in which case some extension into the underlying medullary cavity is commonly seen. Radiologically, each appears as a well-defined area of cortical erosion typically measuring 1–3 cm with mature periosteal reaction and sometimes a thin external shell of bone. Cartilaginous matrix mineralisation is observed in half the cases (Fig. 47-11A). MRI shows the features of a chondral lesion with a lobular hyperintense mass on T2-weighted images adjacent to the cortex (Fig. 47-11B). The differential diagnosis includes periosteal chondrosarcoma and periosteal osteosarcoma. Malignant transformation has not been reported.
Enchondromatosis (Ollier’s Disease).
Rare disease. Prevalence is estimated at around 1 in 100,000. In addition to multiple enchondromas, flame-like rests of cartilage in the metaphyses impede bone growth and may result in bowing, angulation and bone enlargement (Fig. 47-12). Malignant change is reported in 5–30% of cases.
Enchondromatosis with Haemangiomas (Maffucci’s Syndrome).
This rare disorder combines multiple enchondromas and soft-tissue haemangiomas (occasionally lymphangiomas). The condition is unilateral in 50% of cases. Radiographically, the presence of phleboliths differentiates the disorder from Ollier’s disease, while the haemangiomas are well demonstrated by MRI. The true incidence of chondrosarcomatous change is uncertain because of the rarity of the disease, but is reported in approximately 20% of cases, usually in patients over the age of 40 years.
Chondroblastoma13,17
Chondroblastoma accounts for approximately 1% of all bone neoplasms, with 80–90% occurring between the ages of 5 and 25 years (mean age ~20 years). However, lesions of the flat bones such as the talus commonly present later. The male : female ratio is almost 2.7 : 1. Chondroblastoma has rarely been associated with metastases (especially to the lung) and a rare variant termed ‘aggressive’ (atypical) chondroblastoma, associated with cortical destruction and soft-tissue extension, has also been described.
Chondroblastoma commonly presents as mono-arthropathy, since it is typically located in the epiphysis of a long bone, and may promote a synovial reaction. Fifty per cent arise around the knee, while the proximal femur and humeral head are also commonly affected (~20% each). Chondroblastoma is classically located eccentrically in the epiphysis (40%), but with partial closure of the growth plate it usually extends into the metaphysis (55%). The apophyses and sesamoid bones can also be involved, accounting for involvement of the greater trochanter of the femur and the greater tuberosity of the humerus. Approximately 2% are located purely within the metaphysis or diaphysis.18 In the feet, the calcaneus and talus are most commonly involved, while chondroblastoma is the commonest tumour of the patella.
Radiological Features
The lesion is usually spherical or lobular with a fine sclerotic margin, measuring 1–4 cm in size (Fig. 47-13A). Matrix mineralisation is demonstrated in ~30% radiographically. Linear metaphyseal periosteal reaction is present in almost 60% of long bone cases (Fig. 47-13A). MRI shows intermediate T1W SI (Fig. 47-13B) with variable SI on T2W images (Fig. 47-13C), including hypointensity and FFLs due to secondary aneurysmal bone cyst (ABC) change (~15% of cases). Associated marrow and soft-tissue oedema and reactive joint effusion are almost invariable (Fig. 47-13C
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree