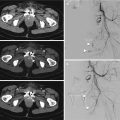
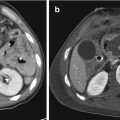
Fig. 10.1
Traumatic inferior cava disconnection. Contrast enhanced MSCT—post-surgical control after 1 day (a) and after 1 week (b, c). In (a) (arrow) is still present a hematoma; in (b, c) the hematoma decreased (arrow)
Similar to the previous conditions, valve injuries, such as leaflet rupture, rapidly lead to a clinical scenario of heart failure (rapidly evolving respiratory insufficiency due to pulmonary edema, pulmonary crackles, and hemodynamic instability) [12].
Septal rupture can cause delayed heart failure. It is important to understand if septal defect (SD) is a preexisting situation or it is caused by trauma. Acquired ventricular SD could be associated with a third heart sound, a loud systolic murmur, and signs of left or right ventricular failure. Finally, commotio cordis is characterized by sudden death following a blunt chest impact in patients without preexisting or traumatic structural heart diseases. Common situations of commotio cordis are those that occur during sport activities [13]. Although the pathophysiology is unclear, the temporal correlation between the trauma and the death keeps the ventricular fibrillation the most likelihood etiopathogenesis [13].
10.2.2 Diagnosis
In multiple trauma, the chest trauma is considered to cause up to 25% of the causes of death. Therefore, chest trauma should always be taken into serious consideration even in the absence of external signs or specific symptoms. The dynamics of the event is also important in the stratification of the risk of damage (impact on steering, airbags, etc.) [14]. Cardiac involvement should be suspected in patients with significant chest injury or polytrauma referring palpitations, ore suffering of arrhythmias, presenting new cardiac murmur, or unexplained tachycardia or hypotension. ECG ST segment might change by mimicking myocardial ischemia after cardiac trauma. The most common conduction abnormalities include atrial fibrillation, bundle branch block (mostly right), unexplained sinus tachycardia, and single or multiple ventricular ectopic beats. Cardiac biomarkers (i.e., troponin, CPK-MB) are useful tools for the screening of blunt cardiac injury. If cardiac biomarkers and ECG are within normal limits and there are no arrhythmias, blunt cardiac injury can be excluded. Rarely, chest trauma can cause a coronary artery damage causing myocardial infarction (Fig. 10.2). In addition, in approximately 20% of patients with penetrating lesions of the heart, and in patients with non-penetrating trauma, a delayed form of pericarditis, similar in character and natural history to those occurring after AMI, can occur [15]. In these cases, the medical history before chest trauma is of major importance in diagnosing the cardiac disease.


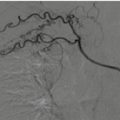
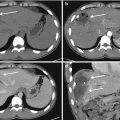
Fig. 10.2
Post-traumatic right coronary occlusion. (a) VRT reconstruction and (b) MIP reconstruction
Nuclear medicine. Until now, the role of nuclear medicine (including PET using 18F-2-fluoro-2-deoxy-D-glucose) has not well established in the setting of blunt thoracic trauma [16]. In selected cases, the same nuclear medicine techniques that are successfully used to diagnose myocardial ischemia have been attempted in evaluating trauma patients.
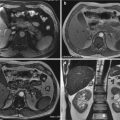
Angiography. Angiography, although not specifically indicated, can visualize or suspect some of the mechanical consequences of a chest trauma such as pericardial effusion, ventricular septal defects (VSDs), fistulae, and ventricular or aortic aneurysms [17].
Echocardiography. Ultrasound techniques, in the setting of trauma, has gained wide acceptance in the form of the Focused Assessment with Sonography for Trauma (FAST), in which echography is used to detect free fluid in the pericardium [16].
Echocardiography usually performed during the early phases of resuscitation can show wall motion abnormalities, pericardial fluid, or chamber or valvular rupture.
In addition, regurgitant valvular lesions, aortic-atrial or ventricular fistulae, and VSDs can produce left ventricular dilatation or hypercontractility at the echocardiographic examination. Valvular regurgitation and shunt flow can be detected and quantified by means of the Doppler evaluation. Myocardial contusion and MI result in regional hypokinesis or akinesis [2].
Chest X-ray (CXR): CXR continues to be an appropriate primary screening modality in thoracic trauma assessment, as noted in “ACR Appropriateness Criteria Blunt Chest Trauma” [16]. Antero-Posterior (AP) chest radiography is essential to quickly exclude rough displacement of lines and tubes that could be difficult to detect in the setting of polytrauma. Although AP chest radiographs are often of pore quality in case of polytrauma, they still are considered essentials. Signs include cardiomegaly secondary to hemopericardium or pericardial effusion; signs of left ventricular failure (vascular redistribution, interstitial or alveolar edema, pleural effusion) secondary to myocardial contusion, ventricular aneurysm, valvular disruption, intracardiac fistula, or VSD; and mediastinal widening secondary to aortic disruption and tracheal deviation. In addition, chest X-ray can easily investigate the occurrence of further findings, such as fractured ribs, hemo/pneumothorax, or pulmonary infiltrates in patients with trauma. However, it is widely known that AP chest radiography has lower accuracy for blunt traumatic injuries than CT and the use of this as the only diagnosis tool in trauma does not seem appropriate [16].
CT how and when. CT represents a gold standard modality in polytrauma. Contrast enhanced chest CT is known as a reliable modality for the investigation of thoracic trauma [16]. A cardiac injury can be present in patients with high kinetic energy trauma associated with sternum or rib fractures, lung contusions, pneumothorax, and vascular lesions. Although CT clearly allows detailed evaluations of trauma patients, the use of ionizing radiation have raised some safety concerns related to the extensive use of CT. In fact, ionizing radiation derived from medical use has increased, and the use of CT should be limited to the necessity [18]. There are conflicting data on whether routine chest CT is necessary in the setting of blunt trauma so far.
Depending on CT available apparatus, a collimation of 0.6 mm is recommended. The radiation dose should be kept as lower as possible, especially by applying dose reduction software wherever available. Nevertheless, the use of 120 KV and 300 mA is currently considered appropriate. Intravenous administration of contrast medium is imperative for imaging polytrauma patients. Usually, pre- and post-contrast imaging is performed in arterial phase (as not to miss any injury of the major vessels) and in venous phase. In case of suspected bleeding, a delayed acquisition at 5 min is highly recommended, taking into account patient’s hemodynamic stability. Optimal opacification may be obtained with injection of 100–140 mL of iodinated contrast medium (preferable high concentration) at a flow rate of 3–4 mL/s followed by a saline flush injection. Importantly, pericardial effusion must be considered a red flag sign (Fig. 10.3). ECG gating for thoracic trauma is quite controversial as it provides a high diagnostic quality for vascular structures (aortic, coronary, or cardiac injury) but may reduce the quality of bone and lung injury. Given the fact that retrospective ECG gating compared with prospective ECG gating increases the radiation dose significantly, and that polytrauma patients may have an unstable heart rate higher than 80 beats/min, one should weigh the use of ECG gating carefully so as not to lose valuable time [14]. When a cardiac trauma or great vessels heart connection injury are suspected in stable patients, a gated CT examination could be useful after the initial CT as extending. A gated cardiac CT can be useful also in a suspect of iatrogenic cardiac trauma as post-surgery or vascular procedures (Fig. 10.4).