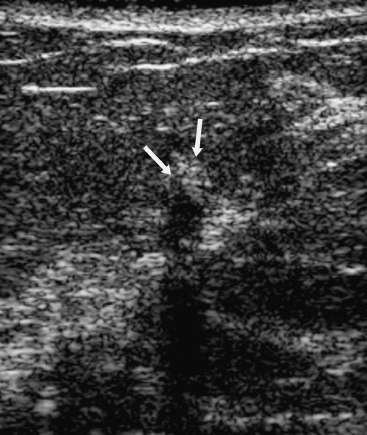
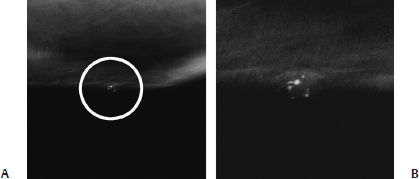
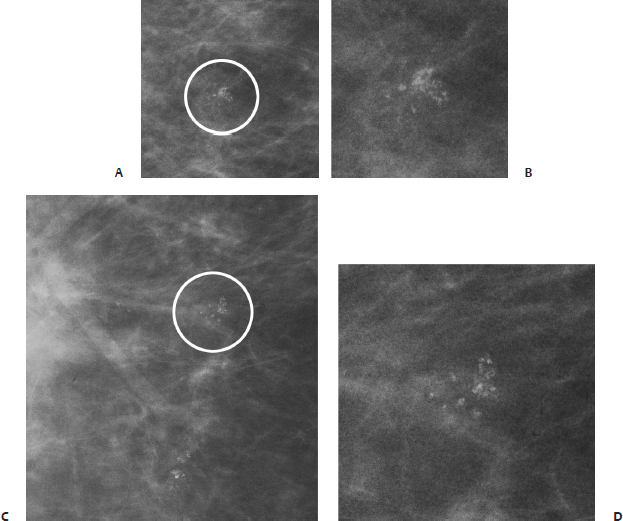
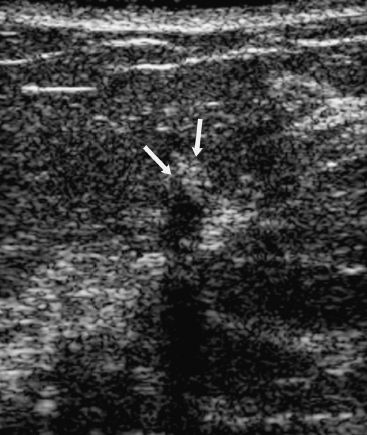
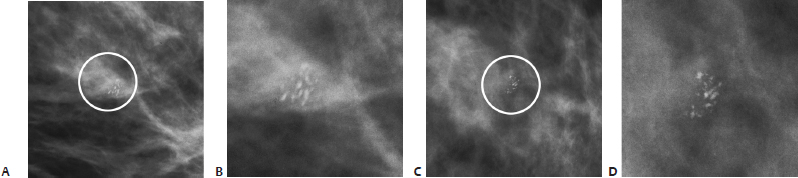
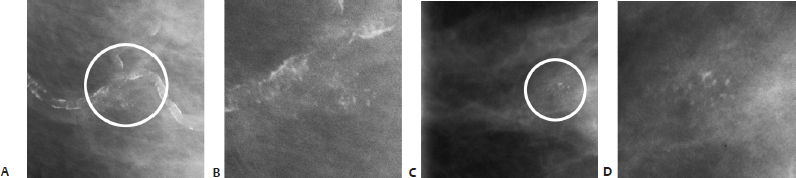
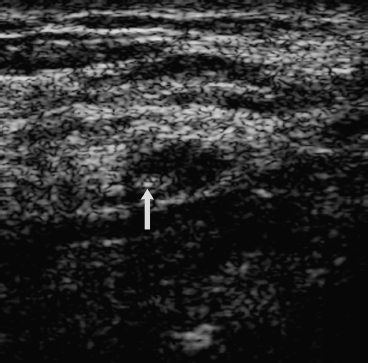
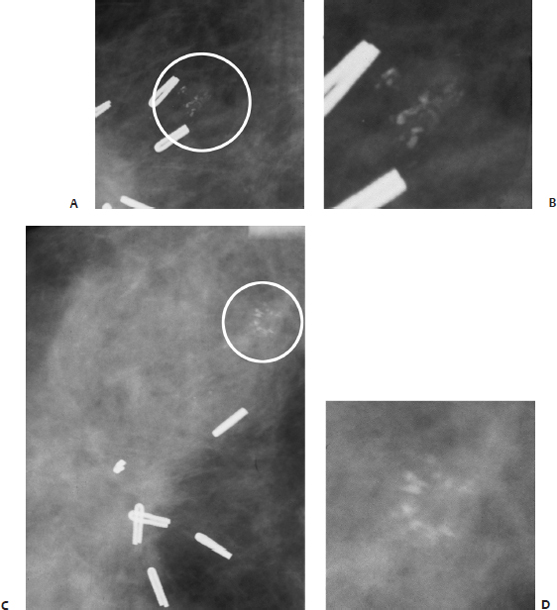
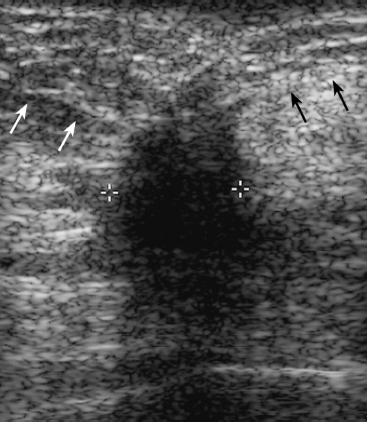
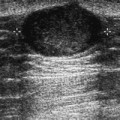
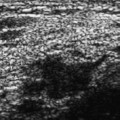
18 Calcifications: Heterogeneous/ Pleomorphic Microcalcifications A 44-year-old woman presents with new densities on her screening mammogram. • Right breast: white Desitin cream • Left breast: normal exam Calcifications (Figs. 18.1 and 18.2) • Type: pleomorphic/heterogeneous • Distribution: grouped/clustered Fig. 18.1 In the 6 o’clock position of the right breast, there is a cluster of heterogeneous densities (circle). (A) Right MLO mammogram. (B) Right CC mammogram. (C) Right MLO spot magnification mammogram. (D) Right CC spot magnification mammogram. Fig. 18.2 (A) Right ML spot magnification mammogram. The heterogeneous densities are within the skin (circle). (B) Enlargement of circled calcifications in A. • Desitin ointment on skin • BI-RADS assessment category 2, benign finding • The cream could not be removed even after scrubbing with alcohol. The patient was advised to stop using the cream and return in 2 months. The mammogram 2 months later showed no abnormal densities. Skin powders and ointments may cause amorphous or heterogeneous densities, which are commonly faint, unusual in appearance, or only visible on one view. Jackson VP, Jahan R, Fu YS. Benign breast lesions. In: Bassett LW, Jackson VP, Jahan R, Fu YS, Gold RH, eds. Diagnosis of Diseases of the Breast. Philadelphia: WB Saunders; 1997:357–443 A 68-year-old woman presents with increasing number of calcifications on her right breast screening mammogram. • Normal exam Calcifications (Fig. 18.3) • Type: pleomorphic/heterogeneous • Distribution: grouped/clustered Fig. 18.3 In the right upper outer breast, there is a cluster of pleomorphic calcifications (circle). (A) Right ML magnification mammogram. (B) Enlargement of circled calcifications in A. (C) Right CC magnification mammogram. (D) Enlargement of circled calcifications in C. Frequency • 11.5 MHz (Fig. 18.4) Fig. 18.4 Right transverse breast sonogram. The mammographic calcifications correspond to multiple high-intensity foci (arrows) associated with posterior acoustic shadowing. No sonographic mass is present. • Fibrocystic changes • Predominantly fatty tissue with benign calcifications in small area of stromal fibrosis and epithelial hyperplasia • BI-RADS assessment category 4, suspicious abnormality; biopsy should be considered. • Clustered heterogeneous calcifications are due to both benign and malignant etiologies. Benign etiologies include early calcification of fibroadenomas or fat necrosis. Papillomas and fibrocystic changes may also produce these types of calcifications. Malignant causes include ductal carcinoma in situ and invasive ductal carcinoma. Bird RE. Critical pathways in analyzing breast calcifications. Radio-graphics 1995;15(4):928–934 A 69-year-old woman presents with new left breast calcifications. • Normal exam Calcifications (Fig. 18.5) • Type: pleomorphic/heterogeneous • Distribution: grouped/clustered Fig. 18.5 A cluster of pleomorphic calcifications (circle)is in the left outer inferior breast. (A) Left ML magnification view. (B) Enlargement of circled calcifications in A. (C) Left CC magnification view. (D) Enlargement of circled calcifications in C. • Fibroadenomatoid hyperplasia • BI-RADS assessment category 4, suspicious abnormality; biopsy should be considered. • Fibroadenomatous hyperplasia is an early stage of fibroadenoma formation. Calcifications formed during this process may be indistinguishable from malignant calcifications. Kamal M, Evans AJ, Denley H, Pinder SE, Ellis IO. Fibroadenomatoid hyperplasia: a cause of suspicious microcalcification on mammographic screening. AJR Am J Roentgenol 1998;171(5):1331–1334 Tavassoli FA, Fattaneh A. Pathology of the Breast. 2nd ed. Stamford: Appleton& Lange; 1999:590–597 An 80-year-old woman presents with new calcifications on her screening mammogram. • Normal exam Calcifications (Fig. 18.6) • Type: pleomorphic/heterogeneous • Distribution: grouped/clustered Fig. 18.6 In the left upper outer quadrant, there is a cluster of calcifications (circle). (A) Left LM magnification mammogram. (B) Enlargement of circled calcifications in A. (C) Left CC magnification mammogram. (D) Enlargement of circled calcifications in C. Low Frequency Frequency • 7 MHz (Fig. 18.7) Mass • Margin: well defined, oval/round • Echogenicity: hypoechoic • Retrotumoral acoustic appearance: no shadowing • Shape: ellipsoid Fig. 18.7 Left radial low-frequency breast sonogram. The calcifications (arrow) identified in Fig. 18.6 are associated with a hypoechoic mass. With this lower frequency, the hypoechoic mass is not well identified. High Frequency (Fig. 18.8) Frequency • 11.5 MHz Fig. 18.8 Left radial high-frequency breast sonogram. The calcifications (arrow) are within a well-defined, oval, hypoechoic mass. The mass is more clearly identified with this high-frequency technique compared with the low-frequency exam. • Fibroadenoma (not otherwise specified) • BI-RADS assessment category 4, suspicious abnormality; biopsy should be considered. • Although the mass has a more benign appearance on the higher-frequency sonographic exam, the small size prevents confident definition of the margins. This limitation and the presence of suspicious mammographic calcifications result in a suspicious, category 4 assessment. Bassett LW. Mammographic analysis of calcifications. Radiol Clin North Am 1992;30(1):93–105 Gershon-Cohen J, Ingleby H. Roentgenography of fibroad-enoma of the breast. Radiology 1952;59(1):77–87 Kopans DB. Breast Imaging. 2nd ed. Philadelphia: Lippincott-Raven; 1998:511–615 A 64-year-old woman, 6 months after right breast lumpectomy and radiation therapy, has new calcifications adjacent to her lumpectomy site. • Right breast: scar in upper outer quadrant of right breast from previous lumpectomy; no new masses • Left breast: normal exam Calcifications (Fig. 18.9) • Type: pleomorphic/heterogeneous • Distribution: grouped/clustered Fig. 18.9 In the right upper outer quadrant, there are clips associated with architectural distortion from a previous lumpectomy. Adjacent to the clips is a group of new heterogeneous calcifications (circle). (A) Right MLO magnification mammogram. (B) Enlargement of circled calcifications in A. (C) Right CC magnification mammogram. (D) Enlargement of circled calcifications in C. Frequency • 5 MHz Mass (18.10) • Margin: spiculation/architectural distortion • Echogenicity: hypoechoic • Retrotumoral acoustic appearance: severe shadowing, mass completely obscured • Shape: irregular Fig. 18.10 Right longitudinal breast sonogram. The patient’s lumpectomy scar is an irregular, hypoechoic, spiculated abnormality with severe posterior acoustic shadowing. The superficial tissue lines (white and black arrows) exhibit architectural distortion. • Scar • BI-RADS assessment category 4, suspicious abnormality; biopsy should be considered. • Differential diagnosis for etiology of these calcifications is either fat necrosis from lumpectomy or malignancy. • Sonographically, scars are hypoechoic areas with severe acoustic shadowing that are commonly associated with architectural distortion and spiculation. Dershaw DD, Giess CS, McCormick B, et al. Patterns of mammo-graphically detected calcifications after breast-conserving therapy associated with tumor recurrence. Cancer 1997;79(7):1355–1361 Liberman L, Van Zee KJ, Dershaw DD, Morris EA, Abramson AF, Samli B. Mammographic features of local recurrence in women who have undergone breast-conserving therapy for ductal carcinoma in situ. AJR Am J Roentgenol 1997;168(2):489–493
Case 18.1: Skin Powder/Deodorant
Case History
Physical Examination
Mammogram
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 18.2: Fibrocystic Changes
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 18.3: Fibroadenoma
Case History
Physical Examination
Mammogram
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 18.4: Fibroadenoma
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 18.5: Fat Necrosis
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree