Myocardial perfusion imaging (MPI), using single photon emission computed tomography (SPECT) or positron emission tomography (PET) radionuclide techniques, is a commonly performed diagnostic imaging test to detect coronary artery disease (CAD) and determine risk of future events in patients with suspected or known CAD. The diagnostic and prognostic value of normal and abnormal MPI tests has been supported by many studies in the literature. This chapter explores the evaluation of patients with preclinical CAD, established chronic CAD, and acute chest pain evaluation, as well as postmyocardial infarction (MI) risk stratification and evaluation of myocardial viability.
Preclinical Coronary Atherosclerosis
Key Questions
- 1.
Does a role exist for radionuclide testing in asymptomatic patients for coronary atherosclerosis?
- 2.
What are the modalities available for detection of preclinical coronary atherosclerosis?
Although robust medical literature supports the use of stress imaging for evaluation of symptomatic patients with known or suspected CAD, literature supporting testing in asymptomatic patients is not widely available. Various tests are available for the detection of subclinical atherosclerosis in asymptomatic patients with coronary risk factors ( Box 29-1 ).
Treadmill exercise test
Single photon emission computed tomography or positron emission tomography myocardial perfusion imaging
Computed tomography coronary calcium scoring
Computed tomography coronary angiography
Endothelial or microvascular dysfunction
Carotid ultrasound
Ankle brachial index
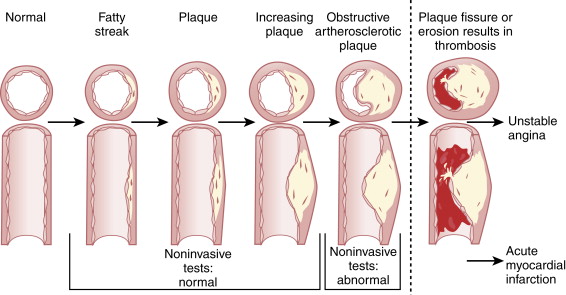
Practical Aspects
In patients with coronary risk factors, coronary atherosclerosis progresses gradually over the course of several decades. At the early stages, coronary risk factors can result in endothelial dysfunction with or without epicardial coronary artery narrowing. Subsequently, atherosclerosis can become evident initially as vessel wall abnormalities with preserved luminal diameter. With further progression of atherosclerosis, the outward remodeling process reaches a limit, and luminal encroachment ensues. Most results of tests of ischemia are positive at a stage in which atherosclerosis causes luminal narrowing and myocardial ischemia ( Fig. 29-1 ). However, several studies have shown that nonobstructive coronary artery lesions can indeed lead to MI and associated complications from rupture of vulnerable albeit nonobstructive CAD. Thus, interest in identifying nonobstructive coronary plaque with imaging techniques is growing, but more evidence is needed to understand whether the identification of nonobstructive CAD in asymptomatic individuals is warranted. Although the idea is not without controversy, selected subsets of asymptomatic subjects may be considered appropriate for nuclear perfusion imaging, such as individuals with high coronary heart disease risk (Adult Treatment Panel III [ATP III] risk criteria) or high CAD risk with an Agatston score (coronary calcium score [CCS]) of 100 to 400 or persons with an Agatston score higher than 400.
Radionuclide imaging is widely used in research applications as a tool to identify preclinical atherosclerosis in asymptomatic individuals. Using quantitative PET, absolute myocardial blood flow can be quantified at rest and during peak stress. The coronary flow reserve (CFR; a unitless number) is computed as the ratio of hyperemic myocardial blood flow (after stress) to resting myocardial blood flow. Quantification of myocardial blood flow is better with radiotracers that are extracted linearly in relation to flow. Oxygen-15 (O-15) water is an ideal tracer for quantification of myocardial blood flow. Quantification of absolute myocardial blood flow is well validated with nitrogen-13 (N-13) ammonia, O-15 water, and rubidium-82 (Rb-82).
Abnormalities in myocardial blood flow have been reported in patients with coronary risk factors but without overt cardiovascular disease. The finding of abnormal CFR is the earliest abnormality associated with CAD and is an integrated parameter of endothelial function and endothelium-independent vascular smooth muscle relaxation. Changes in regional myocardial blood flow may also result from loss of myocytes, fibrosis, scar tissue formation, or high-grade stenosis of the epicardial coronary vessel. Measurement of flow responses to physiologic or pharmacologic challenges is done by PET and can be used to identify functional alterations of preclinical coronary atherosclerosis. Abnormal vasodilator response and reduced flow have been found in asymptomatic patients who are at high risk of CAD, with significant correlation between impairment of CFR and severity of lipid profile. Well-controlled studies of patients with isolated risk factors, such as diabetes, hypertension, smoking, postmenopausal state, and a family history of premature coronary atherosclerosis have been shown to demonstrate abnormalities in CFR in response to vasodilator stress agents (predominantly endothelium-independent flow abnormalities) or cold pressor testing (endothelium-dependent mechanisms). Furthermore, in one study, CFR was inversely related to the Framingham risk score (measuring a composite of risk factor burden), and patients with the highest tertile of Framingham risk score demonstrated the lowest CFR. Noninvasively estimated CFR measured using rest and vasodilator PET is also a very useful tool in assessing response to therapy after aggressive treatment of coronary risk factors.
Acute Coronary Syndromes
Key Questions
- 1.
In which groups of patients with acute chest pain can MPI be used for diagnosis?
- 2.
What are the benefits of MPI testing beyond diagnosing CAD in patients with suspected or known acute coronary syndrome (ACS)?
Radionuclide MPI can be used in patients with acute chest pain and suspected ACS (low to intermediate risk), as well as for risk stratification and ischemia detection in a stable patient following a definite ACS diagnosis. For patients with acute chest pain and suspected ACS (low to intermediate risk), the role of radionuclide MPI is to provide diagnostic and risk stratification information to direct management strategies.
In patients with acute and ongoing chest pain at rest, MPI may be performed using technetium-99m (Tc-99m) tracer injection during or soon after resolution of chest pain. Because of the minimal redistribution, the images reflect myocardial blood flow at the time of injection. This algorithm has been associated with a high negative predictive value for ruling out MI and was also useful for triage of patients presenting to the emergency department. An MPI-guided strategy was associated with reductions in unnecessary admission of patients, lower costs, and shorter lengths of stay. More recently, imaging of ischemic memory has been considered in patients with acute chest pain. Dilsizian et al demonstrated that using iodine-123 (I-123)–labeled 15-( p -iodo-phenyl)-3-R s-methylpentadecanoic acid (BMIPP), defects in fatty acid metabolism could be identified as long as 24 hours after an ischemic episode. More recently, BMIPP was used in the evaluation of patients with acute chest pain in the emergency department. The study demonstrated that in patients who presented to the emergency department with acute chest pain, compared with clinical variables alone, the addition of BMIPP SPECT scan was able to increase the sensitivity (from 43% to 81%) of diagnosing ACS, with higher negative (62% to 83%) and positive (41% to 58%) predictive values.
In patients with recent definite ACS (>48 hours and <3months), MPI may be used for risk stratification and management. The absence of reversible defects identifies a low-risk cohort, whereas the presence of reversible defects is a predictor of cardiac events for which coronary intervention may alter outcome. The Adenosine Sestamibi Post Infarction Evaluation (INSPIRE) trial was a large multicenter prospective randomized study that enrolled stable patients with ST-segment elevation MI or non–ST-segment elevation MI that used adenosine Tc-99m sestamibi SPECT as an initial noninvasive method for risk assessment and guidance for subsequent therapy. Expedited imaging was performed early (between 2 and 4 days from hospital admission), with no reported adverse events in these patients. The results of INSPIRE demonstrated that early SPECT MPI testing was able to stratify patients reliably into low-, intermediate-, and high-risk groups. Event rates at 1 year were lowest in patients with the smallest perfusion defects, but the event rates progressively increased when the defect size exceeded 20%. The rates of total cardiac events or death and reinfarction significantly increased within each INSPIRE risk group from low (5.4%, 1.8%), to intermediate (14%, 9.2%), to high (18.6%, 11.6%) ( P < .01). The perfusion results significantly improved risk stratification beyond that provided by clinical and ejection fraction (EF) variables.
Practical Aspects
Patients With Suspected Acute Coronary Syndrome
- ▪
Patients at low to intermediate risk of ACS who are medically stable can be risk stratified by stress MPI, whereas patients with high-risk clinical characteristics in the setting of unstable angina or non–ST-segment elevation MI are recommended to undergo an early invasive strategy with cardiac catheterization. Patients with indeterminate clinical presentations are candidates for chest pain imaging with rest MPI.
- ▪
These subjects should be injected with radiotracer as soon as possible after chest pain resolution and preferably during chest pain.
- ▪
In this context, attenuation-corrected MPI can provide incremental value. Tc-99m tetrofosmin does not need preparation of the kit and may be better suited for this application. Thallium-201 (Tl-201) offers the advantage of having tracer available for use when needed (because of its 73-hour half-life), but it may be fraught with difficulties related to attenuation artifacts.
- ▪
The presence of a perfusion defect on a chest pain myocardial perfusion study does not differentiate between an earlier MI and a new perfusion defect from acute ischemia. Hence, patients with an earlier MI or Q waves on the electrocardiogram (ECG) are not optimal candidates for chest pain radionuclide study.
- ▪
Stress MPI in low- to intermediate-risk patients without infarct or ischemia in the presence of normal left ventricular (LV) function are at low risk of adverse outcome and can be managed conservatively, whereas patients found to have substantial inducible ischemia may be selected for cardiac catheterization.
Patients With Recently Diagnosed Acute Coronary Syndrome
- ▪
MPI may be used in the triage of patients who suffered unstable angina or an acute MI before hospital discharge; rest and vasodilator MPI may be considered for the risk stratification of patients without earlier coronary angiography or with coronary angiography but with incomplete coronary revascularization.
- ▪
In addition, sometimes viability assessment with SPECT or PET is performed in some of these patients (e.g., with late clinical presentation of ST-segment elevation MI) before consideration of coronary revascularization.
- ▪
Typically, because exercise increases myocardial oxygen demand, treadmill exercise testing is performed using a submaximal modified Bruce protocol (see Chapter 5 ). In contrast, vasodilator pharmacologic stress with adenosine or dipyridamole induces coronary hyperemia with minimal increase in oxygen demand. Hence, in the immediate post-MI phase, rest and vasodilator MPI is ideally suited for risk stratification and evaluation of ischemic burden even in patients who are able to exercise. Vasodilator stress testing has been demonstrated to be safe as early as 48 hours after an uncomplicated MI.
Chronic Coronary Artery Disease
Key Questions
- 1.
What is the diagnostic accuracy of radionuclide MPI?
- 2.
What is the prognostic value of radionuclide MPI?
- 3.
Is radionuclide MPI cost effective?
Diagnostic Accuracy, Sensitivity, and Specificity of Single Photon Emission Computed Tomography and Positron Emission Tomography Myocardial Perfusion Imaging
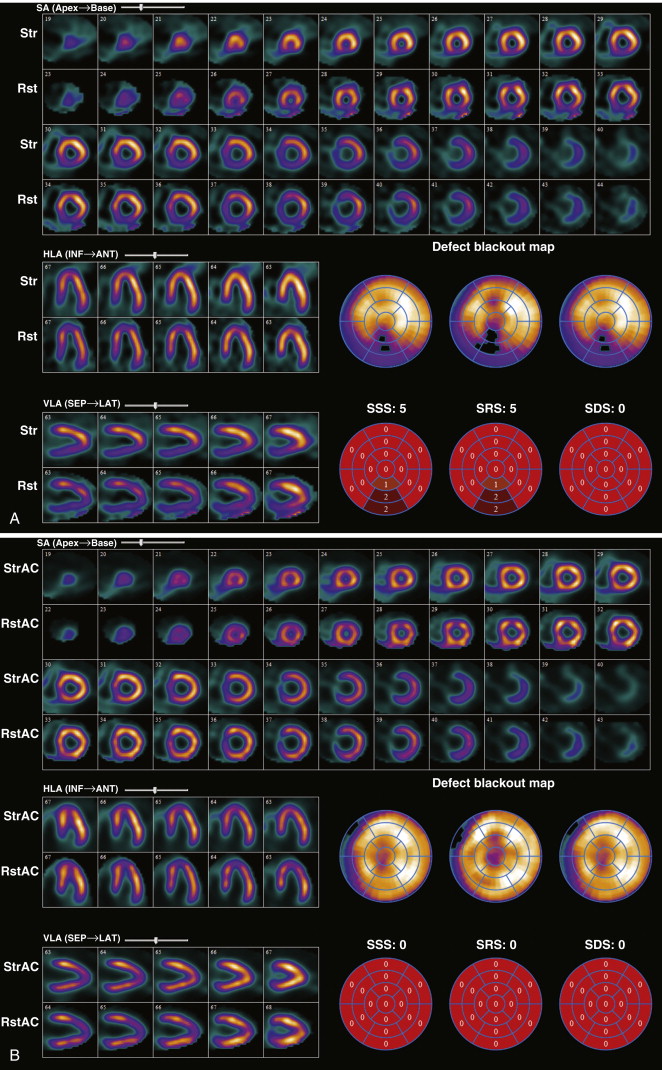
Extensive literature evaluating the sensitivity and specificity of SPECT MPI for detecting obstructive CAD has been published over the years. Pooled analysis of patients with known or suspected CAD demonstrated mean sensitivity and specificity of 87% and 73%, respectively, of exercise myocardial SPECT for detecting more than 50% stenosis. SPECT MPI provides incremental diagnostic value over exercise ECG testing in various patient cohorts. In patients with interpretable ECGs, the Duke treadmill score is able to separate patients into low-, intermediate-, and high-risk groups for future cardiac events. Within each of these Duke treadmill score risk categories, SPECT MPI is able to risk stratify patients further based on summed stress score (SSS) categories. Patients with low- and high-risk Duke treadmill scores may not require nuclear testing because the former group was found to have an extremely low event rate (0.9%), whereas the latter group usually proceeded with cardiac catheterization. In contrast, patients in the larger intermediate-risk category who had a cardiac event rate of 2.5% could be further stratified based on SSS. Those who had normal scans had an event rate of 0.4%, whereas those who had an SSS of 4 to 8 and an SSS of more than 8 had cardiac event rates of 6.4% and 8.9%, respectively.
The literature relating to the diagnostic value of PET MPI is more limited. One study directly comparing the diagnostic accuracy of Rb-82 myocardial perfusion PET and Tl-201 or Tc-99m SPECT showed higher sensitivity with PET than with SPECT (93% versus 76%) and similar specificity (78% versus 80%). However, Stewart et al observed a higher specificity for PET than with SPECT (83% versus 53%, respectively) without significant differences in sensitivity (86% versus 84%, respectively). The overall diagnostic accuracy is also higher for PET than for SPECT using either a 50% or a 70% angiographic threshold (87% versus 71% with a 50% threshold and 89% versus 79% with a 70% threshold), primarily driven by higher specificity. The average positive and negative predictive values of PET MPI for the diagnosis of obstructive CAD are 94% (range, 80% to 100%) and 73% (range, 36% to 100%), respectively.
Attenuation Artifacts Limit the Diagnostic Accuracy of Single Photon Emission Computed Tomography Myocardial Perfusion Imaging
Emitted photons undergo attenuation (absorption or deflection by soft tissues) when they traverse various soft tissue structures (muscle, adipose tissue, bone, breast, and diaphragm) before they reach the photo detectors of the gamma camera. This process of photon attenuation may result in lower sensitivity and specificity for the detection of CAD. Strategies to address attenuation include measurement and correction of soft tissue densities by using transmission scanning by external radioactive sources or cardiac computed tomography (CT). Attenuation correction improves the count uniformity of the image and helps distinguish attenuation artifacts from real defects. In stress-only imaging, if the stress images are normal, attenuation correction offers the possibility to skip the rest imaging and hence reduces time, cost, and radiation dose to the patient. In addition, quantitative estimation of myocardial blood flow in milliliters per gram per minute can be performed because accurate attenuation correction allows for precise measurements of absolute radiotracer concentration in the myocardium.
The disadvantages of using external radionuclide source transmission scans include additional radiation exposure (albeit small) associated with transmission scans that take longer to acquire and degradation of the radionuclide source over time that can diminish image quality. Conversely, CT attenuation correction is rapid (takes a few seconds) and of excellent quality, but it is also associated with additional radiation exposure (albeit small) and is more prone to misregistration with the emission images (as discussed later).
Radionuclide Attenuation Correction
Studies showed that SPECT MPI with radionuclide attenuation correction compared with non–attenuation-corrected images is associated with better test specificity while maintaining sensitivity to detect obstructive CAD. Attenuation correction also increases the normalcy rate, a term used to define the percentage of normal studies in a low-risk cohort. Although publications have demonstrated the improved prognostic capability of attenuation-corrected SPECT MPI, widespread clinical adaptation of radionuclide attenuation correction with SPECT MPI has been slow. In contrast, PET MPI images without attenuation correction are significantly degraded by attenuation and are not interpreted clinically or for research purposes. As a result, PET MPI with radionuclide attenuation correction has been widely used clinically and for research applications.
Attenuation-corrected PET MPI has diagnostic and prognostic value. The sensitivity and specificity of attenuation-corrected PET MPI for the diagnosis of obstructive epicardial CAD are very high (a weighted sensitivity of 90% and specificity of 89% for the detection of a single coronary artery stenosis of >50%). Overall, when compared with the published data for SPECT imaging, current data suggest a higher diagnostic accuracy for PET MPI with a higher specificity for the diagnosis of CAD.
