High CVD risk
Intermediate CVD risk
Low CVD risk
Estimated 10-year cardiovascular mortality (SCORE > 10%)
SCORE 5–10%
SCORE <5%
Established cardiovascular disease
Two or more risk factors (e.g., nicotine abuse, hypertension, low high-density lipoprotein cholesterol, family history of premature coronary artery disease, and age)
0–1 risk factors
Diabetes mellitus II
Diabetes mellitus type I with microalbuminuria
Markedly elevated single risk factor
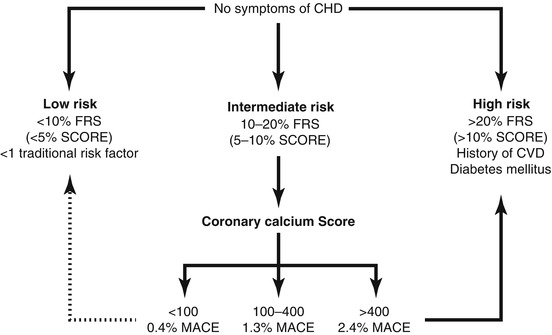
Fig. 4.1
Use of coronary calcium imaging in asymptomatic intermediate-risk individuals. Coronary calcium score can reclassify individuals at intermediate risk of coronary artery disease (10–20% 10-year risk by Framingham Risk Score, FRS) or cardiac death (5–10% 10-year by SCORE) into low, intermediate and high risk (major adverse cardiac events per year). While more intensive preventive measures are warranted in patients reclassified to high risk, there are no recommendations to decrease preventive measures in patients reclassified to low risk. This scheme follows the recommendations by Greenland et al. in the ACCF/AHA 2007 Expert Consensus Document. CHD coronary heart disease, MACE major adverse cardiovascular events
Contrast-enhanced CT angiography is currently not recommended in patients who do not have symptoms. While radiation exposure may become less of a concern with the development of low-dose scan protocols, there is still the need for intravenous injection of potentially harmful contrast media. Coronary CT angiography has the potential to identify patients with severe but noncalcified coronary artery disease, which would be missed by unenhanced CT. Finding severely obstructive disease is rare, and the overall prognosis of asymptomatic patients without detectable coronary calcium is excellent (<1% annual event rate). CT angiography in an asymptomatic Korean population resulted in more coronary interventions, but no increased hard event rate in patients with silent CAD. Whether identification of the small number of patients with significant noncalcified plaque justifies the higher radiation exposure and contrast agent administration is unclear and heavily debated.
4.3 Patients with Stable Chest Discomfort
In Europe exercise electrocardiography remains the most frequently used initial test in patients with suspected coronary artery disease, whereas in the USA single-photon emission computed tomography is more frequently used. Exercise electrocardiography has a high specificity but a low sensitivity, using invasive angiography as a reference (Fig. 4.2). Myocardial perfusion imaging, using single-photon emission computed tomography, positron emission tomography, or magnetic resonance imaging (MRI), is more accurate but also more expensive in comparison to exercise electrocardiography. They are therefore considered secondary diagnostic modalities in the majority of patients (Table 4.2) by the European guidelines. The British NICE guidelines have removed conventional exercise testing and suggest that stress imaging should be the first choice technique in patients with an intermediate pretest likelihood of CAD.
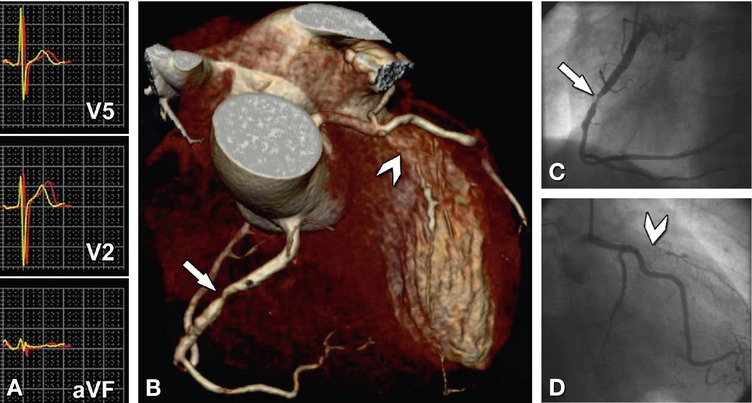
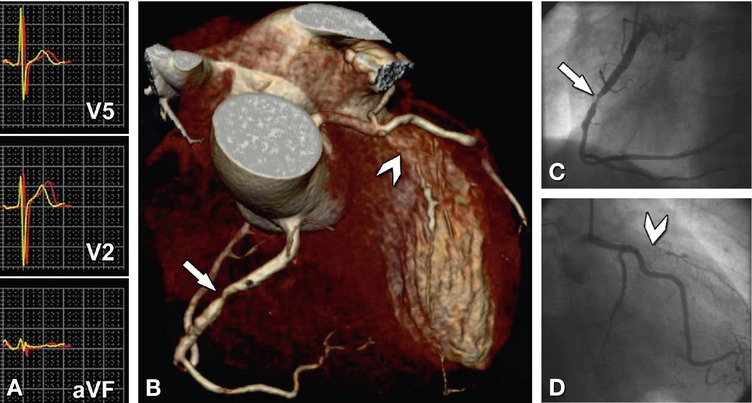
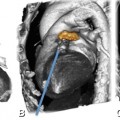
Fig. 4.2
False-negative exercise ECG and true-positive coronary CT angiography. Exercise ECG without significant ECG changes in a 57-year-old patient with stable angina symptoms (Panel A). Severely stenotic right coronary artery (arrow) and occluded left anterior descending coronary artery (arrowhead) on coronary CT angiography (Panel B), confirmed by conventional coronary angiography (Panel C and D)
Table 4.2
Diagnostic accuracy for noninvasive detection of coronary artery disease
Modality | Diagnostic performance | |
|---|---|---|
Sensitivity (%) | Specificity (%) | |
Exercise electrocardiography | 68 | 77 |
Exercise stress echocardiography | 80–85 | 84–86 |
Dobutamine stress echocardiography | 40–100 | 62–100 |
Vasodilator stress echocardiography | 56–92 | 87–100 |
Exercise perfusion scintigraphy | 85–90 | 70–75 |
Vasodilator perfusion scintigraphy | 83–94 | 64–90 |
Dobutamine stress MRI | 83 (79–88) | 86 (81–91) |
Vasodilator perfusion MRI | 91 (88–94) | 81 (77–85) |
CT coronary calcium score (>0 threshold) | >95 | ≈50 |
CT coronary angiography | 100 (98–100) | 89 (85–92) |
Coronary angiography by CT represents an attractive means to noninvasively assess patients with suspected coronary artery disease. The high sensitivity and negative predictive value of coronary CT angiography allow confident visual exclusion of coronary artery disease. Myocardial ischemia is very unlikely in the absence of obstructive coronary artery disease on CT. However, angiographic disease (by CT or catheter angiography) may exist without causing ischemia or symptoms and may not need revascularization. Additionally, stenosis severity cannot be assessed with the same level of accuracy as compared to conventional angiography and will often be overestimated when severe calcification is present. Therefore, coronary CT angiography appears most useful to exclude coronary artery disease in patients with a low-to-intermediate pretest likelihood of disease. Whether CT angiography should be used as the initial test in these patients or after an inconclusive stress test, is still under investigation. Most registries show a very low prevalence of significant obstructive disease in patients with stable chest symptoms without detectable calcium. Therefore, a calcium scan may be an appropriate first step and function as a gatekeeper to further testing, including contrast-enhanced CT angiography. In fact, the British NICE criteria recommend a calcium scan as the first test in patients with chest pain of recent onset and a low pretest likelihood of CAD (10–29%). Only if the calcium scan is 1–400 do they recommend CT angiography. To avoid unnecessary revascularization, we currently prefer to perform stress testing when CT shows moderate obstructive disease to assess hemodynamic significance. As a matter of fact, if coronary CT angiography identifies obstructions of moderate severity at prognostically less important sites, a physician may be more confident in maintaining medical treatment rather than immediately sending the patient for revascularization. Methods to assess functional significance of coronary stenosis by computed tomography are under investigation, which include vasodilator mediated myocardial perfusion imaging and computed simulated fractional flow reserve estimation based on CT angiograms. While statistical modeling of registry data suggests that CT angiography can be cost-effective, prospective data in comparison with other techniques has not yet become available.
In patients with suspected coronary anomalies, CT angiography is the most accurate imaging technique for assessment of the origin, course, and termination of abnormal coronary arteries in relation to surrounding structures (Chap. 17).
In conclusion, cardiac CT (including calcium scanning and CT angiography) has an expanding role in the assessment of suspected coronary artery disease. Whether the technique should be used as the initial test in low-to-intermediate risk patients followed by functional testing in patients with obstructive disease or secondary to functional tests that cannot be performed or produce equivocal results, is yet unresolved. Just as there are patients who are unsuitable to undergo stress testing, CT angiography should only be performed in patients in whom diagnostic image quality can be expected.
4.4 Acute Chest Pain
Cardiac CT may have various advantages over the current diagnostic approach in patients presenting to an emergency department with acute chest pain. Particularly when symptoms have subsided the ECG may be normal, while biomarkers could still take hours to convert in case of an acute coronary syndrome. Stress testing may exclude severe stenosis, but will neglect the presence and extent of coronary atherosclerosis. CT can visualize coronary artery atherosclerosis, identify severe obstructions, detect myocardial hypoperfusion (secondary to myocardial infarction), and allow detection of other potentially life-threatening conditions presenting with acute chest discomfort including aortic dissection, pulmonary emboli, pericardial effusions, and pulmonary disease.
A simple calcium scan may allow exclusion of severe disease in a substantial number of patients and is associated with excellent outcome. However, because of the potentially devastating consequences and the possibly higher incidence of noncalcified disease in patients with an acute presentation, many prefer contrast-enhanced CT angiography instead (Fig. 4.3). CT angiography can exclude an acute coronary syndrome with a high negative predictive value, whereas the positive predictive value appears to be somewhat lower in acute patients. Additionally, the absence of coronary stenosis on CT does not entirely rule out an acute coronary stenosis. A number of randomized trials in low-risk patients with acute chest discomfort can be safely discharged based on CT, reducing hospital stay and overall expenses (Fig. 4.4). The applicability of these results and limited to low risk patients. No clinical benefit was demonstrated and cost-effectiveness will be affected by local logistics and practices of both CT and standard practice, and may change with widespread implementation of high-sensitive troponin measurements. Use of cardiac CT in the emergency ward requires technicians and physicians experienced in coronary CT, a service few clinics can provide 24 by 7.
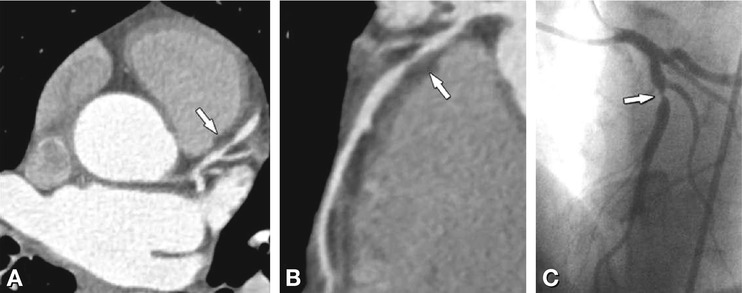
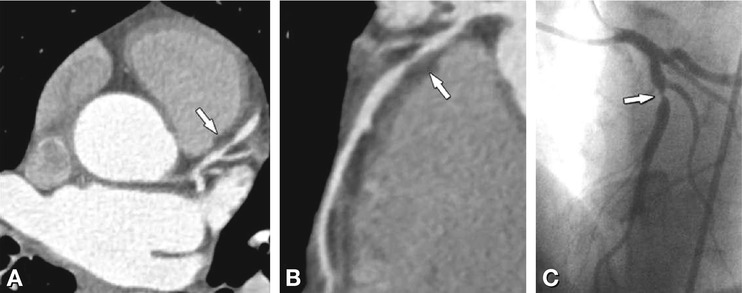
Fig. 4.3
Acute presentation of a 43-year-old man with progressive angina pectoris (without elevated troponin). Coronary CT angiography shows an outwardly (positively) remodeled, noncalcified, stenotic lesion (arrow) in the left anterior descending coronary artery (Panel A, axial image; Panel B, curved multiplanar reformation), confirmed on conventional coronary angiography (Panel C)
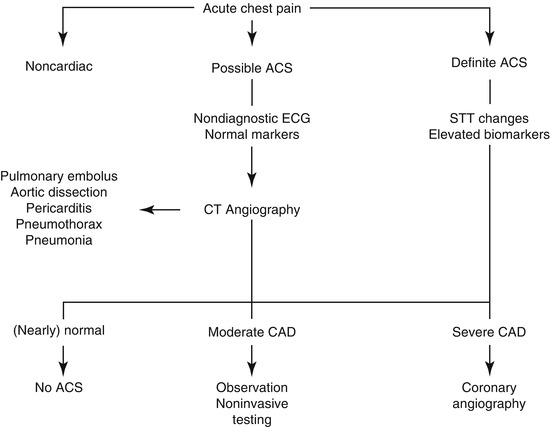
Fig. 4.4
Potential implementation of cardiac CT in patients with a suspected acute coronary syndrome. ACS acute coronary syndrome, CAD coronary artery disease, STT ST trace
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree