Cancer Pain Management in Children
Pesach Shvartzman
In spite of the advancement in the knowledge and skills in treating cancer pain in children, many patients still receive suboptimal treatment. No physician, nurse, technician, or parent likes to see a child in pain. However, we still witness many barriers to treatment. For many parents the words morphine or methadone mean the situation is serious or terminal, we are giving up, addiction, and/or concern that when there will be a need for stronger pain medications it will not be effective. Amongst many medical teams morphine and methadone mean addiction, risk of shortening life, respiratory depression, confusion, tolerance, side effects, and fear of pain medications. Unfortunately, many physicians and nurses do not receive structured training in pain management.
One of the reasons treating children with pain is difficult is that evaluating the pain level in children is complex. As pain is a subjective feeling, children above the age of 5 years will know to report pain on an imaginary scale of 0-10 VAS (visual analogue scale). In children under the age of 5 years, a Faces Pain Scale can be used to report the level of pain. In younger children, evaluation tools that integrate observation of behavior may be used, such as facial expressions, restless legs, level of activity, crying and consolability.
Pain in the child with cancer can be due to the illness itself (e.g., a brain tumor causing increased intracranial pressure), a diagnostic procedure (such as bone marrow aspiration or lumbar puncture), or treatment (surgery, mucositis after chemotherapy, or radiation).
The pathophysiologic classification has important practical implications since for each category a specific treatment is recommended. Neuropathic pain is caused by an injury to the transmission system: peripheral nonmyelinated type C fibers, and type A myelinated nerve fibers, or injury to the spinal cord or the brain. The injury may be a result of the tumor infiltration, chemotherapy, radiation, mechanical reasons (i.e., surgery), or infection (i.e., herpes zoster). Nociceptive pain derives from stimulation of peripheral receptors as in a fracture or bone tumor. Pain can be treated by both pharmacologic and nonpharmacologic methods. At our disposal there are many pain killers: acetaminophen, nonsteroidal anti-inflammatories (NSAIDs), opioids, tramadol, anticonvulsants, and antidepressants.
HOW DO WE CHOOSE WHICH MEDICATION TO GIVE FIRST AND WHEN?
A useful tool to assist in this predicament is the World Health Organization (WHO) ladder. The severity of pain, on a scale of 1-10, determines the type and dose of medication prescribed. For mild pain (1, 2, 3, 4) administer nonopioids, for moderate pain (5, 6, 7)—low dose opioids ± adjuvants, and for severe pain (8, 9, 10)—opioids ± adjuvants. However, like a step ladder, a patient with severe pain is initially prescribed nonopioids, effectiveness is assessed, and if pain management is not achieved, only then the next stage up the ladder is taken.
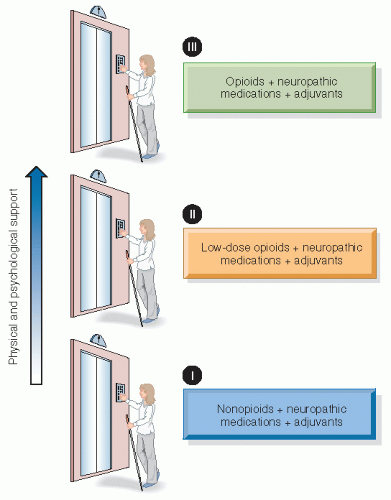
In our latest recommendations, published by the Israeli Cancer Association and the Israeli Medical Association, we recommended the elevator model rather than the WHO ladder. In this model, medications are prescribed in accordance with the patient’s pain level. Thus, a child reporting a pain intensity of 8/10 would receive an opioid rather than an NSAID or acetaminophen, and if a child reports pain intensity of 4/10, an NSAID or acetaminophen would be prescribed (Fig. 23.1).
In each stage, if the patient has neuropathic pain a medication for neuropathic pain should also be prescribed. For
mild pain (1, 2, 3, 4) with a neuropathic component the patient will receive nonopioids and antidepressants, anticonvulsants, steroids, or NMDA antagonist. If the patient suffers from moderate pain (5, 6, 7) with a neuropathic component, he or she will receive low-dose opioids and neuropathic pain medications. For severe pain (8, 9, 10) with a neuropathic component, the patient will receive opioids and neuropathic pain medications (Tables 23.1 and 23.2).
mild pain (1, 2, 3, 4) with a neuropathic component the patient will receive nonopioids and antidepressants, anticonvulsants, steroids, or NMDA antagonist. If the patient suffers from moderate pain (5, 6, 7) with a neuropathic component, he or she will receive low-dose opioids and neuropathic pain medications. For severe pain (8, 9, 10) with a neuropathic component, the patient will receive opioids and neuropathic pain medications (Tables 23.1 and 23.2).
Table 23.1 Opioids Available for Children | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree