Bronchiectasis
Jud W. Gurney, MD, FACR
Key Facts
Terminology
Irreversible bronchial dilatation usually associated with inflammation of bronchial wall
Imaging Findings
↑ Bronchoarterial ratio (signet-ring sign)
B/A > 1 not specific, seen in elderly (> 65 years old) or those at high altitude (due to mild hypoxia that dilates bronchi and causes vasoconstriction)
Lack of bronchial tapering: Earliest and most sensitive sign of bronchiectasis
Acute pneumonia may result in pseudobronchiectasis (functional bronchiectasis)
Top Differential Diagnoses
Pneumonia
Chronic Bronchitis
Pathology
Integrity of bronchial wall dependent on normal immune system, normal structural integrity of airways (normal cartilage), and normal ciliary function
Infection (most common etiology)
Cystic fibrosis
Allergic bronchopulmonary aspergillosis
Chronic aspiration
Toxic fume inhalation, especially ammonia
Obstruction: Tumor, foreign body, or lymph node enlargement
Diagnostic Checklist
Central bronchial obstruction in patients with focal bronchiectasis
TERMINOLOGY
Definitions
Irreversible bronchial dilatation usually associated with inflammation of bronchial wall
IMAGING FINDINGS
General Features
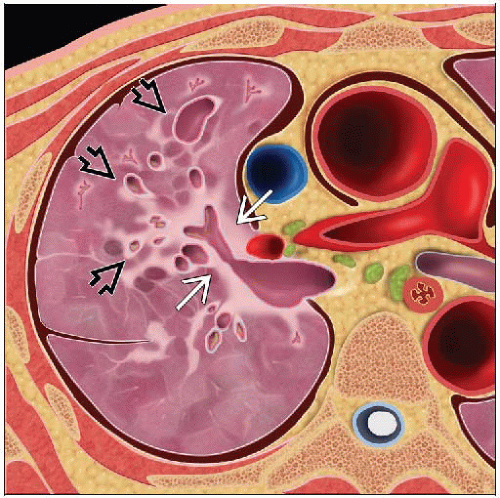
Best diagnostic clue: Bronchi diameter larger than adjacent pulmonary artery
Size: Cylindrical to varicose to saccular
Morphology: Bronchi can be filled with air, fluid, or mucus
CT Findings
Morphology: Direct
Bronchial dilatation
↑ Bronchoarterial ratio (signet-ring sign)
Normal bronchoarterial ratio (B/A) = 0.65-0.70
B/A > 1 not specific, seen in elderly (> 65 years old) or those at high altitude (due to mild hypoxia that dilates bronchi and causes vasoconstriction)
B/A > 1.5 indicative of bronchiectasis
Contour abnormality: Cylindrical, varicose, saccular
Cylindrical bronchiectasis: Uniform diameter
Varicose bronchiectasis: “String of pearls,” alternating dilatation & narrowing
Saccular or cystic bronchiectasis: “Cluster of grapes,” marked dilatation, rounded
Lack of bronchial tapering
Length of 2 cm distal to bifurcation
Earliest and most sensitive sign of bronchiectasis
Visibility of peripheral airways within 1 cm of costal pleura
Normal airways may be visible within 1 cm of mediastinal pleura
Morphology: Indirect
In bronchiectatic airways
Bronchial wall thickening
Mucoid impaction or fluid-filled bronchi
Bronchial artery hypertrophy
Distal to bronchiectatic airways
Centrilobular nodules or tree-in-bud opacities
Mosaic perfusion (air-trapping on expiratory scan)
Atelectasis or pneumonia distal to bronchiectasis
Interlobular septal thickening (60%)
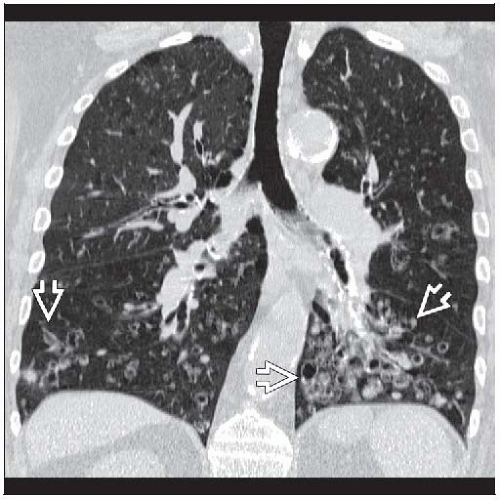
Distribution
Focal or diffuse
Focal: Confined to 1 lobe, usually postinfectious or secondary to aspiration
Focal: May be due to central obstructive lesion (slow-growing tumor, broncholith, foreign body)
Central bronchiectasis (normal peripheral airways)
Allergic bronchopulmonary aspergillosis
Tracheobronchomegaly
Williams-Campbell syndrome
Upper lobe predominant bronchiectasis
Cystic fibrosis
Allergic bronchopulmonary aspergillosis
Tuberculosis
Ventral bronchiectasis
Mycobacterial avium complex (Lady Windermere syndrome)
Postinfectious (childhood)
Most commonly basilar segments of lower lobes, with relative sparing of superior and anterior basilar segments
Left lower lobe involved 2x as often as right lower lobe
Correlation with pulmonary function
Extent of decreased attenuation most strongly correlated with decline in FEV1
Degree of bronchial wall thickness and extent of bronchiectasis also correlated with obstruction
Degree of bronchial wall thickening main indicator of declines in pulmonary function over time
Accuracy of CT in determining etiology
Correct diagnosis > 50% for cystic fibrosis, allergic bronchopulmonary aspergillosis, and tuberculosis
Radiographic Findings
Radiographic findings can be normal or nonspecific
Imaging Recommendations
Best imaging tool: CT much more sensitive than chest radiography
Protocol advice
Acute pneumonia may result in pseudobronchiectasis (functional bronchiectasis)
Bronchi dilated but not destroyed in response to acute inflammation
Bronchial dilatation may persist for 3-4 months after acute pneumonia
CT investigation for bronchiectasis should be delayed 6 months following pneumonia to avoid pitfall of pseudobronchiectasis
Other Modality Findings
Bronchography obsolete
DIFFERENTIAL DIAGNOSIS
Pneumonia
Bronchi often dilated in consolidated lung from acute pneumonia
Not true bronchiectasis; known as pseudobronchiectasis or functional bronchiectasis
Bronchi will return to normal in 3-4 months
Chronic Bronchitis
Bronchial wall thickening, but morphology normal
May be precursor to bronchiectasis
Bronchial Atresia
Dilated, mucous-filled bronchus distal to atretic segment (bronchocele)
Associated with marked hyperlucency & hypoperfusion of involved segment
Interestingly, even though airway obstructed, distal airways are usually not bronchiectatic
Cystic Lung Disease
Bronchiectasis maybe confused for cystic lung disease
Tracing cysts, in continuity with airways, helps to differentiate the 2
Langerhans cell histiocytosis
Irregular cysts can simulate bronchiectasis
Predominantly located in upper lung zones
Usually associated with solid nodules
Lymphangioleiomyomatosis
Uniform distribution of cysts in young women
Laryngeal papillomatosis
Airway nodules
Combination solid & cystic lung nodules
Cystic nodules may communicate with airways
PATHOLOGY