- •
Cardiac magnetic resonance (CMR) can be used to detect and quantify the most common complications after repair of tetralogy of Fallot. CMR can accurately measure pulmonary regurgitant fraction (phase-contrast CMR) and assess right ventricular function (cine CMR) and morphology in these patients.
- •
CMR can assess hemodynamic significance of recurrent or residual coarctation of the aorta.
- •
After surgical correction for transposition of great arteries, CMR can be used to evaluate for possible complications of atrial switch and arterial switch procedures.
- •
CMR can identify and estimated the severity of conduit stenosis and regurgitation after the Rastelli operation.
- •
CMR can be used to assess for the most common complications associated with the Fontan procedure, which are conduit stenosis or thrombosis and dysfunction of the single functioning ventricle.
A 28-year-old man presents with a recent history of shortness of breath and palpitation during exercise. Clinical examination is unremarkable, except for a diastolic cardiac murmur. Past medical history is significant for surgical correction of tetralogy of Fallot at the age of 4.
Comments
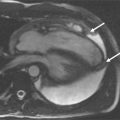
Pulmonary regurgitation is the most common complication observed after correction of tetralogy of Fallot, usually presenting clinically as intolerance to exercise. It is nearly always present in patients who underwent a transannular patch repair for correction of the right ventricular outflow tract stenosis and is often associated with dyskinesis or aneurysm on the patch area. Chronic pulmonary regurgitation eventually causes right ventricular dilatation and dysfunction. The CMR study can accurately measure pulmonary regurgitant fraction (phase-contrast CMR) and assess right ventricular function (cine CMR) and morphology in these patients ( Figure 16-1 ).


A 30-year-old woman presents with intolerance to exercise and shortness of breath. Clinical examination is noticeable for both systolic and diastolic murmurs. Patient underwent correction of tetralogy of Fallot with infundibulectomy and pulmonary valvotomy at the age of 2.
Comments
A common complication after correction of tetralogy of Fallot with infundibulectomy is residual infundibular and/or valvular pulmonary stenosis, which is usually associated with a mild to moderate degree of pulmonary regurgitation. Branch pulmonary artery stenosis is a common coabnormality seen in patients with tetralogy of Fallot and is often diagnosed later in life, after the initial surgical correction has been performed. A comprehensive CMR study allows for evaluation of morphology of stenosis and quantification of stenotic pressure gradient and ventricular function ( Figure 16-2 ).


A 35-year-old woman presents for clinical evaluation 1 year after coarctation of the aorta angioplasty because blood pressure levels remain higher in the upper extremities (BP: 160/100 mm Hg) than in the lower extremities (BP: 126/80 mm Hg). Clinical examination is unremarkable.
Comments
Residual or recurrent coarctation of the aorta is a common complication after either angioplasty or surgical intervention. CMR can not only assess the morphology of the coarctation site but also determine if the lesion is hemodynamically significant, based on the presence of collateral circulation ( Figure 16-3 ).