Fig. 19.1
Linear EUS-FNA scope (Hitachi-Pentax FG 34 UX) with a convex linear array ultrasound transducer, sheet, and 22-gauge needle
Esophageal ultrasound is performed in fasting patients lying in a left lateral position under conscious sedation using a low dose of midazolam. A thorough knowledge of mediastinal anatomy is a prerequisite for an EUS investigation as only ultrasound images are available for orientation. A standardized EUS evaluation in patients with (suspected) lung cancer starts by identifying the left adrenal gland from the stomach. Subsequently, the endoscope is retracted stepwise while making circular movements in order to visualize all mediastinal nodes that can be detected from the esophagus. The following anatomical landmarks are used for orientation: celiac axis, liver, vena cava, right atrium, left atrium, pulmonary artery, and aorta. Nodes that are observed by EUS are described in relation to those vascular structures and given the appropriate number according to the TNM classification system. Lesions adjacent to the esophagus can be aspirated under real-time ultrasound control. Nodes with a round shape, a short axis > 10 mm, sharp demarcation, and a hypoechoic echo texture are more likely to be malignant involved. Elastography, a novel technique measuring tissue stiffness (Fig. 19.2), might be helpful in selecting the optimal target area to obtain tissue.
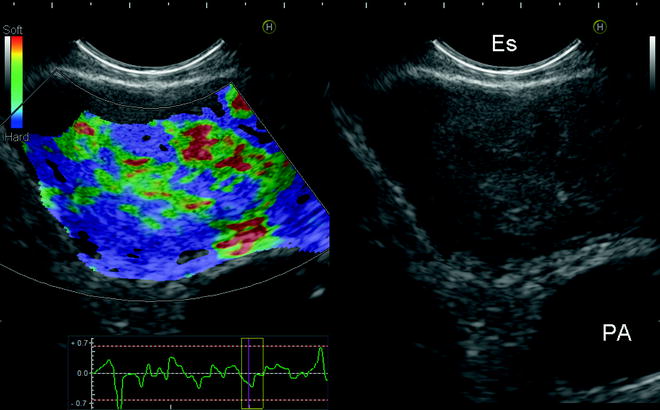
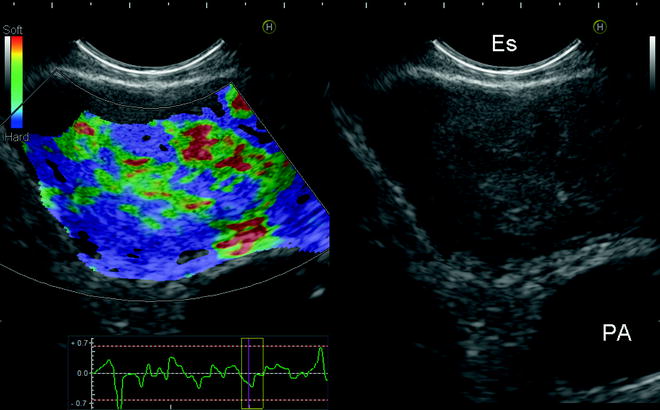
Fig. 19.2
EUS image of a subcarinal mass (station 7) in the left–panel “elastography” is used. Blue colors correspond with areas of increased tissue stiffness in comparison to the red and green areas. PA pulmonary artery, ES esophagus
In the absence of on-site cytology, four needle passes will result in an optimal yield and minimize false-negative results. The standard needle size is 22 gauge, but also 19 gauge and Tru-Cut needles are available. Suction is mostly applied, but the necessity of it has been questioned in recent studies. From the aspirates, tissue blocks can be made on which immunohistochemistry staining and molecular analysis can be performed. On average, an evaluation of the left adrenal gland and all mediastinal nodes that can be detected by EUS including aspirations takes around 20 min. Importantly, EUS has a very low complication rate and is well tolerated by patients. This is especially of importance in patients with severe COPD and an advantage to an endobronchial approach.
Mediastinal EUS can be taught to chest physicians without prior gastroscopy or ultrasound experience applying a limited but dedicated implementation strategy. Learning EUS anatomy is the most time consuming; the actual aspiration of nodes is relatively straightforward and easier in comparison to a transbronchial route due to the absence of the cartilage rings. Training tools to assess competency in EUS are under evaluation.
Lung Cancer
Diagnosing and staging of lung cancer is the most common indication for EUS-FNA in pulmonary medicine (Table 19.1). By providing tissue proof of a mediastinal nodal metastasis, a diagnosis and locoregional staging can be achieved with a single minimally invasive test. Besides nodal staging, EUS-FNA can be used to obtain tissue of centrally located intrapulmonary tumors and the left adrenal gland.
Table 19.1
Indications for esophageal ultrasound (EUS) in chest diseases
Suspected lung cancer |
– Enlarged or PET-positive mediastinal lymph nodes within reacha |
– Primary lung tumor located adjacent to the esophagus |
Staging of non-small cell lung cancer |
– Mediastinal staging (regardless of nodal size at CT) |
– Mediastinal involvement at FDG-PETa |
– Mediastinal restaging after induction chemotherapya |
– Suspected mediastinal tumor invasion (T4) |
– Suspected left adrenal metastasis |
Analysis of mediastinal masses |
– Solitary mediastinal masses |
– Suspected mediastinal metastases in patients with (previous) extrathoracic cancera |
Suspected sarcoidosis |
Nodal Staging
EUS-FNA provides access to nodes located in lower mediastinum (subcarinal region station 7) (Fig. 19.3), lower paraesophageal area (station 8), and pulmonary ligament (station 9). Nodes located paratracheally to the left (station 4L) (Fig. 19.4), in the aortopulmonary window (station 5) (Fig. 19.5), and the para-aortal region (Fig. 19.6) can be detected by esophageal ultrasound. Aspiration of small left paratracheal nodes is often easier from the esophagus (Fig. 19.4B) – in comparison to an EBUS approach – due to absence of cartilage rings and cough reflexes. The aortopulmonary nodes can only be aspirated safely in selected cases due to the intervening pulmonary artery (Fig. 19.5B). The para-aortal nodes (Fig. 19.6) can be approached transaortally. Nodes paratracheally to the right (stations 2R and 4R) can regularly only be detected by EUS when enlarged. The esophagus is located in a left dorsal position in relation to the trachea, so air prevents visualization of these mediastinal areas. For enlarged nodes (short axis > 10 mm), EUS has a sensitivity of 90 %. EUS can also be used for a reevaluation of the mediastinum after induction chemotherapy.
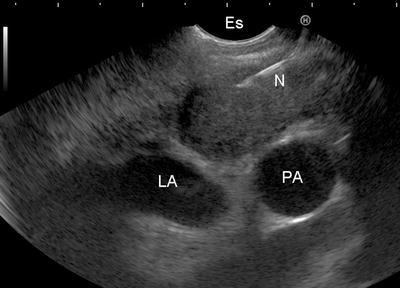
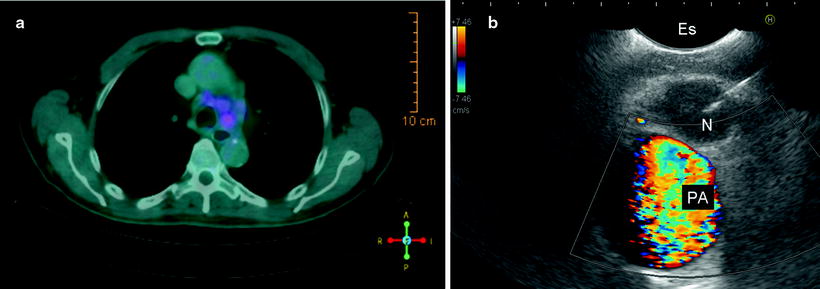
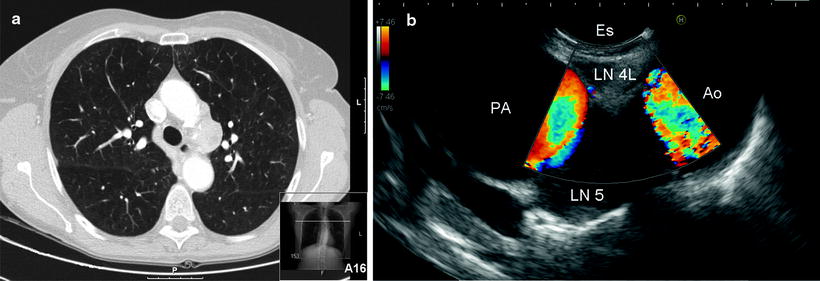
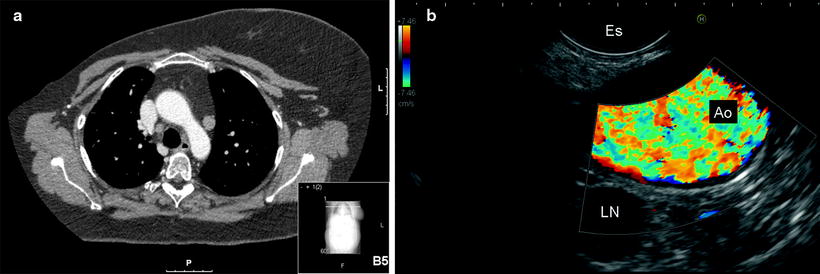
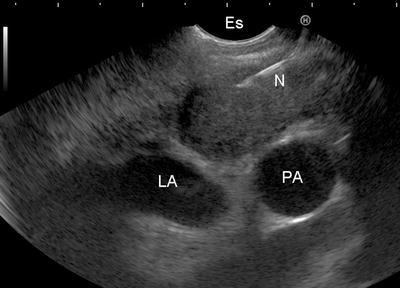
Fig. 19.3
EUS-guided fine-needle aspiration (N) of a subcarinal node (station 7) located between esophagus (ES), left atrium (LA), and pulmonary artery (PA)
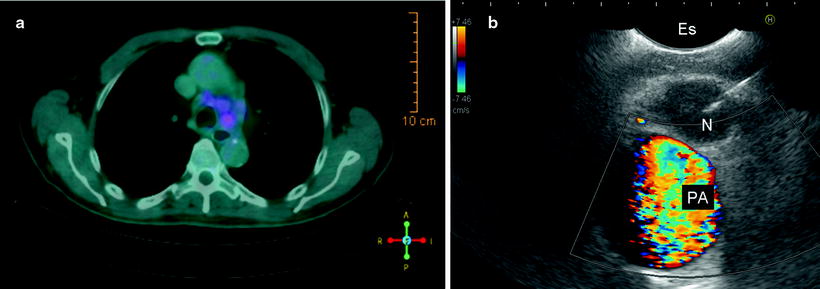
Fig. 19.4
(a) Integrated positron emission and computed tomography (PET-CT) scan with FDG uptake in a lower left paratracheal node (station 4L). (b) Corresponding EUS-guided FNA (N needle) of the lower left paratracheal lymph nodes located between the esophagus (Es) and pulmonary artery (PA)
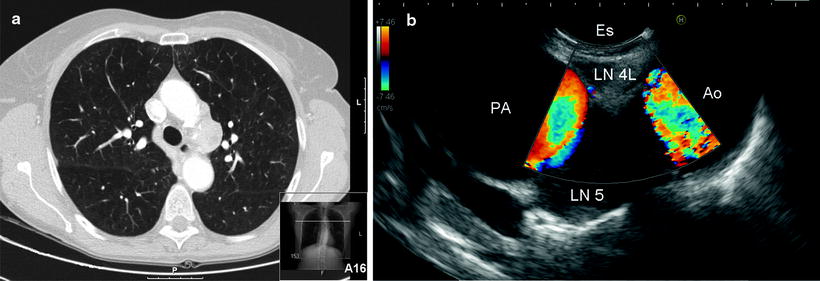
Fig. 19.5
(a) Computed tomography of the chest showing enlarged mediastinal nodes in the aortopulmonary window (station 5). (b) Corresponding EUS image, showing the left lower paratracheal node (station 4L) and the nodes in the aortopulmonary window. AO aorta, PA pulmonary artery, ES lumen of the esophagus
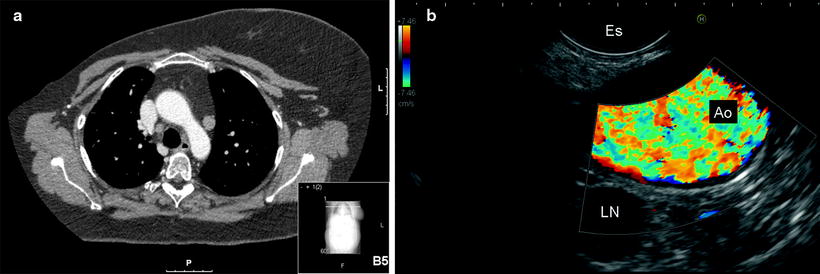
Fig. 19.6
(a) Computed tomography of the chest demonstrating a para-aortal node (station 6). (b) Corresponding EUS image, the para-aortal node (LN) is seen transaortally (AO). ES esophagus
Tumor Staging
Centrally located intrapulmonary tumors located adjacent or near the esophagus (Fig. 19.7) or aorta (Fig. 19.8) can be detected and aspirated by EUS. For those patients with a centrally located lung tumor without endobronchial abnormalities, EUS is often an accurate and safe test to obtain a tissue diagnosis. EUS provides an attractive alternative to CT-guided biopsy; the latter is often not possible due to the close proximity of the pulmonary vasculature and increased risk of pneumothorax. In addition to assessing a tissue diagnosis, EUS can often make an assessment regarding the presence (Fig. 19.9) or absence (Fig. 19.8B) of mediastinal/vascular tumor invasion (T4 tumor, stage IIIB).
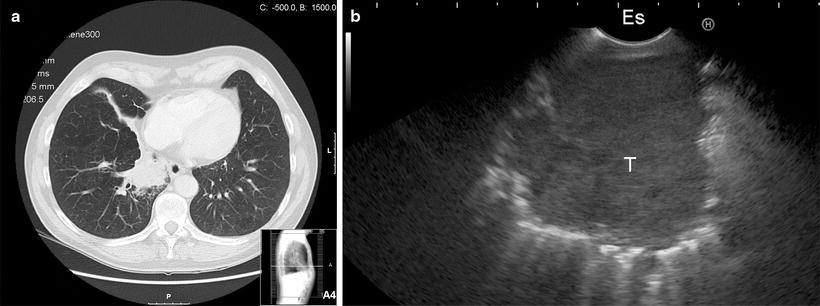
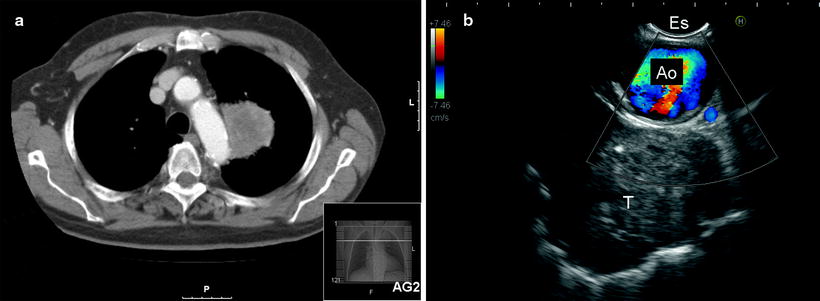
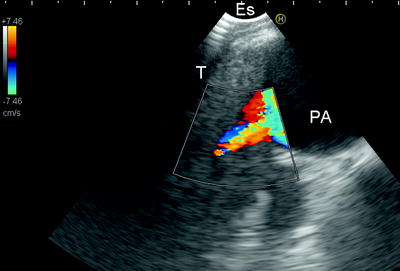
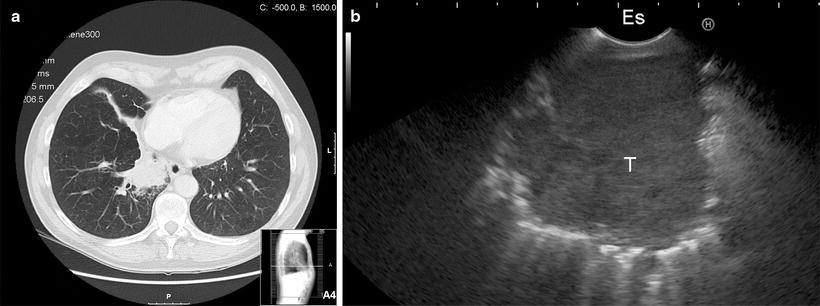
Fig. 19.7
(a) CT scan of the chest showing a centrally located right lower lobe tumor. No diagnosis was obtained with bronchoscopy. (b) Corresponding EUS image showing the right lower lobe tumor (T) from the esophagus (ES). The diagnosis squamous cell carcinoma was made by EUS-FNA
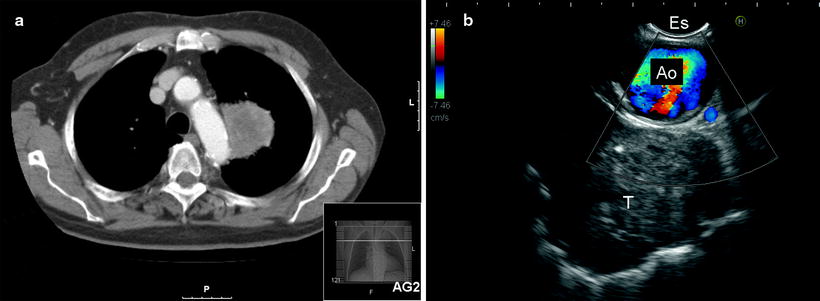
Fig. 19.8
(a) CT scan of the chest demonstrating a tumor of the left upper lobe located adjacent to the aorta. (b) Corresponding EUS image showing the left upper lobe tumor (T). The aorta (AO) functions as an ultrasound window. There are no signs of aortic invasion. ES esophagus
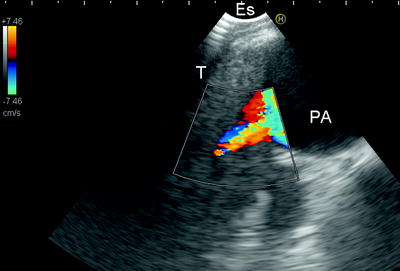
Fig. 19.9
EUS image of centrally located left side tumor (T) invading the pulmonary artery (PA). Images are compatible with T4 (stage IIIB)
Left Adrenal Gland
The left adrenal gland is a predilection site of metastatic spread for bronchogenic carcinoma. From the stomach, the left adrenal gland can be detected and typically presents with a seagull shape (Fig. 19.10). Loss of the “seagull shape” (Fig. 19.11), increased size, and FDG-PET uptake are predictors for malignant involvement.
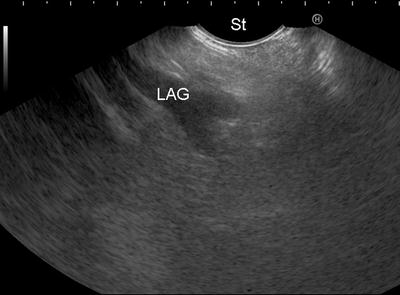
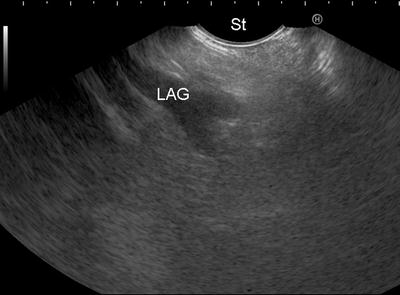
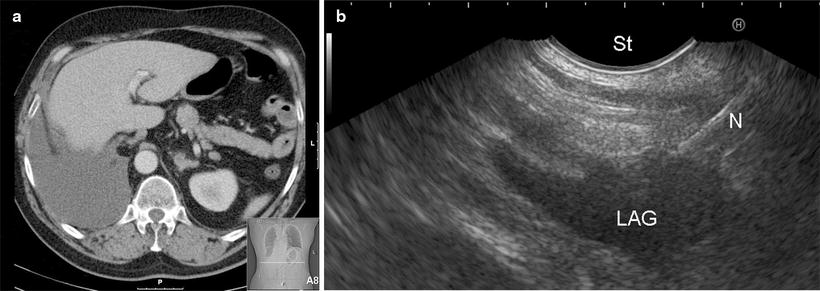
Fig. 19.10
Transgastric EUS image of normal-sized and normal-shaped left adrenal gland (LAG). Notice the typical “seagull” shape. St stomach
Endosonography in Lung Cancer Staging Algorithms
EUS is a safe, minimally invasive, and accurate technique to detect mediastinal tumor spread within their diagnostic reach. EUS can prevent 50–70 % of scheduled mediastinoscopies by providing tissue proof of advanced disease in patients with (suspected) lung cancer and enlarged or PET-positive nodes. However, EUS has limitations in excluding malignant nodal involvement. Several studies have shown that a complete endosonographic evaluation – combining an esophageal and endobronchial approach – improves nodal staging versus each of the techniques alone. EUS has a complementary value to both EBUS and mediastinoscopy especially for nodes located in the lower mediastinum and aortopulmonary window. Additionally, mediastinal tumor invasion can be diagnosed as well as left adrenal metastases (Table 19.2). A complete endosonography evaluation of the mediastinum is at least as good as mediastinoscopy but is associated with fewer complications. Therefore, endosonography – and not mediastinoscopy – qualifies as the initial mediastinal tissue staging test. Performing mediastinoscopy after a negative endosonography improves the sensitivity of mediastinal nodal staging from 85 % to 94 %. Whether all patients staged negative by endosonography – or a selected subgroup – should subsequently undergo surgical staging of the mediastinum is under discussion. Ongoing studies focus on predictors for false-negative endosonography results.
Table 19.2
Added value of esophageal to endobronchial ultrasound
Complementary diagnostic reach |
– Lower mediastinum: stations 8 and 9 |
– Aortopulmonary window: station 5 (only in selected cases) |
– Para-aortal region: station 6 (transaortal approach) |
– Left adrenal gland |
– Lung tumors located adjacent to the esophagus |
Histology sampling possible (19-gauge, Tru-Cut, Quick core needles) |
Well tolerated by patients (no coughing or dyspnea) |
Granulomatous Diseases
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree