- •
Multiple contrast weighted imaging sequences (including bright- and black-blood techniques) are needed for accurate assessment of the luminal surface condition and plaque composition.
- •
MRI is able to visualize carotid atherosclerosis at different stages and quantify atherosclerotic plaque burden.
- •
Assessment of luminal narrowing alone may underestimate atherosclerotic plaque burden and the stage of disease.
- •
Gadolinium contrast enhancement is beneficial for identification and quantification of the fibrous cap, lipid-rich necrotic core, and vessel wall inflammatory status.
- •
The common carotid artery bifurcation provides an internal fiducial marker for coregistration in serial MRI studies.
- •
Key plaque features identified by MRI, such as intraplaque hemorrhage and fibrous cap status, are associated with more rapid plaque progression and subsequent ischemic events.
Stroke is a leading cause of long-term disability and is the third most common cause of mortality in many countries. Carotid atherosclerosis is one of the causes of stroke. As a means to prevent cerebrovascular events, carotid endarterectomy has been advocated in patients with high-grade carotid stenosis. However, there is increasing evidence that luminal narrowing may be a poor predictor of carotid plaque vulnerability. The Asymptomatic Carotid Atherosclerosis Study noted that carotid endarterectomy was associated with a reduction in absolute risk for ipsilateral stroke of only 5.9% at 5 years, compared with medical management. If we assume that the projected risk reduction is equally distributed over the course of 5-year follow-up, only one stroke per year would be prevented for every 85 patients undergoing successful endarterectomy.
As such, additional criteria have been sought to better identify patients most at risk of complications from carotid disease. Based on analysis of histologic findings in carotid endarterectomy specimens, fibrous cap rupture, intraplaque hemorrhage, large necrotic cores with thin overlying fibrous caps, plaque neovasculature and inflammatory cell infiltration have been hypothesized to be features of the high-risk, vulnerable plaque.
Although histopathology studies have identified plaque features associated with prior ischemic events, it is not possible to determine risk for future events based on findings in excised tissue. Until recently progress toward prospectively testing the “vulnerable plaque hypothesis” has been hampered by the inability to accurately and reproducibly identify the crucial plaque features theorized to represent the high-risk lesion in vivo.
Cardiovascular magnetic resonance (CMR) imaging has been extensively validated by multiple investigators as an accurate and reproducible method to characterize human carotid atherosclerosis. Furthermore, CMR is ideally suited for serial studies of plaque progression and regression as it is noninvasive and does not involve ionizing radiation.
The case reports and the list of suggested reading that follow were selected to illustrate this chapter’s important points:
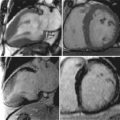
Figure 25-1 shows application of black-blood technique for identification of luminal and outer wall boundaries of carotid arteries.

A 58-year-old man with a history of hypercholesterolemia presented with right upper extremity weakness of four weeks’ duration. Duplex ultrasonography discovered a 50% to 79% stenosis in the left internal carotid artery and 1% to 15% stenosis in the right carotid artery. The patient underwent a carotid CMR examination before endarterectomy, which revealed the presence of a large lipid-rich necrotic core in the left carotid artery ( Figure 25-2 ).

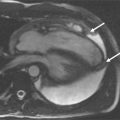
A 57-year-old man described multiple episodes consistent with left amaurosis fugax over a period of 5 weeks. Duplex ultrasonography discovered a 80% to 99% left midinternal carotid artery stenosis. A carotid CMR was performed before endarterectomy, which showed a large lipid-rich necrotic core in the left common carotid artery. Use of the contrast-enhanced T1-weighted sequence improved the delineation of lipid-rich necrotic core as well as the overlying fibrous cap ( Figure 25-3 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree