TRAUMA: AVULSION AND STRETCH INJURIES
KEY FACTS
 Nerve root avulsions are generally caused by traction injuries of the extremities (in the lower cervical spine, they are related to traction of the arms; in the lower spine, they are related to lumbosacral spine or pelvic fractures).
Nerve root avulsions are generally caused by traction injuries of the extremities (in the lower cervical spine, they are related to traction of the arms; in the lower spine, they are related to lumbosacral spine or pelvic fractures).
 With complete avulsion, the nerve roots retract, leaving behind fluid-filled pseudomeningoceles.
With complete avulsion, the nerve roots retract, leaving behind fluid-filled pseudomeningoceles.
 Nerve avulsions at “root entry zones” may result in adjacent subarachnoid hematomas and edema/ hemorrhage in the spinal cord.
Nerve avulsions at “root entry zones” may result in adjacent subarachnoid hematomas and edema/ hemorrhage in the spinal cord.
 Penetration of meninges by bone fragments, bullets, or stab wounds may cause durai tears.
Penetration of meninges by bone fragments, bullets, or stab wounds may cause durai tears.
 Stretching of the plexus results in a “burning” injury, characterized by edema but which may later lead to degeneration and even posttrauma neuroma formation.
Stretching of the plexus results in a “burning” injury, characterized by edema but which may later lead to degeneration and even posttrauma neuroma formation.
 Compressive damage may be produced by posttrauma lesions such as clavicle fracture, hematoma, and pseudoaneurysm of subclavian artery.
Compressive damage may be produced by posttrauma lesions such as clavicle fracture, hematoma, and pseudoaneurysm of subclavian artery.

FIGURE 27-1. Coronal T2 shows a fluid-filled pseudomenlngocele (arrow) from avulsion of the eft C7 nerve root.
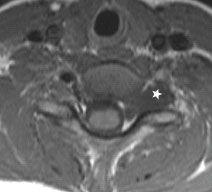
FIGURE 27-2. Axial T1, In the same patient, shows the pseudomenlngocele (star) In the region of the avulsed nerve root.
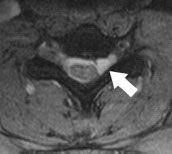
FIGURE 27-3. Axial T2, in a different patient, shows mostly internal pseudomeningocele (arrow) compressing the spinal cord.
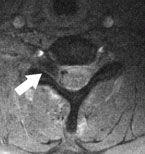
FIGURE 27-4. Axial T2, in a different patient, shows dark blood-filled pseudomeningocele (arrow) with inward displacement of thecal sac and subarachnoid blood.

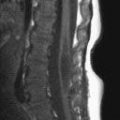
FIGURE 27-5. Parasagittal T2, in a different patient, shows two pseudomeningoceles (arrows).
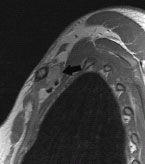
FIGURE 27-6. Parasagittal T1, in a different patient, shows bright retroclavicular hematoma (arrow) compressing the divisions of the plexus.
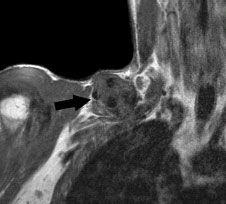
FIGURE 27-7. Coronal T1, in a different patient with poorly healed clavicle fracture, shows large callus (arrow) that resulted in a compressive plexopathy.

FIGURE 27-8. Coronal T2, in a different patient, shows thickening (arrows) and high signal due to stretching of the plexus.
SUGGESTED READING
Aralasmak A, Karaali K, Cevikol C, Uysal H, Senol U. MR imaging findings in brachial plexopathy with thoracic outlet syndrome. Am J Neuroradiol 2010;31:410–417.
KEY FACTS
 Schwannomas are the most common primary tumor of the brachial plexus; neurofibromas are the most common tumors in patients with NF-1 but may occasionally happen in patients without that disease.
Schwannomas are the most common primary tumor of the brachial plexus; neurofibromas are the most common tumors in patients with NF-1 but may occasionally happen in patients without that disease.
 Most schwannomas present with a sensory but often mixed sensory/motor plexopathy.
Most schwannomas present with a sensory but often mixed sensory/motor plexopathy.
 They may involve any part of the plexus but more commonly occur in the roots and trunks.
They may involve any part of the plexus but more commonly occur in the roots and trunks.
 Extension into and expansion of the corresponding neural foramen is typical.
Extension into and expansion of the corresponding neural foramen is typical.
 Enhancement pattern is nonspecific.
Enhancement pattern is nonspecific.
 Main differential diagnosis: neurofibroma, posttraumatic neuroma, metastasis, sarcoma, lymphoma.
Main differential diagnosis: neurofibroma, posttraumatic neuroma, metastasis, sarcoma, lymphoma.

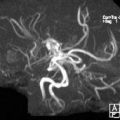
FIGURE 27-9. Coronal T2 shows a mass in the region of the right roots/trunks extending to a neural foramen (arrow).
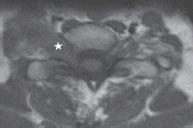
FIGURE 27-10. Axial noncontrast T1, in the same patient, shows the schwannoma (star) expanding the neural foramen.
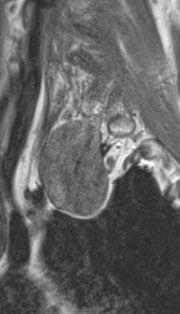
FIGURE 27-11. Parasagittal noncontrast T1, in a different patient, shows a large schwannoma.
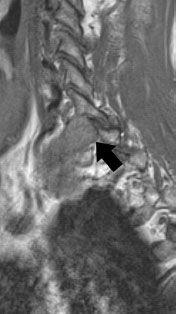
FIGURE 27-12. More medially, the mass is seen entering and expanding a neural foramen (arrow).
SUGGESTED READING
Bowen BC, Pattany PM, Saraf-Lavi E, Maravilla KR. The brachial plexus: normal anatomy, pathology, and MR imaging. Neuroimaging Clin North America 2004;14:59–85.
 BRACHIAL PLEXUS PLEXIFORM NEUROFIBROMAS
BRACHIAL PLEXUS PLEXIFORM NEUROFIBROMAS
KEY FACTS
 These tumors are mostly found in patients with NF-1 and are a hallmark of this disease.
These tumors are mostly found in patients with NF-1 and are a hallmark of this disease.
 Initially, mostly mild enlargement of the dorsal root ganglia is present.
Initially, mostly mild enlargement of the dorsal root ganglia is present.
 They attain large size, involve all of the plexus, and may be bilateral.
They attain large size, involve all of the plexus, and may be bilateral.
 Enhancement is variable, but a significant change in size and enhancement may indicate malignant degeneration.
Enhancement is variable, but a significant change in size and enhancement may indicate malignant degeneration.
 Main differential diagnosis: lymph nodes, lymphoma, metastasis, lymph nodes, hypertrophie polyneuropathy
Main differential diagnosis: lymph nodes, lymphoma, metastasis, lymph nodes, hypertrophie polyneuropathy
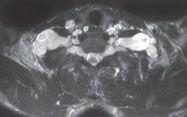
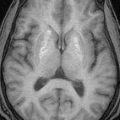
FIGURE 27-13. Axial T2 shows extensive, bilateral, bright plexiform neurofibromas in the brachial plexus. Note that masses arising in between the anterior and middle/posterior scalene muscles are nearly always primary tumors in the trunks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree