Presentation and Presenting Images
( ▶ Fig. 87.1, ▶ Fig. 87.2, ▶ Fig. 87.3, ▶ Fig. 87.4, ▶ Fig. 87.5, ▶ Fig. 87.6, ▶ Fig. 87.7, ▶ Fig. 87.8, ▶ Fig. 87.9, ▶ Fig. 87.10)
A 56-year-old female with a strong family history of breast cancer presents with left breast pain, marked with a BB. .
87.1.1 Breast Tissue Density
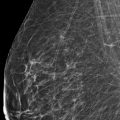
The breasts are heterogeneously dense, which may obscure small masses.
87.1.2 Imaging Findings
The conventional digital and synthetic mammograms do not demonstrate a significant finding correlating to the area of pain noted by the patient (marked with a BB in ▶ Fig. 87.1, ▶ Fig. 87.2, ▶ Fig. 87.3, and ▶ Fig. 87.4). The digital breast tomosynthesis (DBT) images ( ▶ Fig. 87.5 and ▶ Fig. 87.6) reveal a 1.3-cm irregular mass with obscured and spiculated margins at the 2 o’clock location, slightly anterior and medial to the site marked as painful. This lesion is not readily apparent on the full-field digital mammograms (FFDM) or the synthetic mammograms. The additional spot-compression mammograms ( ▶ Fig. 87.7, ▶ Fig. 87.8, ▶ Fig. 87.9, and ▶ Fig. 87.10) of this region also demonstrate the mass that was seen on DBT due to the associated architectural distortion. An ultrasound is recommended for further characterization.
87.2 Diagnostic Images
( ▶ Fig. 87.11, ▶ Fig. 87.12, ▶ Fig. 87.13, ▶ Fig. 87.14, ▶ Fig. 87.15)
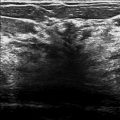
87.2.1 Imaging Findings
The ultrasound of the mammographic mass that is near the area of pain reveals a 9 × 9 × 13 mm irregular hypoechoic mass with indistinct margins at the 2 o’clock location, 3 cm from the nipple. Adjacent to this mass is a similar smaller, 7 × 5 × 8 mm irregular hypoechoic mass with indistinct margins and posterior shadowing located at the 3 o’clock location, 2 cm from the nipple ( ▶ Fig. 87.11, ▶ Fig. 87.12, and ▶ Fig. 87.13). In retrospect, the second mass is not seen on the conventional digital mammogram, synthetic mammogram, or DBT. Both masses were biopsied. The coil marker clip was placed in the 2 o’clock mass, and the ribbon clip, in the 3 o’clock mass ( ▶ Fig. 87.14 and ▶ Fig. 87.15).
87.3 BI-RADS Classification and Action
Category 4C: High suspicion for malignancy
87.4 Differential Diagnosis
Two cancers (invasive ductal carcinoma): The patient’s pain may have been a referred pain, but it did not directly relate to the masses. Her breast pain did bring her in for evaluation, and eventually for diagnosis of two adjacent cancers.
Fat necrosis: Fat necrosis can be symptomatic or asymptomatic. The patient has no history of trauma or surgical breast procedures. The imaging is too worrisome to dismiss the findings as fat necrosis. Biopsy of both lesions is warranted.
Radial scars: Radial scars are great mimickers of carcinoma. For this diagnosis to be concordant, the size of the imaging finding needs to match the size of the histopathologic finding. A smaller lesion would be discordant.
87.5 Essential Facts
This case demonstrates two adjacent cancers; one is seen mammographically and the other is occult. Both are seen by ultrasound.
Multifocal breast cancer is defined as multiple lesions (two or more) within 4 or 5 cm of each other.
Multifocal breast cancer typically occurs within the same quadrant.
Up to 27 to 34% of cancers are multifocal. Mammographically unifocal cancers were found to have additional foci at histopathologic aassessment.
It is more common for invasive lobular carcinoma (ILC) to be multifocal than for invasive ductal carcinoma. (IDC).
87.6 Management and Digital Breast Tomosynthesis Principles
Understanding the advantages and limitations of the breast imaging modalities allows one to optimize the use of these imaging modalities in detecting the majority of breast cancers. Ultrasound and magnetic resonance (MR) imaging can be useful adjunct tools in the detection of mammographically occult cancers.
Early studies suggest that DBT was better at detecting architectural distortion when compared to FFDM. DBT detected those architectural distortions seen on FFDM and also those not detected on FFDM.
Any new technology has a prevalence bias, that is, when first introduced, cancer detection rates are higher than observed in subsequent incident screening. This was observed when mammography and breast MRI were first introduced, and this may also now be happening with the introduction of DBT. Further studies are needed to determine the role that DBT will have in breast cancer detection.
87.7 Further Reading
[1] Berg WA, Gutierrez L, NessAiver MS, et al. Diagnostic accuracy of mammography, clinical examination, US, and MR imaging in preoperative assessment of breast cancer. Radiology. 2004; 233(3): 830‐849 PubMed
[2] Partyka L, Lourenco AP, Mainiero MB. Detection of mammographically occult architectural distortion on digital breast tomosynthesis screening: initial clinical experience. AJR Am J Roentgenol. 2014; 203(1): 216‐222 PubMed

Fig. 87.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree