Fig. 49.1
Example of a one-way implantable valve (zephyr). The design allows for air and mucous to escape through the valve. The device is placed via a catheter-based system
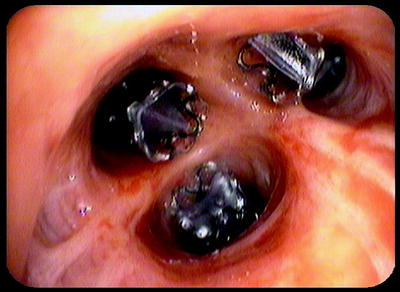
Fig. 49.2
Three valves are placed into the segments of a right upper lobe in a patient with emphysema with the goal to achieve complete occlusion and atelectasis
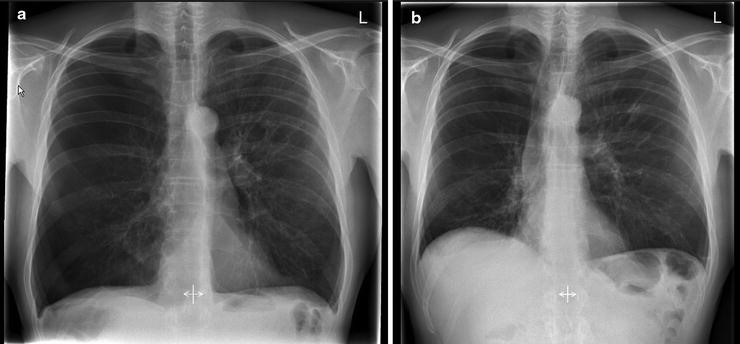
Fig. 49.3
Chest X-ray of the patient shown in Fig. 49.2. The X-ray on the left shows the hyperinflated lungs and depressed diaphragm. The X-ray on the right demonstrates right upper lobe collapse, volume reduction, and a more normal diaphragm configuration
The Endobronchial Valve for Emphysema Palliation Trial (VENT) study was a multicenter, randomized, controlled study that enrolled 220 patients in North America and 111 patients in Europe into the intervention arms. Patients with heterogeneous emphysema as determined by quantitative high-resolution computed tomography (CT) were treated with unilateral therapy targeting lobar exclusion. The North American data showed modest improvements in spirometry and quality of life as measured on the SGRQ at 6 months. The increase in forced expiratory volume in 1 s (FEV1) was 4.3%, and the difference between the intervention and the control arms was 6.8%. The difference in 6-min walk was 5.8%. Complications were manageable, including COPD exacerbations, pneumothorax, hemoptysis, and pneumonia, and acceptable in rate. There was no procedure-related mortality. Valves were removed during the study in 31 patients for reasons such as valve migration, pneumonia, and COPD exacerbations. Valve removal is generally easily performed with conventional biopsy forceps, and this reversibility presents a major attraction of this technique.
Over 40% of trial sites reported technical error rates of greater than 10% in valve placement, suggesting that technical success cannot be taken for granted. Patients who had evidence of complete interlobar fissures on pre-procedure CT had incremental improvements of forced expiratory volume at 1 s (FEV1) over those who did not, and the efficacy was further improved in the subgroup of patients who actually achieved lobar isolation.
Using either EBV or IBV valves, lobar atelectasis was not achieved in the majority of patients even with a lobar exclusion approach, whereby all the bronchi to a target lobe were occluded. In the VENT study, only 22% of patients showed complete interlobar fissures and lobar collapse at 1 year. However, the greatest benefits appear to be found in these patients who do develop target lobe atelectasis because of favorable changes in chest wall dimensions.
More limited symptomatic benefits have also been found in a large proportion of COPD patients treated with endobronchial valves despite the absence of any lobar collapse suggesting a role for other physiological mechanisms. It is postulated that by occluding airways, valves increase resistance to airflow such that air is diverted to other relatively less emphysematous parts of the lung resulting in reduced air trapping and dynamic hyperinflation. Moreover, by excluding the most diseased parts of the lung from gas exchange, physiological dead space can be reduced by an interlobar shift of ventilation from the treated lobe to untreated regions of the lung. This is matched by changes in perfusion as a result of hypoxic vasoconstriction and results in better ventilation-perfusion matching in the untreated, more normal lung regions.
Thermal Vapor Ablation
Controlled doses of steam, when delivered to a segmental airway, can produce an inflammatory response that results in lung volume reduction by creating scar formation. The advantage of this technique is that no prosthesis needs to be inserted. The degree of collateral ventilation is also not an issue because the treatment works at the level of the lung parenchyma. Targeting can be staged with several or single segments added in procedures. The energy dose considers the target tissue mass as determined by CT imaging, and a time is calculated to achieve the desired energy delivery. It is therefore crucial to know exactly at which segment or lobe one wants to isolate, as it determines the treatment algorithm based on the dependant lung mass. It appears that 10 cal/kg is the most commonly dose used in current trials. Procedures are currently mainly performed under general anesthesia to completely control cough and balloon placement. A reusable 2-mm vapor catheter is inserted via flexible bronchoscopy to the target airways (Fig. 49.4). On the vapor catheter, there is a distal occlusion balloon that isolates the lung segment. An electronically controlled pressure vessel generated precise doses of steam that is then delivered to the isolated airways. Airways do show immediate post-procedural blanching, but there are few specific side effects.