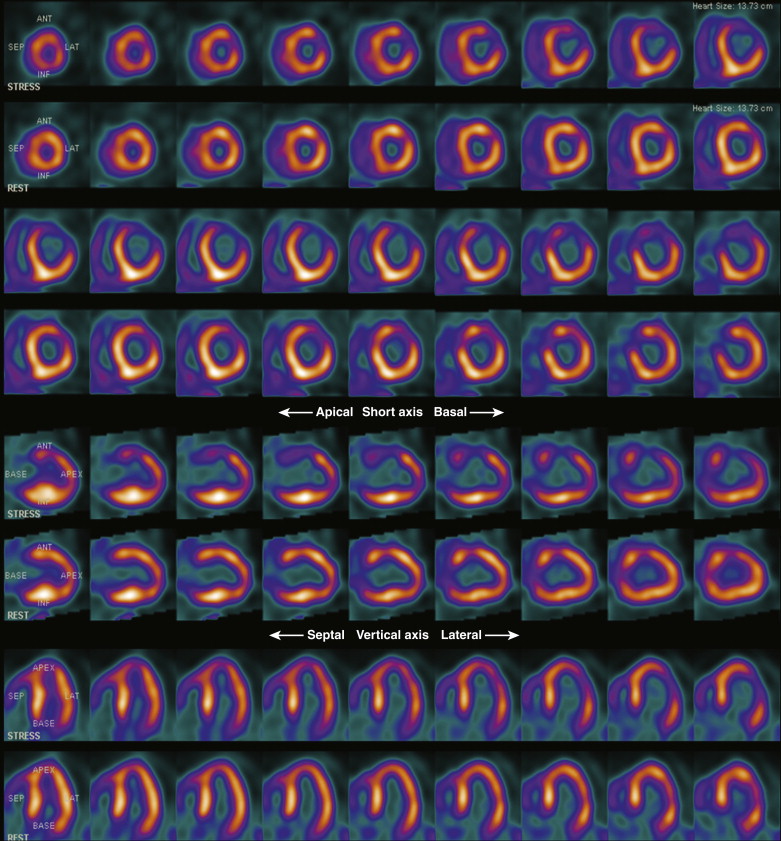
Computed Tomography–Based Attenuation Correction
SPECT-CT and PET-CT use low-dose x-ray transmission CT for attenuation correction, rather than an external radiation source. As previously mentioned, misregistration of CT attenuation-corrected and SPECT or PET MPI images may result from inherent differences in image resolution between CT and SPECT or PET MPI. Accurate registration is critical for improving the diagnostic yield of CT attenuation-corrected MPI. SPECT-CT MPI has been validated in patients with and without underlying CAD. Compared with uncorrected images, attenuation-corrected SPECT-CT MPI had improvements in specificity and normalcy. Figure 29-2 demonstrates the effect of attenuation correction using a hybrid SPECT-CT system. In patients with CAD, Sampson et al showed, in an Rb-82 PET-CT MPI study, that the sensitivity, specificity, and normalcy rates of MPI in 64 consecutive patients with intermediate risk of CAD who underwent coronary angiography following stress testing were 93%, 83%, and 100%, respectively. In addition, in 1433 patients, gated Rb-82 PET-CT MPI was associated with an excellent outcome in patients with a normal scan, but the investigators found increased event rates in patients with mild, moderate, and severely abnormal scans.
Risk Stratification
Both PET and SPECT MPI provide important prognostic information. Risk assessment with radionuclide MPI is based on stress variables and MPI variables. The stress variables that predict high risk are listed in Box 29-2 . Functional capacity is a very powerful predictor of adverse outcomes and should be carefully reviewed and reported.
Duration of symptom limiting exercise <5 METs
Failure to increase SBP >120 mm Hg or a sustained decrease ≥10 mm Hg or lower than at rest during progressive exercise
ST-segment depression ≥2 mm, down sloping, at <5 METs, ≥5 leads, ≥5 minutes into recovery
Exercise-induced ST-segment elevation
Angina at low workloads
Sustained (>30 seconds) or symptomatic ventricular tachycardia
Poor heart rate recovery (<12 beats/minute)
Chronotropic incompetence
Single Photon Emission Computed Tomography Myocardial Perfusion Imaging
The important MPI determinants of risk in patients with CAD are the extent of jeopardized myocardium, LV function, and other high-risk features. The extent and severity of perfusion defects are powerful predictors of outcome. Normal scans reflect a good prognosis, and abnormal scans reflect a poor prognosis. Further, the prognostic value of a given normal or abnormal scan result is modulated by patient-related factors, LVEF, and other high-risk scan features.
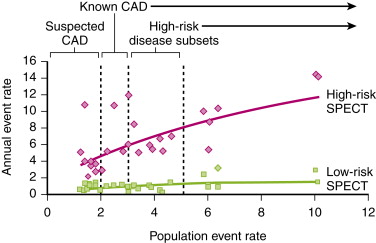
A meta-analysis that included 19 studies of more than 39,000 patients with an average 2.3-year follow-up found an event rate of 0.6% with a normal SPECT MPI result (64). The “warranty period” of a normal SPECT MPI study is considered to be approximately 2 years; however, patients with a history of CAD, pharmacologic stress, diabetes, and female gender appear to have higher event rates during year 2 after the index SPECT study. Patients with abnormal and high-risk MPI scans have much higher event rates ( Figs. 29-3 and 29-4 ). The presence and extent of reversible defects on stress MPI reflect jeopardized myocardium at risk for future damage. The number of myocardial segments with reversible defects has been reported to be the best predictor of future cardiac events, over clinical and angiographic data.
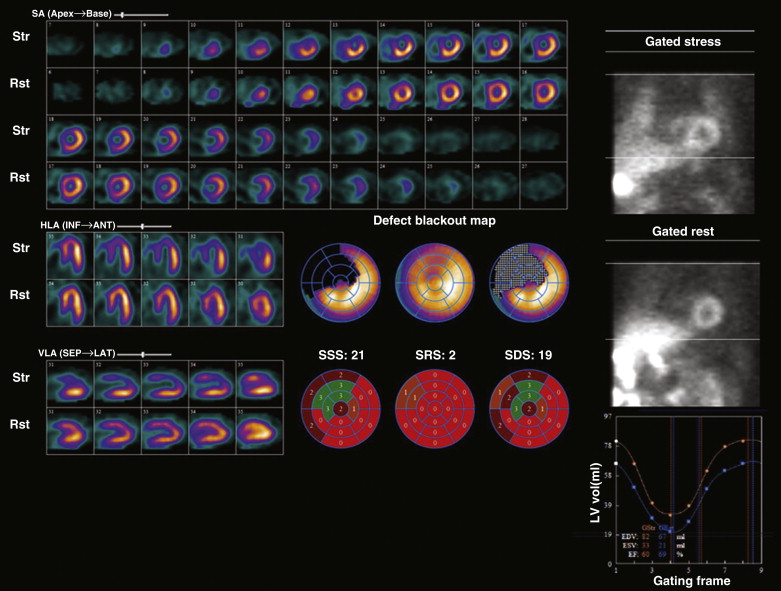
LVEF is the most direct measure of LV systolic function, and measurement of resting EF has been shown to be a crucial predictor of future cardiac events. Sharir et al reported on the incremental prognostic value of poststress LVEF by gated SPECT MPI. In a study of 1680 patients, these investigators demonstrated that for any given degree of scan abnormality, patients with an EF of less than 45% had higher rates of cardiac death. Similarly, LV volumes (>70 mL) were also important for risk stratification. These variables were predictive of worse outcomes among patients undergoing exercise stress or adenosine stress.
Several other markers of high risk have been identified on MPI ( Table 29-1 ). The presence of transient ischemic dilation of the LV cavity size with stress compared with rest on radionuclide MPI reflects global subendocardial hypoperfusion, as opposed to true cavity dilation from ischemia, as seen with exercise echocardiograms or dobutamine echocardiograms. Transient ischemic dilation is associated with severe and multivessel CAD. Increased lung uptake of radiotracer associated with elevated LV filling pressures also reflects LV dysfunction, extensive angiographic disease, and risk of adverse cardiac events. This situation was more frequently seen with Tl-201 imaging, in which scanning was started 10 to 15 minutes after completion of stress. However, when increased lung uptake is seen with Tc-99m studies, the pathophysiologic implications are the same as with Tl-201 studies. These high-risk scan features are particularly helpful in risk assessment when the scan shows only mild perfusion defects. Finally, studies suggest that the use of multicategory reporting of scan results (normal, probably normal, equivocal, probably abnormal, and abnormal) that incorporates the image findings, the stress findings, and clinical information provides enhanced risk stratification compared with a dichotomous normal or abnormal categorization based solely on image scores.
| Features | Identification | Implication And Pathophysiology |
|---|---|---|
| Perfusion defect size, severity and location | Qualitative and semiquantitative analysis on reconstructed slices Correlation of location of defect with coronary distribution | Large defect size (reflecting extent of CAD) and severity (reflecting severity of CAD) implying worse prognosis More than one coronary distribution affected implying multivessel coronary disease |
| Increased lung uptake (particularly with Tl-201) | Increased lung uptake during cine review of raw projection data; software program can generate lung-to-heart ratios using region of interest | Lung-to-heart ratio >0.54 Tl-201, or >0.45 Tc-99m a poor prognostic indicator of extensive LV ischemia, earlier infarct, or LV dysfunction |
| Transient dilation of the left ventricle after stress (TID) | Increased stress-to-rest LV cavity ratio; software programs can generate TID ratio | TID ratio >1.22 abnormal; abnormal TID ratio based on the study protocol Marker of extensive and severe CAD Sensitivity 71% and specificity 95% Postulated to be related to diffuse subendocardial ischemia versus true LV dilation at stress |
| Increased right ventricular uptake | Qualitatively assessed on raw projection data and on reconstructed data; software programs can generate RV/LV tracer uptake ratios using region of interest | Increased in the presence of RV hypertrophy resulting from pulmonary hypertension or relatively “increased” in the setting of global LV uptake reduction during exercise stress |
| Decrease in left ventricular systolic function | Gated SPECT display on multiple ventricular slices and software-generated LVEF | Poor prognostic indicator related to high-risk coronary disease or cardiomyopathy |
| Poststress global stunning | Analyzed as stress LVEF – rest LVEF using commercial software programs; a decline of LVEF >5% considered abnormal | Related to severe ischemia and significant or multivessel CAD |
| Reversible regional wall motion abnormalities | Poststress regional dysfunction and regional wall motion abnormalities that are not present or less severe on rest; visual review of the rest and stress-gated images | 53% sensitive and 100% specific for detection of severe CAD Presence of reversible regional wall motion abnormalities identifies >70% angiographic stenosis |
Positron Emission Tomography Myocardial Perfusion Imaging
The prognostic value of PET MPI has been well documented. Both Rb-82 and N-13 ammonia PET MPI have been shown to have prognostic value in patients with known or suspected coronary disease ( Table 29-2 ). In earlier studies, PET MPI was used in higher-risk patients with known CAD, whereas more contemporary studies confirmed the prognostic value of relative PET MPI in lower-risk patient cohorts. As with SPECT MPI, a normal relative PET MPI result is associated with excellent prognosis, and an increase in the extent and severity of stress perfusion defects is associated with worse outcomes. In a study of 685 patients with known CAD, Rb-82 dipyridamole stress demonstrated incremental prognostic value to clinical history and angiographic data. A normal study result was associated with a 0.9% annual event rate, whereas a positive study result was associated with a 4.3% annual event rate. Lertsburapa et al demonstrated that peak stress LVEF added significantly to clinical and MPI variables in predicting all-cause mortality. In addition, LVEF reserve (stress minus rest EF) provides significant independent and incremental value to Rb-82 PET MPI for predicting the risk of future adverse events. Annualized rates of cardiac events (2.1% versus 5.3%; P < .001) and all-cause death (4.3% versus 9.2%; P < .001) were significantly higher in patients who did not increase their LVEF from rest to peak stress. PET has also been found to be cost effective compared with angiography, exercise ECG, and SPECT in terms of quality-adjusted life-years.
| First Author | Year | Stress Agent | Tracer | Patients ( N ) | Events ( N ) | Event Type | Prior CAD (%) | Normal Scans (%) | Event /Year In Normal MPI (%) | Event /Year In Abnormal MPI (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Marwick | 1997 | Dipyridamole | Rb-82 | 685 | 81 | Cardiac death | Prior MI, 48%; prior revascularization, 37% | 24 | 0.9 | Mild, 2.6%; moderate, 5.1%; severe, 5.1% |
| Yoshinaga | 2006 | Dipyridamole | Rb-82 | 367 | 17 | Cardiac death or MI | 40.3 | 70.5 | 0.4 | Mild, 2.3%; moderate to severe, 7.0% |
| Lertsburapa | 2009 | Dipyridamole | Rb-82 | 1,441 | 132 | All-cause mortality | 53.6 | 64.8 | 2.4 | Mild, 4.1%; moderate to severe, 6.9% |
| Dorbala | 2009 | Dipyridamole Adenosine | Rb-82 | 1,432 | 140 | Cardiac death or MI | 30.6 | 54 | 0.7 | Mild, 5.5%; moderate, 5%; severe, 11% |
| Herzog | 2009 | Adenosine | N-13 | 256 | 29 | Cardiac death | 66 | 45 | 0.5 | 3.1 |
| Chow | 2009 | Exercise and dobutamine | Rb-82 | 124 | 16 | Cardiac death, MI, revascularization | MI, 40%; PCI, 29%; CABG, 15% | 37 | 1.7 | 13 |
The additional ability of PET to quantify absolute blood flow by dynamic imaging of tracer kinetics allows measurement of myocardial perfusion at rest and during stress, as well as CFR. CFR with vasodilators predominantly measures endothelium-independent coronary flow abnormalities and, to a lesser extent, endothelium-dependent flow abnormalities. In 51 patients with hypertrophic cardiomyopathy and 8-year follow-up, Cecchi et al showed that patients with the lowest tertile of dipyridamole-induced myocardial blood flow had worse outcomes compared with patients in the highest tertile. Furthermore, the degree of coronary microvascular dysfunction was an independent predictor of death and progressive heart failure in patients with dilated cardiomyopathy. Absolute myocardial perfusion may also be superior to quantitative coronary angiography in quantifying changes in myocardial blood flow in response to aggressive risk factor modification.
The prognostic value of vasodilator CFR when using N-13 ammonia or Rb-82 PET has also been investigated. In a study of 256 patients undergoing N-13 ammonia PET and a normal relative PET study, abnormal CFR was independently associated with a higher annual major adverse cardiac event rates over 3 years compared with normal CFR (1.4% versus 6.3%; P < .05). Despite the small number of patients, this was the first study to report the prognostic value of quantitative PET MPI in patients with known or suspected CAD. Similarly, another study that included 275 patients who underwent rest and dipyridamole stress Rb-82 PET MPI showed that a vasodilator CFR lower than the median value (2.11) was predictive of worse outcomes in the entire cohort, as well as in patients with normal relative PET MPI.
Endothelium-dependent flow abnormalities can be studied using cold pressor testing. In 72 subjects with chest pain and nonobstructive CAD, Schindler et al demonstrated that an impaired or decreased myocardial blood flow response to cold pressor test was associated with the highest incidence of cardiovascular events. Impaired cold pressor myocardial blood flow was independently associated with adverse cardiovascular events over and above coronary risk factors (smoking, hypercholesterolemia, hypertension, and increases in body mass index).
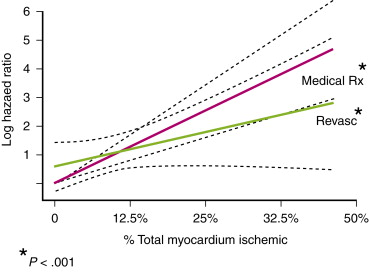
Myocardial Perfusion Imaging to Guide Patient Management
Radionuclide MPI results are also used to guide patient management. Hachamovitch et al were the first to demonstrate that patients with a large ischemic burden (>10% ischemic myocardium) had a lower hazard of cardiac mortality in the revascularization group compared with the medical therapy group ( Fig. 29-5 ). The nuclear substudy of the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) study also investigated this concept. The main COURAGE study was a randomized study that found no difference in major adverse cardiovascular events between patients who underwent percutaneous coronary revascularization and patients who received optimal medical therapy (OMT) alone. In the nuclear substudy of COURAGE, 314 patients underwent SPECT MPI at baseline and at 18 months. Percutaneous coronary intervention (PCI) plus OMT was found to reduce ischemic burden significantly compared with OMT alone, with the greatest benefit in patients with large ischemic burden, although this benefit was no longer evident on risk-adjusted analysis.
In response to therapeutic interventions, quantitative PET has been used in several research studies to evaluate progression or regression of atherosclerosis. In patients with dyslipidemia treated with aggressive risk factor modification (lifestyle changes and medications), quantitative PET is superior to quantitative coronary angiography in identifying response to therapy. This is because small changes in atherosclerosis that are not easily evident on coronary angiography may translate into much larger changes in myocardial blood flow that are readily imaged by quantitative PET imaging.
Cost Effectiveness of Radionuclide Myocardial Perfusion Imaging
In patients with chronic stable angina, SPECT MPI has been shown to be cost effective. In the Economics of Noninvasive Diagnosis (END) study that looked at 11,249 consecutive patients with stable angina, a strategy of initial medical therapy with MPI-guided coronary angiography compared with a strategy of direct coronary angiography was associated with significantly lower diagnostic and follow-up evaluation costs with no differences in outcomes. The Economics of Myocardial Perfusion Imaging in Europe (EMPIRE) study was another study (retrospective case-controlled study) from four countries (France, Germany, Italy, and the United Kingdom) that found that when considering exercise ECG, MPI, and coronary angiography, a strategy including MPI was cheaper and at least as effective compared with strategies not including MPI. In one study, SPECT MPI had a lower cost-per-unit effectiveness compared with an exercise ECG test over a wide range of pretest probabilities of CAD, whereas PET MPI had the lowest cost-per-effectiveness or cost-per-utility unit in patients with intermediate pretest likelihood of CAD (pretest likelihood of 0.70). In a group of intermediate-risk subjects, Merhige et al also showed that the downstream costs of evaluation following PET MPI were lower than those of SPECT at their institution, and costs were lower than that reported with SPECT MPI from the END study. The results of the ongoing Study of Myocardial Perfusion and Coronary Anatomy Imaging Roles in CAD (SPARC) study will likely illustrate the utility of various imaging tests (SPECT, PET, CT angiography [CTA], or hybrid SPECT or PET with CTA) in evaluating patients with intermediate pretest likelihood of CAD.
Practical Aspects
The specificity of SPECT MPI is diminished when attenuation artifacts are interpreted as perfusion abnormalities resulting from CAD. ECG-gated SPECT improves specificity, as does attenuation-corrected SPECT. Attenuation correction algorithms are much more robust with PET MPI, and hence attenuation-corrected PET MPI has better specificity than non–attenuation-corrected SPECT MPI.
Stress perfusion defects reflect a combination of infarction (fixed) and viable but ischemic myocardium (reversible) (SSS). Specifically, although reversible defects predict MI and fixed defects predict cardiac death, the combination of reversible and fixed defects is a stronger predictor of overall events. Identification of reversible defects on stress MPI implies a modifiable risk that can be improved by therapeutic interventions, either revascularization by bypass surgery or PCI or medical therapy.
Routine stress imaging after successful PCI or coronary artery bypass graft (CABG) is not indicated, unless patients have symptoms. In selected asymptomatic patients, repeat MPI may be considered 5 or more years after CABG and 2 or more years after PCI. Repeat MPI should always be compared with a preintervention study, and the examiner should know the details of the PCI. In patients who have undergone CABG, abnormal perfusion may persist despite patent grafts because of residual disease in the native nongrafted vessels. A classic pattern of proximal defects with preserved perfusion in the distal portion of the left ventricle suggests a patent left internal mammary artery (LIMA) graft with progression of native left anterior descending coronary artery disease proximal to the LIMA insertion ( Fig. 29-6 ). Moreover, in a patient with a pattern of perfusion defects in the apical segments with a patent LIMA graft on angiography, progression of vascular disease with subclavian artery stenosis should be considered. Septal wall motion abnormality is also common after CABG surgery, as is seen with any open heart surgery, left bundle branch block, or right ventricular pacing with left bundle branch block morphology.