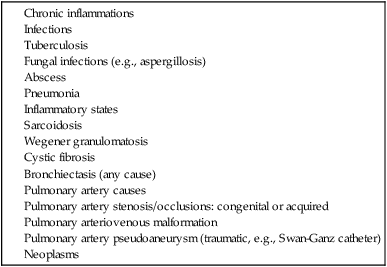
Hemoptysis has many causes (Table 84-1). Worldwide, disease states causing chronic lung inflammation arising from tuberculosis are the most common cause of hemoptysis. In the developed world, cystic fibrosis is the corresponding common culprit, leading to bronchiectasis requiring bronchial artery embolization. Regardless of the pathologic process, disease chronicity leads to hypertrophy in the respiratory mucosa of the bronchial circulation in response to occlusion of the pulmonary arterioles from hypoxia secondary to underlying pulmonary disease. These hypertrophied vessels are under systemic pressures, and rupture of these vessels leads to bleeding that “floods” the air spaces. It is the hypertrophy of these vessels that allows them to be amenable to transcatheter embolotherapy, resulting in a clinical benefit. TABLE 84-1 Obtaining and reviewing the history, physical examination, and tests, especially prior imaging studies, may help provide useful information before the procedure (Table 84-2). Try to ascertain the etiology and side of bleeding to help focus attention during the case to that side. Patients may describe a gurgling sensation on the side of the bleeding. If the pathologic process is limited to one side, imaging will show this and allow for targeted angiograms of that area. Contrast-enhanced chest computed tomography (CT) can offer a diagnosis in which chest radiography and bronchoscopy may be nondiagnostic.1,2 CT can help localize the site of bleeding in over half of cases of hemoptysis3 while also revealing hypertrophic vessels in the mediastinum along with their site of origin—key information to help with catheterization. CT can also suggest the presence of nonbronchial systemic arteries supplying the lung via thickened pleura,4 and this can help reduce instances of incomplete embolizations. When imaging is not helpful, bronchoscopy performed early in the course of the presentation can help localize the site of bleeding and/or pathologic process. TABLE 84-2 Preprocedural Issues to Address in Workup Table 84-3 lists some measures to consider in massive hemoptysis. A neurologic examination of the lower extremities is a must before any angiogram and/or embolization to help monitor for spinal cord complications. This should be repeated after the procedure to look for any changes and may also have to be repeated during the case if there is any concern for spinal cord compromise. If there is a history of recent Swan-Ganz catheter use, a pulmonary artery pseudoaneurysm should be considered and, if possible, computed tomographic angiography (CTA) of the lungs performed. In such a case, one can proceed straight to pulmonary angiography. A pulmonary arteriovenous malformation may also present as hemoptysis and can be seen on chest CT. Again, starting with a pulmonary angiogram is appropriate. The typical indication is massive hemoptysis, defined as 300 mL or more of expectorated blood within a 24-hour period.5–7 Hemoptysis reduces the available surface area for gas exchange. Depending on the severity of the underlying pathologic process, the available lung surface area will vary between patients, and some may experience respiratory distress with a volume of hemoptysis of less than 300 mL. Thus, a functional assessment is also useful in patient selection. Lesser amounts of bleeding (Table 84-4), especially if recurrent and debilitating, may also qualify patients to be candidates for this procedure. Patients with cystic fibrosis typically fall into this latter group, and the availability of lung transplantation has lowered the threshold to use bronchial artery embolization as a palliative measure to build a bridge to lung transplantation. TABLE 84-4 Indications for Bronchial Artery Embolization Table 84-5 lists recommended equipment for bronchial artery embolization. Adequate imaging equipment is a prerequisite. The initial catheter is one that allows for injection of an adequate volume of contrast agent. We prefer a 6F pigtail catheter positioned in the distal aortic arch to obtain a descending thoracic aortogram. The subsequent selection of guidewire and catheter equipment depends on the anatomy. In general, we prefer “pull down”–shaped catheters because they offer a secure and stable selection method of the desired vessel. Microcatheters used in a coaxial fashion through the previously positioned catheter allow for superselective catheter positioning within the vessel of interest to avoid nontarget embolization. The chosen embolic agent (our preference: 350- to 500-µm particles) can then be delivered via the catheter. Coils should be avoided because they preclude access into the same vessel at a later date when repeat embolization may be necessary. Liquid agents penetrate into the capillary level within the mucosa, creating necrosis. Furthermore, they may pass through any shunts and return to the heart for systemic distribution. Nonionic contrast agents should be used to minimize any chances of transverse myelitis occurring from injections of contrast media. TABLE 84-5 Equipment for Bronchial Artery Embolization
Bronchial Artery Embolization

Indications
Massive hemoptysis
300 mL or more in 24 hours
Moderate hemoptysis
Three or more episodes of 100 mL or more within 1 week
Mild hemoptysis
Chronic or slowly increasing episodes
Equipment
Catheters
Microcatheters
Nonionic contrast
Embolic agents ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access