Fig. 49.4
Schematic of treatment stages with steam application (Courtesy of Uptake Medical)
The procedure is irreversible (Fig. 49.5), and large-scale or long-term data is not yet available, but results from pilot trials have shown promising results (Fig. 49.6).
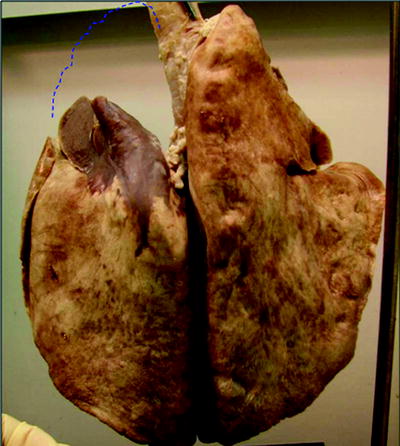
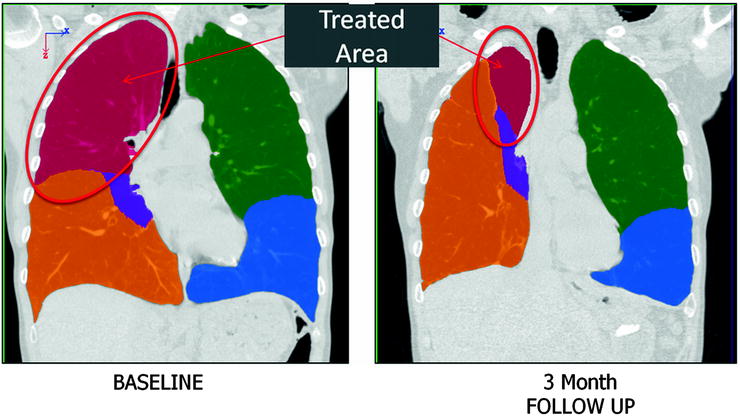
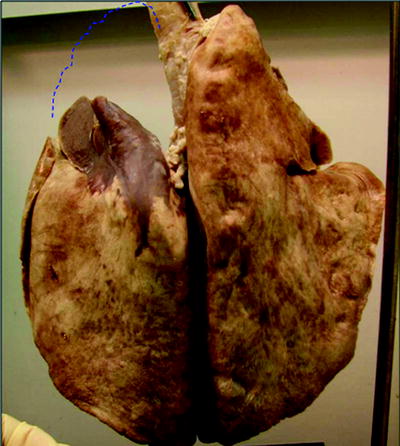
Fig. 49.5
Explanted lung of a sheep treated with steam 3 months prior. The volume reduction in the treated area is clearly visible
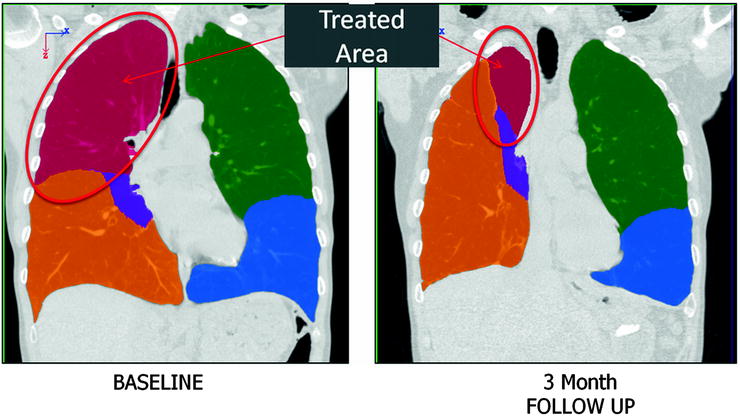
Fig. 49.6
Schematic coloration of an X-ray of a patient who had received steam treatment to the right upper lobe. The left image shows the baseline and the right image the change after 3 months. The volume reduction of the right upper lobe is delineated
Biological Lung Volume Reduction
Biological agents aim to reduce lung volume by blocking off the most emphysematous areas with a rapidly polymerizing sealant. Similar to vapor treatment, the mechanism of action involves resorption atelectasis from airway occlusion, subsequent airspace inflammation, and then remodeling. This remodeling will lead to scarring that induces contraction of lung parenchyma, and functional volume reduction can be expected within 6–8 weeks. The sealant causes blockage of interalveolar as well as bronchiolar-alveolar collateral channels and negates the effects of collateral ventilation.
After identifying a target region, the distal airways in this segment are collapsed by wedging the flexible bronchoscope in the bronchial orifice and applying suction. The liquid sealant in predetermined dose is then injected, and the wedging position is held for a short period of time.
Biological lung volume reduction therapy did bear significant promise. It was instituted in 50 patients with upper lobe predominant emphysema in a phase 2 multicenter trial. Serious adverse events were documented in four patients due to aspiration, pneumonia, pulmonary embolism, and a fall related to analgesia. However, there were no documented fatalities. COPD exacerbations were observed in 28% (14/50) although three events were thought not to be procedure related. Postoperative leukocytosis, fever, or malaise occurred in 89% over the first 24 h. The primary endpoint of a significant reduction in air trapping was sustained at 6 months in only the patients receiving high-dose therapy (20 ml per subsegment compared to 10 ml). Spirometric improvements and radiological evidence of remodeling were also greater in patients who received high-dose treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree