Noninvasive imaging of the carotid and vertebral arteries is achieved with duplex ultrasonography, computed tomography angiography (CTA), and magnetic resonance angiography (MRA). This chapter focuses on pearls and pitfalls of these modalities in the evaluation of steno-occlusive disease of the carotid and vertebral arteries.
Ultrasonography
Justification
Carotid artery duplex ultrasonography is a noninvasive, affordable screening test that is devoid of radiation for patients at high risk for severe carotid disease, and hence at high risk for acute stroke. Duplex ultrasonography of the internal carotid arteries (ICAs) is indicated in several clinical settings, including patients who have experienced transient ischemic attacks, patients with ischemic stroke, and asymptomatic patients who possess cervical carotid bruits, and as a preoperative evaluation before coronary artery bypass graft surgery or aortic valve replacement.
Although carotid screening is not recommended for all coronary artery bypass graft surgery or aortic valve replacement candidates, patients over the age of 60 years or those presenting with a minimum of two cardiovascular risk factors, such as elevated cholesterol levels or hypertension, should undergo carotid evaluation to reduce the risk for perioperative stroke. Noninvasive carotid imaging is also important for those patients who have experienced transient ischemic attacks because of the significantly increased risk for stroke in the months following a transient ischemic attack. Approximately 20% to 30% of embolic strokes originate from the carotid arteries, and it is recommended that patients suffering from acute stroke also undergo carotid artery duplex ultrasonography to serve as a baseline for future evaluations. Although a carotid bruit in itself is neither a specific nor sensitive indication of carotid disease, it has been documented that up to one third of patients with bruits do have severe ICA stenosis. Therefore noninvasive duplex ultrasonography to assess the degree of carotid stenosis is important to determine those patients who will benefit the most from carotid artery revascularization.
Standard Evaluation
A standard carotid duplex ultrasonography consists of a bilateral examination of the common carotid arteries (CCAs), ICAs, external carotid arteries (ECAs), and the vertebral arteries (VAs).
Transverse grayscale images are typically obtained at the carotid artery bulb and carotid artery bifurcation, and in the case of any significant lesions, both grayscale images and color Doppler images are obtained in the transverse plane. Images in the longitudinal plane are obtained throughout the course of the CCA and ICA, ECA, and VA. Grayscale imaging is conducted separately from the spectral Doppler evaluation. Spectral Doppler waveforms are obtained with a defined technique; the waveforms should be obtained by placing the cursor in the longitudinal view of the artery with the cursor placed in the center of the stream of flow, the “flow jet.” The recommended Doppler angle is between 40 and 60 degrees. Nine standardized sites are imaged: the proximal, middle, and distal CCA; the proximal, middle, and distal ICA; the proximal ECA; and the proximal and middle VA. According to the American College of Radiology and American Institute of Ultrasound in Medicine, blood-flow velocity measurements should be recorded at a minimum of one site in the CCA, ECA, and VA, and two sites in the ICA. If significant stenoses are detected, spectra should be sampled within and distal to each stenosis, with the highest velocity determined and recorded.
Normal Waveform Characteristics
Each vessel has a characteristic normal waveform pattern based on the vascular bed distal to the artery. The ICA demonstrates a low-resistance waveform with continuous forward flow throughout diastole; in contrast, the ECA displays a high-resistance waveform with a sharp systolic upstroke and decreased diastolic flow. Waveforms in the CCA are hybrids of the ICA and ECA waveforms, generally displaying a sharp systolic upstroke and continuous flow throughout the diastole. The VA in a healthy patient demonstrates a low-resistance waveform with continuous forward flow in the diastole. Changes in the waveforms of the VA are further discussed later.
Grayscale and color flow imaging and spectral Doppler evaluation provide the necessary tools to determine the severity of carotid stenosis. Multiple studies have defined significant carotid stenosis as greater than 70%. We use the guidelines listed in Table 43-1 at our laboratory to determine the degree of carotid artery stenosis.
| Degree of Stenosis | Peak Systolic Velocity (cm/sec) | Approximate Degree of Stenosis (%) | Luminal Diameter (mm) | Other Indirect Signs |
|---|---|---|---|---|
| Normal limits | <150 | <50 | >3 | |
| Mild | 150-200 | 50- 60 | 2.5-3 | |
| Moderate | 200-300 | 60-70 | 2-2.5 | |
| Severe | 300-400 | 70-80 | 1-2 | Reversal flow ipsilateral ACA (TCD) |
| Critical | >400 | 80-90 | 0.7-1 | Reversal flow ophthalmic artery (TCD) |
| Falling off | >90 | <0.7 | MRA shows absent distal ICA signal (slow flow versus occlusion); consider CTA |
Postoperative Evaluation
For those patients who have undergone carotid endarterectomy or stenting, subsequent follow-up should also be performed to assess for restenosis, occlusion, and development of intimal hyperplasia. Intimal hyperplasia is probably the most frequent complication after surgery and results secondary to operative trauma, usually peaking at 3 months post surgery. It generally does not progress after the first year and is characterized by scar tissue or redundant granulation. Intimal hyperplasia with smooth muscle cell and matrix accumulation is the prominent feature in all these situations. Primary carotid atheromatous disease is associated with intense cell proliferation and cell death without evidence of inflammation.
The evaluation of the revascularized carotid artery should be focused on the expected areas of surgical incision and clamping. For instance, the evaluation of the postendarterectomy carotid artery should be concentrated on the near wall, which is usually the area of carotid artery incision, and special attention should be paid to the distal portion of the ICA, where a clamp is usually placed and intraoperative inspection is often limited.
Principal Indications for Sequential Carotid Artery Studies
Although CTA and MRA are the tests of choice in the workup of acute ischemic events, radiation and cost limit these techniques for sequential follow-up of carotid artery lesions. Ultrasonography may be ideal for long-term follow-up of patients at high risk for atheromatous disease of the carotid arteries and postsurgical complications.
Sequential carotid artery imaging is suggested for the following:
- •
To assess for progression of carotid artery stenosis caused by atheromatous disease
- •
To monitor the revascularized carotid artery for evidence of intimal hyperplasia or recurrent atheromatous disease
- •
To evaluate dissected carotid arteries for evidence of progression or resolution of occlusive process
Carotid Artery Duplex Ultrasonography Pitfalls
Problems occurring with carotid artery duplex ultrasonography may be divided into three general groups: technical pitfalls, limitations of the technology, and interpretation pitfalls.
Technical Pitfalls
Technical pitfalls include equipment difficulties such as choosing the correct probe according to patient body habitus and selecting appropriate imaging parameters (pulse repetition frequency [PRF], color gain, filters, speckle-reduction software) for the highest diagnostic image quality.
Appropriate Transducer
As the Doppler beam propagates through tissues, its intensity decreases with increasing penetration in a process referred to as attenuation. Although attenuation is quite high for muscle and skin, in fluid-filled structures such as the carotid arteries, attenuation is very low. Higher frequencies in duplex ultrasonography typically offer improved image resolution. A 7- to 9-MHz probe is the most commonly used and is appropriate for most patients; however, in a patient with a large body habitus or in a patient with deep vessels, a 5-MHz probe will allow for greater penetration. In a patient with very superficial vessels, a higher frequency transducer such as a 10- or 12-MHz probe may be more appropriate.
Angle of Insonation
The angle of insonation must be considered when performing and interpreting carotid ultrasonography. If the correct angle is used, the sampling cursor will be parallel to the vessel wall. The recommended Doppler angle is between 40 and 60 degrees; an angle that is too low or too high results in inaccurate insonated peak systolic velocities. Tortuous vessels can be especially difficult to insonate; keeping the angle between 40 and 60 degrees may at times be impossible. In cases in which the vessel “dives deeply,” using an angle of zero degrees may be the most appropriate. Because of the inherent difficulty in placing the Doppler probe, velocities are often overestimated secondary to vessel tortuosity. When interpreting the degree of stenosis in a tortuous vessel, it is important to note that although peak systolic velocities may be consistent with stenosis, velocities may also be simply overestimated because of the limitations of the Doppler angle. As always, the best angle to use is one in which the cursor is parallel to the vessel wall and located in the middle of the flow jet.
Luminal Echo (Reverberation Artifact)
The reverberation artifact results from the differences in impedances of two different objects. In the context of the carotid artery, these two materials are the near wall of the carotid artery and a small carotid plaque or a calcified nodule within the soft tissue of the neck. When the transducer scans to the left or right of the high-impedance object, in this case the plaque or calcified nodule, the normal image of the top surface of this object is displayed over the image of the object below, in this case the carotid artery wall. If the impedance differences are of the proper magnitude when the transducer is above the object, the ultrasound pulse will reflect back and forth several times between the top and bottom surfaces. This gives rise to a series of echoes, equally spaced in dimension, received by the transducer. This appears on the grayscale images as a series of lines within the carotid lumen that may be mistaken for a dissection with an intraluminal flap.
The correction for this artifact is usually dynamic and is easily discovered; when changes in the angle of insonation are performed and the luminal echo disappears or changes in location, this is consistent with reverberation artifact.
Mirror Image Artifact
The mirror image artifact is usually present when the ultrasonic beam of insonation intersects within the oblique surface and the echoes from this oblique surface do not return to the transducer. The time elapsed for these echoes from the oblique structure is longer than for those that are perpendicular; however, they may be interpreted as deeper given the time difference. The resulting artifact is an image that displays a mirror image at an artifactual depth compared to the true surface. The simplest correction for this artifact is again dynamic imaging; mirror image artifact is easily discovered when changes to the angle of insonation are performed.
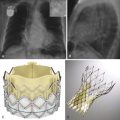
Excessive Color Gain
Excessive color gain results in overestimation of the residual lumen given that the increased color gain surpasses and covers the boundaries of the stenosis and vessel ( Fig. 43-1 ). This prevents accurate assessment of plaque composition and thickness. Appropriate color gain is especially important in the imaging of a carotid dissection involving the intima, when excessive color gain artifact may overshadow an intimal flap. Narrowing of the vessel lumen diameter should be evaluated based on the peak systolic velocities and not solely on color flow or grayscale imaging.

Appropriate Pulse Repetition Frequency
In the case of a carotid pseudo-occlusion (hairline lumen), it is especially important that an appropriate PRF is used in the insonation of the vessel. In a typical hairline lumen, pseudonormalization will be observed, and in such a “slow-flow” situation, a PRF between 10 and 40 is typically most appropriate. A PRF below 10 will result in excess color artifact ( Fig. 43-2 ); this could potentially resemble color flow within the vessel, which could be misconstrued as normal carotid flow. A PRF above 40 will likely diminish all low-level flow, and images could be misinterpreted as true arterial occlusion.

Limitations of the Technology
Limitations of the technology include physical limitations such as the inability to insonate the CCA origin or the ICA at the skull base, as well as flow limitations, as seen during the imaging of ICA tandem lesions.
B-Mode (Grayscale) Ultrasonography
B-mode alone is not a reliable measure of the degree of stenosis in the carotid arteries. Although B-mode is useful in determining plaque location, composition, and length, dense hypoechoic plaque is not well identified on B-mode alone ( Figs. 43-3 and 43-4 ); the use of color flow is necessary to demonstrate hemodynamic significance. Peak systolic velocities should be used to determine the degree of stenosis.


Heavily Calcified Plaque
Heavily calcified plaque impedes Doppler measurements of the underlying vessel. This limitation is of great importance when a calcified plaque extends greater than 1 cm down the course of the vessel; such lesions cannot be thoroughly imaged using duplex ultrasonography, and distal Doppler measurements are not reliable to infer the degree of proximal stenosis. MRA and dual energy CTA with calcium removal are useful to evaluate these segments.
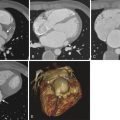
Tandem Lesions
Tandem lesions in the carotid arteries are defined as two separate stenoses occurring at least 3 cm apart, resulting in a severe stenosis of the vessel. The second lesion, located downstream from the insonated lesion, causes dampening of the peak systolic velocity between the two lesions. This phenomenon is secondary to increased pulse pressure between the two lesions, which eliminates the pressure gradient necessary to increase velocities immediately distal to the initial lesion. In this situation, although B-mode imaging is consistent with a severe stenosis, velocities and spectral configuration of flow of the poststenotic segment (between the two lesions) remain within normal or slightly abnormal limits ( Fig. 43-5 ) . It is the stenosis with the greatest narrowing that determines the hemodynamic compromise. When tandem lesions are suspected because of the discrepancy between the B-mode images and Doppler flow, CTA or contrast-enhanced MRA or conventional angiography of the neck should be used for a definitive diagnosis.

Anatomic Limitations
Carotid duplex ultrasonography is limited in its ability to evaluate the entire ICA. The distal ICA, defined as the ICA at the skull base, cannot be imaged with duplex ultrasonography because of anatomic limitation. The presence or absence of stenosis in this vessel segment must be determined by MRA or CTA. However, changes in the proximal ICA waveforms can provide clues about the presence of stenosis distal to the area of insonation in this specific scenario. High-resistance waveforms demonstrating sharp systolic upstrokes are suggestive of a more distal stenosis of the ICA, likely in the intracranial portion, when not visualized in the area of sampling ( Fig. 43-6 ).

Alternatively, delayed systolic upstrokes and low peak systolic velocities noted throughout the course of the ICA are suggestive of more proximal stenosis at the ICA origin, in the bulb, or in the more proximal CCA. Similarly, the CCA origin cannot be insonated secondary to anatomic limitations; however, changes in the CCA waveform are useful in determining the presence of more proximal stenosis. Again, delayed systolic upstrokes and low peak systolic velocities are suggestive of a more proximal stenosis, either of the aorta or at the CCA origin, whereas highly resistant waveforms with sharp systolic upstrokes are suggestive of severe distal stenosis within the ICA. Tandem lesions could also be considered an anatomic limitation for ultrasound coverage.
Interpretation Pitfalls
Internal Carotid Artery Versus External Carotid Artery
During interpretation it is essential that the ICA and ECA are correctly identified. The worst-case scenario is that the two vessels are confused, and a patient with severe stenosis is recommended for carotid revascularization, only to find out that the diseased vessel is an ECA. There are four anatomic and waveform patterns that help distinguish the ECA from the ICA. It is important that during the course of carotid duplex ultrasonography the sonographer uses a temporal tap to prove that the vessel being insonated is an ECA; an ECA will respond to a temporal tap, whereas the ICA will not. In addition, the ECA may have visible branches and will most likely be located medial to the ICA. Lastly, as previously discussed, the ECA will demonstrate high-resistance waveforms, whereas the ICA demonstrates low-resistant waveforms.
Pseudo-Occlusion Versus Complete Occlusion of the Internal Carotid Artery
Vessel occlusion is indicated by lack of Doppler shift within the vessel lumen; however, very slow flow may not be detected during routine examination. Routine duplex ultrasonography may be insensitive to such low velocities. Carotid duplex ultrasonography displays a sensitivity of 80% to 90% for detecting hairline lumina when correct parameters are followed ( Fig. 43-7 ); technique should be optimized by placing the Doppler signal in the ghost vessel while increasing color gain to the maximum level and decreasing filters and PRF. When there is clinical suspicion for ICA or CCA occlusion with duplex ultrasonography, CTA may be required for a definitive diagnosis, although conventional catheter angiography remains the standard for accurately determining between true occlusion and pseudo-occlusion/residual hairline lumen.