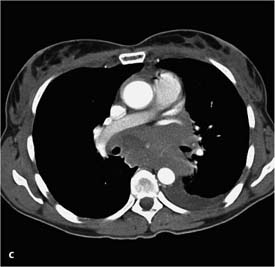
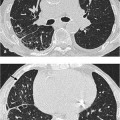
8 Bronchopulmonary Neoplasms Primary neoplasms of the lung and bronchial system. Most common cause of death from cancer Main risk factor is cigarette smoking; other factors include asbestos exposure. CT (including the adrenal region), PET (PET/CT) Pulmonary focal lesion of variable size (1–10 cm) with ill-defined margins and spicules Solid intrapulmonary mass of variable size; margins may be lobulated or spiculated More sensitive in detecting chest wall, plexus, or mediastinal involvement FDG-PET is the modality of choice for N and M staging (except for adenocarcinoma, where 30% false-negative findings occur) Spiculated nodule with or without hilar and mediastinal lymphomas. Confirm diagnosis by imaging studies and histologic examination Fig. 8.1 Peripheral bronchial carcinoma (large cell carcinoma) in a 45-year-old woman. The CT shows the spiculation clearly. It also shows isolated streaky densities consistent with a fingerlike pleural lesion or microatelectasis. Findings are almost pathognomonic for a peripheral bronchial carcinoma. Cough – Circumscribed local tumor (stages I and II): Surgery with or without adjuvant chemotherapy. – Locally advanced tumor (stage III): Combined radiation and chemotherapy or neoadjuvant multimodal therapy concepts. – Stage IV (M1 with malignant pleural effusion): Palliative chemotherapy or, where indicated, palliative radiation therapy. Five-year survival rate is about 10%, depending on the stage (stage Ia 75–80%, stage III b 5%) Staging – T staging: T1 = Tumor diameter less than 3 cm without involvement of the main bronchus (intrapulmonary tumor) Fig. 8.2 Peripheral bronchial carcinoma (noncornified squamous cell carcinoma, nonsmall cell lung cancer) in a 69-year-old man. The plain chest radiographs show a large, relatively well-demarcated tumorous mass in the right posterior lower lobe. The radiographic morphology suggests an adenocarcinoma. – N staging: N1 = intrapulmonary, ipsilateral peribronchial, or ipsilateral hilar lymph nodes Changes in the T categories (Goldstraw et al., 2007)
Nonsmall Cell Lung Cancer
Definition
 Epidemiology
Epidemiology
 More common in men than women
More common in men than women  Age 40–70
Age 40–70  A fundamental distinction is made between small cell lung cancer (SCLC, 15–20% of cases) and nonsmall cell lung cancer (NSCLC, 80–85%)
A fundamental distinction is made between small cell lung cancer (SCLC, 15–20% of cases) and nonsmall cell lung cancer (NSCLC, 80–85%)  Adeno-carcinoma is the most common type of nonsmall cell lung cancer (40%, acinar, papillary, bronchioalveolar, solid, mucus-forming), followed by squamous cell carcinoma (30%), and large cell carcinoma (15%).
Adeno-carcinoma is the most common type of nonsmall cell lung cancer (40%, acinar, papillary, bronchioalveolar, solid, mucus-forming), followed by squamous cell carcinoma (30%), and large cell carcinoma (15%).
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
Imaging Signs
 Modality of choice
Modality of choice
 Chest radiographs are not used in staging.
Chest radiographs are not used in staging.
 Radiographic findings
Radiographic findings
 Larger focal lesions are often lobulated
Larger focal lesions are often lobulated  Lesions occur more often in the upper lobe than lower lobe
Lesions occur more often in the upper lobe than lower lobe  Adenocarcinoma is usually peripheral
Adenocarcinoma is usually peripheral  Squamous cell carcinoma is usually central.
Squamous cell carcinoma is usually central.
 CT findings
CT findings
 Central necrosis occurs in squamous cell carcinoma
Central necrosis occurs in squamous cell carcinoma  Adenocarcinoma shows lesser density (ground-glass pattern)
Adenocarcinoma shows lesser density (ground-glass pattern)  Peritumoral lymphangitis and/or pulmonary metastases may be present
Peritumoral lymphangitis and/or pulmonary metastases may be present  Adenocarcinoma may occur in three forms (peripheral solitary, multilocular, pneumonia-like consolidation).
Adenocarcinoma may occur in three forms (peripheral solitary, multilocular, pneumonia-like consolidation).
 MRI
MRI
 Can exclude brain metastases.
Can exclude brain metastases.
 PET
PET
 MIBG-PET is used for tumors with neuroendocrine differentiation.
MIBG-PET is used for tumors with neuroendocrine differentiation.
 Pathognomonic findings
Pathognomonic findings
 Diagnostic steps in nonsmall cell lung cancer
Diagnostic steps in nonsmall cell lung cancer
 Exclude distant metastases
Exclude distant metastases  Determine resectability.
Determine resectability.
Clinical Aspects
 Typical presentation
Typical presentation
 Hemoptysis
Hemoptysis  Dyspnea
Dyspnea  Chest pain.
Chest pain.
 Therapeutic options
Therapeutic options
 Course and prognosis
Course and prognosis
 The slow-growing bronchioalveolar adenocarcinoma generally has a better prognosis.
The slow-growing bronchioalveolar adenocarcinoma generally has a better prognosis.
 What does the clinician want to know?
What does the clinician want to know?
 Complications
Complications  Monitoring treatment.
Monitoring treatment.
Staging
 TNM classification
TNM classification
 T2 = Tumor diameter greater than 3 cm with invasion of the main bronchus 2 cm distal to the carina, invasion of visceral pleura, or partial atelectasis or obstructive pneumonitis
T2 = Tumor diameter greater than 3 cm with invasion of the main bronchus 2 cm distal to the carina, invasion of visceral pleura, or partial atelectasis or obstructive pneumonitis  T3 = Tumor diameter greater than 7 cm with invasion of the chest wall, diaphragm, pericardium, mediastinal pleura, or main bronchus adjacent to the carina (distance to the carina < 2 cm, carina free of tumor) or complete collapse of one lung or a solitary tumor node in the same lobe
T3 = Tumor diameter greater than 7 cm with invasion of the chest wall, diaphragm, pericardium, mediastinal pleura, or main bronchus adjacent to the carina (distance to the carina < 2 cm, carina free of tumor) or complete collapse of one lung or a solitary tumor node in the same lobe  T4 = Any tumor invading the mediastinum, heart, major vessels, trachea, esophagus, spine, or carina; or separate tumor node or nodes in another ipsilateral pulmonary lobe.
T4 = Any tumor invading the mediastinum, heart, major vessels, trachea, esophagus, spine, or carina; or separate tumor node or nodes in another ipsilateral pulmonary lobe.
 N2 = ipsilateral mediastinal and/or subcarinal lymph nodes
N2 = ipsilateral mediastinal and/or subcarinal lymph nodes  N3 = contralateral mediastinal or hilar lymph nodes, or ipsilateral or contralateral scalene or supraclavicular lymph nodes
N3 = contralateral mediastinal or hilar lymph nodes, or ipsilateral or contralateral scalene or supraclavicular lymph nodes
 Stages in nonsmall cell lung cancer.
Stages in nonsmall cell lung cancer.
6th edition T and M description | 7th edition T and M |
T1 (≤ 2 cm) | T1a |
T1 (> 2–3 cm) | T1b |
T1 (≤ 5 cm) | T2a |
T2 (> 5–7 cm) | T2b |
T2 (> 7 cm) | T3 |
T3 (invasion) |
|
T4 (same lobe nodules) |
|
T4 (extension) | T4 |
M1 (ipsilateral lung) |
|
T4 (pleural effusion) | M1a |
M1 (contralateral lung) | M1a |
M1 (distant) | M1b |
Differential Diagnosis
Granuloma or tuberculoma | – Denser, more sharply demarcated, and rounder focal lesion – Calcifications – History and previous imaging studies |
Hamartoma | – Asymptomatic incidental finding – Popcorn calcifications |
Carcinoid | – Carcinoids, adenoid cystic carcinomas, and mucoepidermoid carcinomas primarily involve the central airways |
Tips and Pitfalls
N staging based on imaging morphology is unreliable—sensitivity is about 60%, specificity about 80%, negative predictive value about 55%, and positive predictive value about 80%.
Selected References
Gilman MD, Aquino SL. State-of-the-art FDG-PET imaging of lung cancer. Semin Roentgen-ol 2005; 40: 143–153
Goldstraw P et al. The IASLC lung cancer staging project: proposals for the revision of the TNM stage groupings in the forthcoming (7 th) edition of the TNM classification of malignant tumors. J Thorac Oncol 2007; 2: 706–714
Mohammed TH, White CS, Pugatch RD. The imaging manifestations of lung cancer. Semin Roentgenol 2005; 40: 98–108
Ravenel JG. Lung cancer staging. Semin Roentgenol 2004; 39: 373–385
Small Cell Lung Cancer
Definition
Aggressive, rapidly growing primary neoplasm of the bronchial system.
 Epidemiology
Epidemiology
A fundamental distinction is made between small cell lung cancer (SCLC, 15–20% of cases) and nonsmall cell lung cancer (NSCLC, 80–85%)  More common in men
More common in men  Age 40–70.
Age 40–70.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
Main risk factor is cigarette smoking.
Imaging Signs
 Modality of choice
Modality of choice
CT (including the adrenal region), PET (PET/CT)  Chest radiographs are not used in staging.
Chest radiographs are not used in staging.
 Radiographic findings
Radiographic findings
Hilar or mediastinal mass  A pulmonary focal lesion is the exception (< 10% of cases).
A pulmonary focal lesion is the exception (< 10% of cases).
 CT findings
CT findings
Large mediastinal and hilar tumor with bronchial obstruction  The mass may compress major vessels (vena cava, pulmonary artery)
The mass may compress major vessels (vena cava, pulmonary artery)  Obstructive atelectasis and/or pneumonitis.
Obstructive atelectasis and/or pneumonitis.
 MRI
MRI
Excludes brain metastases.
 PET
PET
FDG-PET is the modality of choice for staging (identifies disease as local or extended)  MIBG-PET identifies neuroendocrine tumors.
MIBG-PET identifies neuroendocrine tumors.
 Pathognomonic findings
Pathognomonic findings
Large mediastinal tumor involving the hilum.
 Diagnostic steps in small cell lung cancer
Diagnostic steps in small cell lung cancer
Confirm diagnosis by imaging studies and histologic examination  Determine stage of disease
Determine stage of disease  Limited program in extended disease.
Limited program in extended disease.
Clinical Aspects
 Typical presentation
Typical presentation
Cough  Hemoptysis
Hemoptysis  Dyspnea
Dyspnea  Chest pain.
Chest pain.
 Therapeutic options
Therapeutic options
Local disease: Multimodal curative approach with surgery, chemotherapy, and radiation  Extended disease: Palliative chemotherapy, with adjunctive radiation therapy where indicated.
Extended disease: Palliative chemotherapy, with adjunctive radiation therapy where indicated.
 Course and prognosis
Course and prognosis
With treatment, 5-year survival rate is 10–20% in local disease and 0–10% in extended disease.
 What does the clinician want to know?
What does the clinician want to know?
Staging  Complications
Complications  Monitoring treatment.
Monitoring treatment.
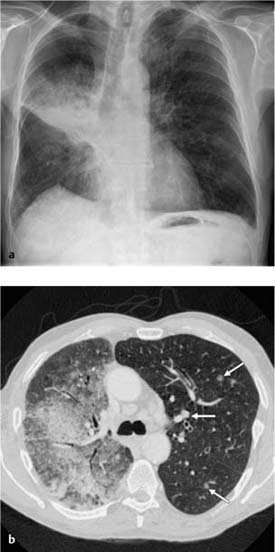
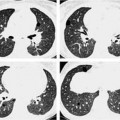
Fig. 8.3 Small cell bronchial carcinoma in a 40-year-old woman with back pain from spinal metastases.
a The plain chest radiograph shows an extensive mediastinal tumor without signs of a pulmonary lesion.
b, c On CT the findings appear as a conglomerate of lymph nodes involving all mediastinal compartments. Associated pleural effusion on the left side. The central tracheo-bronchial system appears normal. Only repeated bronchoscopy demonstrated the shallow tumor in the right main bronchus.
 Staging
Staging
Local disease: Tumor limited to mediastinum, hila, and supraclavicular region  Extended disease: Extrathoracic manifestation or pulmonary metastases, malignant pleural effusion, axillary lymph node involvement.
Extended disease: Extrathoracic manifestation or pulmonary metastases, malignant pleural effusion, axillary lymph node involvement.
Differential Diagnosis
Lymphoma or lymph node metastases | – Usually no signs of obstruction such as atelectasis, compression of the vena cava, or invasion or obstruction of the pulmonary artery. |
Benign lymphadenopathy | – Usually smaller lymph nodes that are distinguishable from each other |
Nonsmall cell lung cancer | – Pulmonary focal lesion – Fewer hilar and/or mediastinal lymph node metastases |
Tips and Pitfalls
Primary site of small cell lung cancer is often unidentifiable on imaging studies.
Selected References
Gilman MD, Aquino SL. State-of-the-art FDG-PET imaging of lung cancer. Semin Roentgen-ol 2005; 40: 143–153
Irshad A, Ravenel JG. Imaging of small cell lung cancer. Curr Probl Diagn Radiol 2004; 33: 200–211
Bronchioalveolar Carcinoma—Alveolar Cell Carcinoma
Definition
 Epidemiology
Epidemiology
Variant of adenocarcinoma  2–5% of all lung carcinomas
2–5% of all lung carcinomas  More common in men than in women
More common in men than in women  Peak age is about 50.
Peak age is about 50.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
Arises from type II pneumocytes and bronchiolar epithelium  Not associated
Not associated  Scarring predisposes
Scarring predisposes  Spreads along the peripheral airways (bronchioloalveolar spread).
Spreads along the peripheral airways (bronchioloalveolar spread).
Imaging Signs
 Modality of choice
Modality of choice
CT.
 Radiographic findings
Radiographic findings
Forms: Peripheral nodules or pneumonia-like infiltrate  Solitary (80% of cases) or multilocular to disseminated (20%).
Solitary (80% of cases) or multilocular to disseminated (20%).
 CT findings
CT findings
– Broad morphologic spectrum: Peripheral nodule (ill-defined margins, lobulated or spiculated, satellite lesions)  Consolidation of a relatively low density (mucinous subtype) with CT angiogram sign, air bronchogram, and bronchiolo-gram (“air bubbles” in 50% of cases)
Consolidation of a relatively low density (mucinous subtype) with CT angiogram sign, air bronchogram, and bronchiolo-gram (“air bubbles” in 50% of cases)  Multilocular, unilateral or bilateral, disseminated appearances.
Multilocular, unilateral or bilateral, disseminated appearances.
– Density: Solid  Ground-glass
Ground-glass  Mixed.
Mixed.
– Collateral findings: Peripheral halo  Peritumoral lymphangitis (“crazy paving”)
Peritumoral lymphangitis (“crazy paving”)  Peritumoral centrilobular nodules (bronchogenic spread)
Peritumoral centrilobular nodules (bronchogenic spread)  Pulmonary metastases or multicentric tumors
Pulmonary metastases or multicentric tumors  Pleural effusion (30% of cases)
Pleural effusion (30% of cases)  Lymph-adenopathy (20%).
Lymph-adenopathy (20%).
 FDG-PET
FDG-PET
High rate of false-negative findings.
 Pathognomonic findings
Pathognomonic findings
Chronic, progressive lobar or multilobar infiltrate.
Clinical Aspects
 Typical presentation
Typical presentation
Incidental finding in nearly asymptomatic patients, or patients may have a cough with bronchorrhea and dyspnea.
 Confirmation of the diagnosis
Confirmation of the diagnosis
Bronchoalveolar lavage and transbronchial biopsy.
 Therapeutic options
Therapeutic options
Tumor resection where findings are localized  Radiation therapy and chemo-therapy are indicated for nonresectable tumors.
Radiation therapy and chemo-therapy are indicated for nonresectable tumors.
 Course and prognosis
Course and prognosis
Prognosis is better than for other lung carcinomas due to the slow growth  Resectable tumors have a 5-year survival rate of 75%.
Resectable tumors have a 5-year survival rate of 75%.
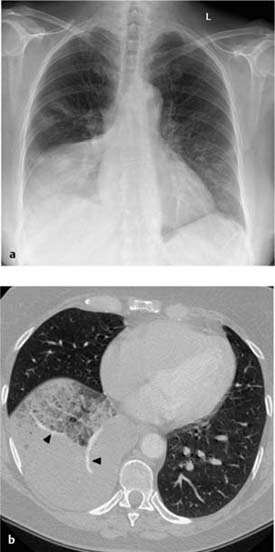
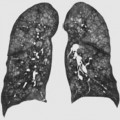
Fig. 8.4 Bronchioalveolar carcinoma (alveolar cell carcinoma) in a 65-year-old man.
a The plain chest radiograph shows a pneumonia-like infiltrate on the right side involving primarily the apical segments of the lower lobe and the perihilar region.
b The area of the infiltrate is hypodense on CT so that the larger vessels are delineated in addition to an air bronchogram (CT angiogram sign). Mediastinal lymphadenopathy and isolated focal infiltrates are also seen on the left side (arrows).
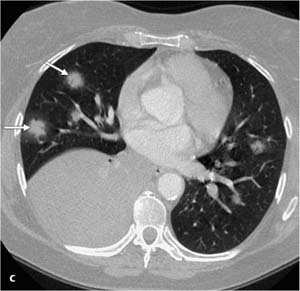
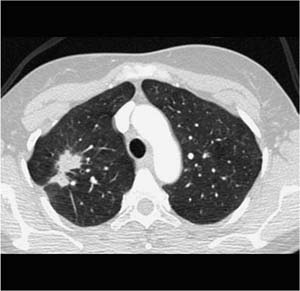
Fig. 8.5 Bronchioalveolar carcinoma (alveolar cell carcinoma) in a 60-year-old woman.
a The plain chest radiograph shows a pneumonia-like infiltrate in the right lower lobe and bilateral isolated, ill-defined focal opacities, more pronounced on the right than on the left.
b, c On CT the infiltrate appears partially as a homogeneously dense acinar shadow and partially as a less pronounced density resembling a ground-glass opacity. The CT angiogram sign (arrowhead) is prominent in both segments. The additional focal infiltrates in both lungs show a halo sign (arrows).
 What does the clinician want to know?
What does the clinician want to know?
Resectability (staging as in nonsmall cell lung cancer)  Course.
Course.
Differential Diagnosis
Peripheral bronchial carcinoma | – No air bronchogram or bronchiologram |
Pneumonia | – Symptoms of infection – Responds to antibiotics |
Cryptogenic organizing pneumonia | – Fluctuating picture – Responds to steroids |
Wegener granulomatosis | – Renal insufficiency – Sinus involvement |
Sarcoidosis |

 M1a = Separate tumor node or nodes on the contralateral lung, pleural nodes, or malignant pleural effusion
M1a = Separate tumor node or nodes on the contralateral lung, pleural nodes, or malignant pleural effusion  M1b = Distant metastases
M1b = Distant metastases