18
Carotid, Vertebral, and Spinal Arteriography
Although usually they are managed by neuroradiologists, especially in academic institutions, the head, neck, and spine are of interest to the vascular and interventional radiologist, who also may perform diagnostic and interventional procedures in these anatomic areas. This chapter provides a brief, overview of this vascular anatomy and pathology of these regions.
 Anatomy
Anatomy
Arteries of the neck
Within the superior mediastinum, the aortic arch normally gives rise to three major arteries that supply the upper extremities, head, and neck. The first branch is the brachiocephalic trunk, also called the innominate artery. This vessel courses superiorly for a short distance before bifurcating into the right subclavian and right common carotid arteries (Fig. 18-1). The right subclavian artery (RSCA) courses superiorly, gives off the right vertebral artery, and then turns laterally to supply the right upper extremity. The right common carotid artery (RCCA) courses superiorly to bifurcate into the right internal and external carotid arteries The second vessel off the aortic arch is the left common carotid artery, which travels cephalad and bifurcates into the left internal and external carotid arteries. The left subclavian artery is normally the final arch vessel. It courses superiorly before turning sharply laterally to supply the left upper extremity. The common carotid arteries are paired vessels located anteriorly within the neck. Each common carotid artery courses superiorly, along with the vagus nerve and internal jugular vein, without branching, and then it bifurcates into the internal carotid artery (ICA) and external carotid artery (ECA) (Figs. 18-2 and 18-3). The bifurcation of the common carotid artery is generally at the level of C3–4, but it may occur anywhere from C1–T2.1
The ICA supplies the anterior circulation of the brain as well as a portion of the skull base and is divided into four segments: cervical, petrous, cavernous, and supraclinoid. Only the cervical segment is extracranial. The most proximal portion of the ICA is posterolateral in relation to the ECA and then courses medially to enter the skull base through the carotid canal. The cervical ICA has no named branches. The remaining three segments of the ICA are named as to their location; the petrous and cavernous portions lie within the petrous bone and cavernous sinus, respectively, and the supraclinoid segment runs above the level of the anterior clinoid. The major arteries of the anterior circulation of the brain are branches of the supraclinoid ICA (Fig. 18-4).
The ECA is the smaller of the two branches of the common carotid artery. At its origin, the ECA is anteromedial to the ICA. The branches of the ECA are the superior thyroid, ascending pharyngeal, lingual, facial, occipital, and posterior auricular arteries. The ECA then bifurcates into the internal maxillary and superficial temporal arteries. Certain branches of the ECA may serve as important collaterals to the intracranial circulation in the setting of ICA stenosis or occlusion. These include the distal branches of the internal maxillary artery and the facial artery, both of which may fill the supraclinoid ICA by anastomosing with the ophthalmic artery. Less commonly, the ascending pharyngeal artery and the middle meningeal branch of the internal maxillary artery may serve as collaterals.
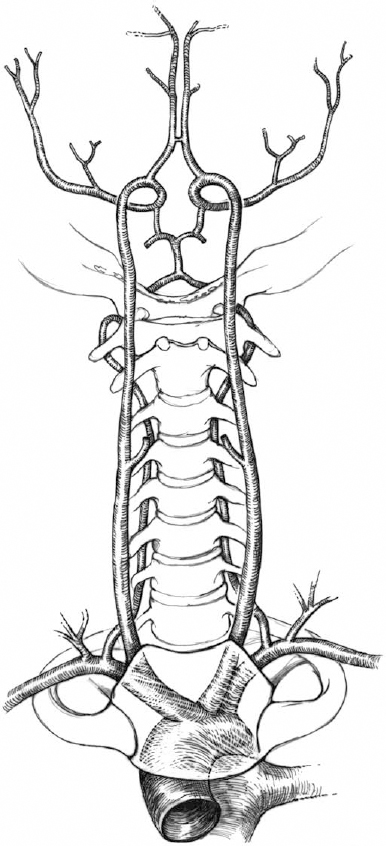
FIGURE 18-1. The aortic arch and its major branches (anteroposterior view).
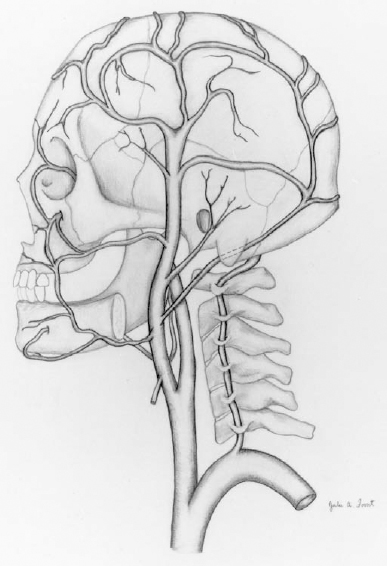
FIGURE 18-2. The external carotid artery and its branches.
The vertebral arteries arise as the first and largest branches of the subclavian arteries and supply the posterior circulation of the brain, spinal cord, and muscles of the neck. The vertebral arteries travel superiorly to enter the foramina transversaria of the C6 vertebra and then run within bony canals, exiting at the C2 foramena. The artery then turns sharply laterally to course around the lateral mass of C1 before returning medially to ascend through the foramen magnum to join and form the basilar artery. The occipital artery and ascending pharyngeal artery may serve as collateral supply to the vertebral arteries and posterior circulation.
Veins of the neck
The interal jugular veins (IJV), formed by the confluence of the sigmoid sinuses and the inferior petrosal sinuses, drain most of the blood from the brain (Fig. 18-5). The IJVs are paired structures that course inferiorly, lateral to the carotid arteries and deep to the sternocleidomastoid muscle (SCM) in the neck, to join the ipsilateral subclavian vein. The external jugular veins (EJV) drain portions of the face and neck; they course superficial to the SCM to join the subclavian veins. The vertebral veins arise in the occipital region from multiple small veins and travel inferiorly adjacent to the vertebral arteries within the foraminae transversaria to empty into the innominate veins.
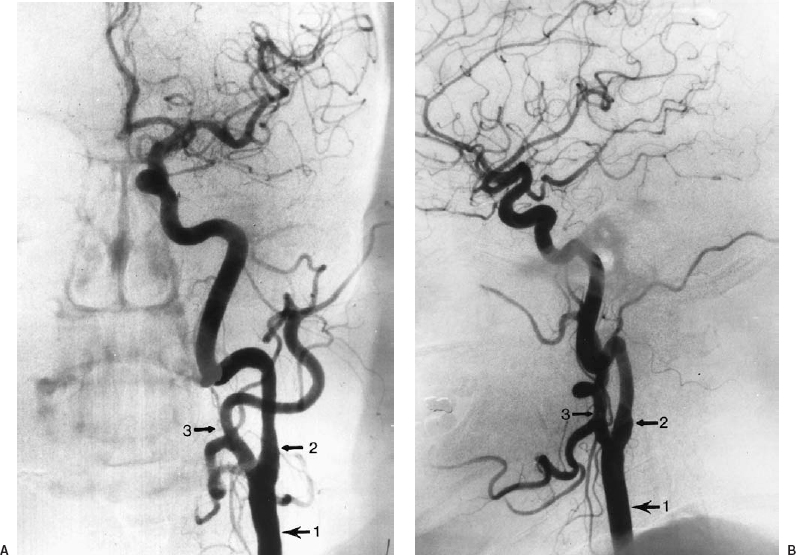
FIGURE 18-3. Film subtraction angiography of the left common carotid artery bifurcation in anteroposterior (A) and lateral (B) views demonstrate the normal branching pattern of the common carotid artery (1) into the internal (2) and external (3) carotid arteries.
 Pathologic Processes of the Arteries of the Neck
Pathologic Processes of the Arteries of the Neck
Atherosclerosis
Atherosclerosis is by far the most common disease process to involve the arteries of the neck. Caused by the formation of fibrofatty intimal plaques, its various manifestations include intimal calcification, vessel tortuosity, and ectasia. This process may progress to stenosis, occlusion, and dolichoectasia and aneurysm formation (Fig. 18-6). The most common sites of atherosclerotic stenoses within the neck are, in order of frequency, the common carotid bifurcation, origins of the ICA and ECA, the origins of the vertebral arteries, and the proximal subclavian arteries.2 Angiography has an important role in this disease: Several large-scale prospective studies found that carotid endarterectomy is effective in the long-term prevention of stroke in certain patients with moderate to severe stenosis.3,4
Fibromuscular dysplasia
Fibromuscular dysplasia (FMD) is an idiopathic process that leads to stenoses of medium to small arteries as a result of segmental overgrowth of fibrous and muscular elements of the arterial media and, to a lesser extent, the adventitia (Fig. 18-7). Originally described in renal arteries, FMD most commonly affects the cervical ICA, but it may involve any of the major arteries of the neck.2 FMD is often bilateral and is associated with spontaneous arterial dissection as well as intracranial aneurysms. It is more common in women and tends to occur in patients younger than the expected age distribution for atherosclerosis. Radiographically, FMD usually appears as alternating segments of stenosis and dilatation, producing a so-called “string of beads” appearance.
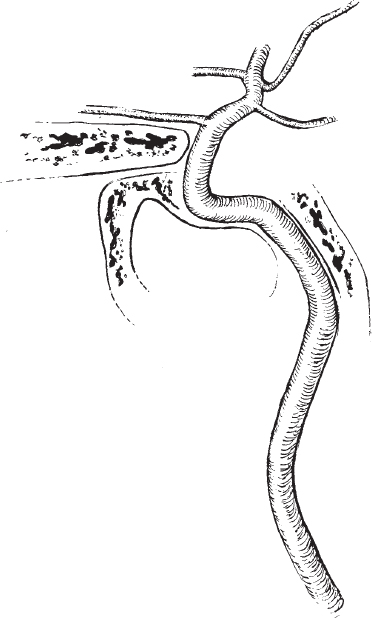
FIGURE 18-4. Internal carotid artery distribution (lateral view).
Takayasu arteritis
Takayasu arteritis, also known as pulseless disease, is characterized by long-segment, smooth stenoses of the proximal arch vessels, although any of the branches of the aorta may be involved (Fig. 18-8). The left subclavian is the artery that is most often involved, although typically several vessels are involved.5 The process often leads to complete occlusions of vessels. The disease typically affects females aged 15 to 45 years. The pathogenesis of this disease is unknown.
Giant cell arteritis
Giant cell arteritis is an idiopathic process manifested by focal granulomatous inflammation of medium and small arteries. This disease usually affects smaller vessels, such as the superficial temporal artery, but it may involve the larger vessels of the neck. The most common radiographic pattern in giant cell arteritis is multiple discrete stenoses.1
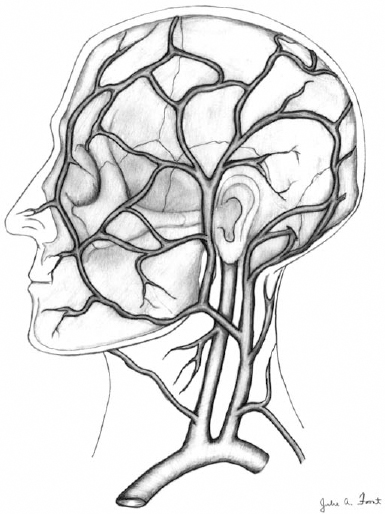
FIGURE 18-5. The draining veins of the cranium and neck.
Subclavian steal
In some cases, collateral pathways are already present but do not manifest until normal hemodynamics are altered, as in the case of subclavian steal syndrome. Subclavian steal syndrome occurs when the subclavian artery, most commonly the left, becomes occluded proximal to the origin of the vertebral artery. In this setting, the distal subclavian artery “steals” blood from the posterior circulation of the brain by means of retrograde flow through the ipsilateral vertebral artery (Fig. 18-9). The decreased blood flow to the posterior circulation of the brain may result in ischemia, from which patients often become symptomatic when exercising the affected upper extremity.
Trauma
Traumatic injury to the neck is a common indication for performing angiography, especially in the setting of penetrating trauma to regions where physical examination is difficult. By convention, the neck is divided into three zones:

FIGURE 18-6. Digital subtraction angiography of left common carotid artery in anteroposterior oblique projection demonstrates stenosis involving the carotid bulb with a focal collection of contrast projecting posteriorly. The appearance is typical of an ulcerated atherosclerotic plaque.
- • Zone 1 extends from the thoracic inlet to the cricoid cartilage
- • Zone 2 extends from the cricoid to the angle of the mandible
- • Zone 3 extends from the mandibular angle to the skull base.
Traditionally, penetrating trauma to zones 1 and 3 calls for an angiogram in most surgical algorithms, although angiographic studies for these “proximity” injuries have notoriously low yields.6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree