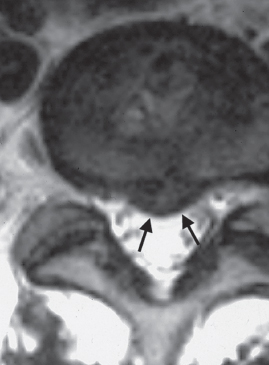
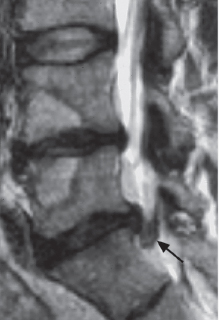
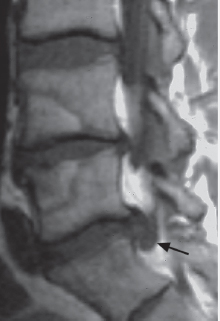
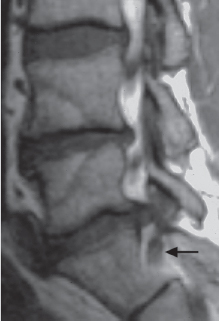
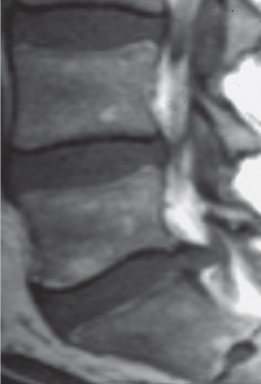
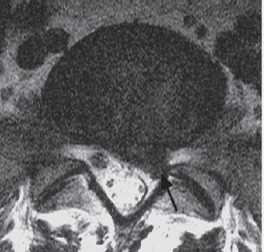
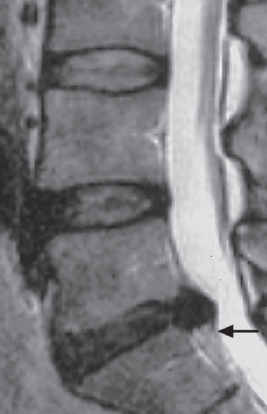
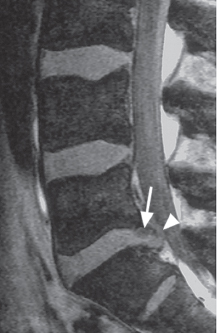
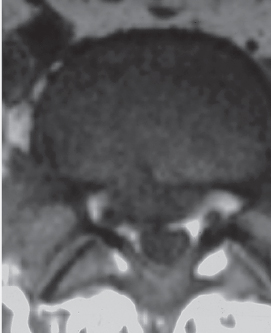
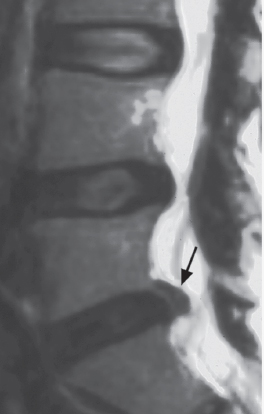
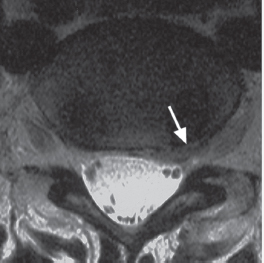
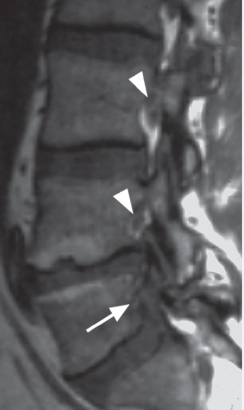
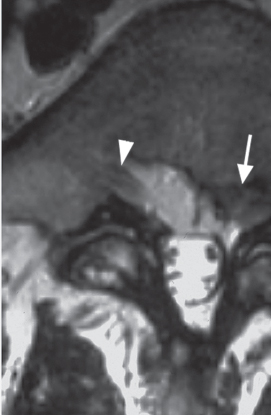
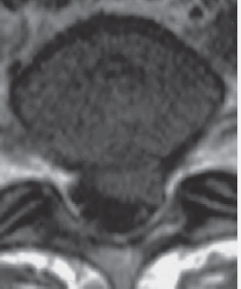
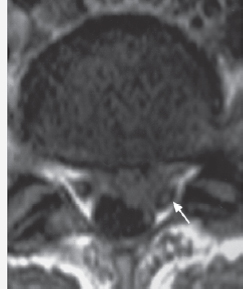
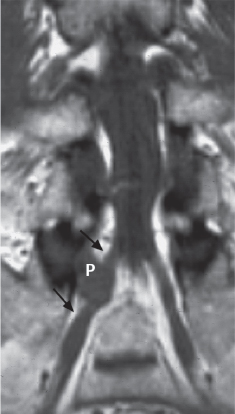
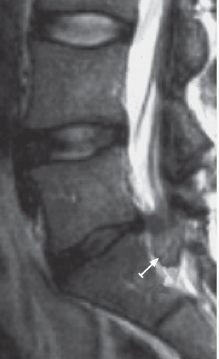
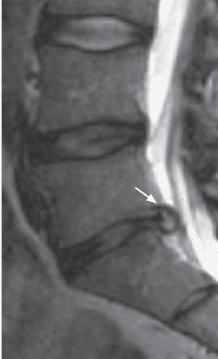
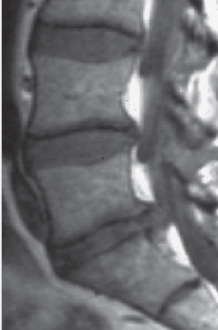
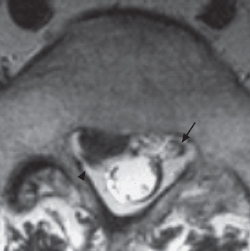
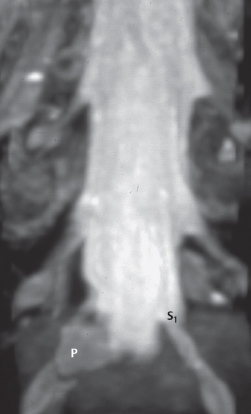
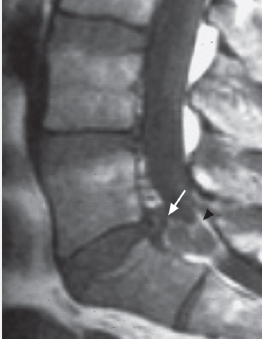
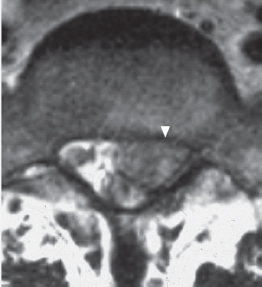
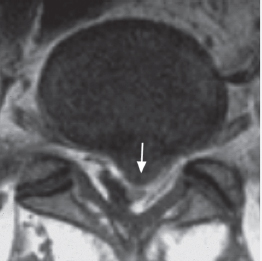
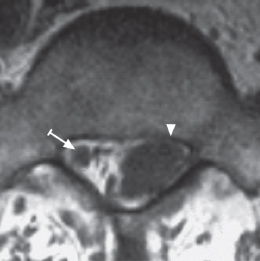
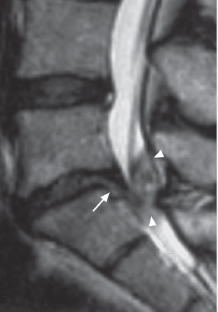
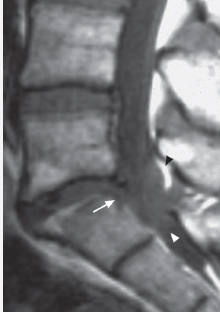
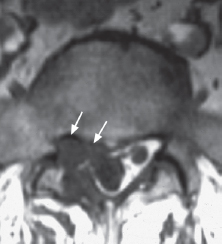
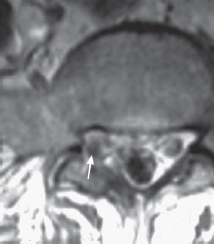
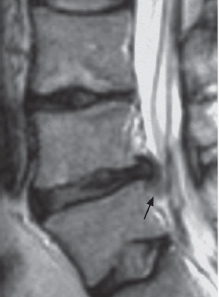
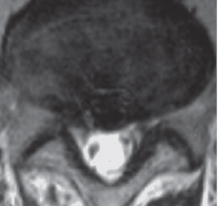
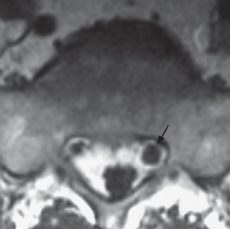
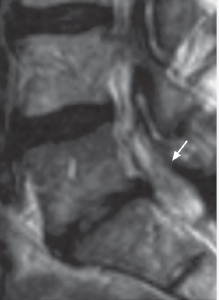
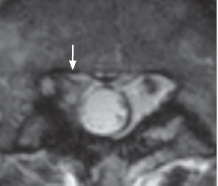
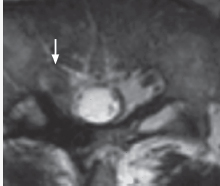
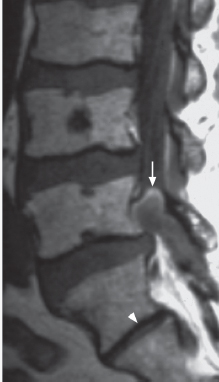
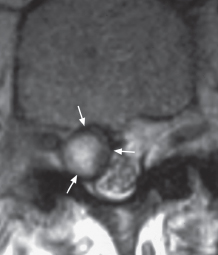
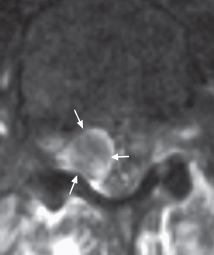
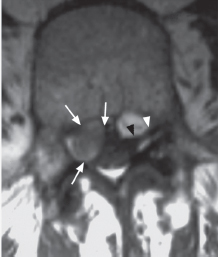
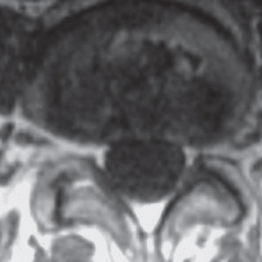
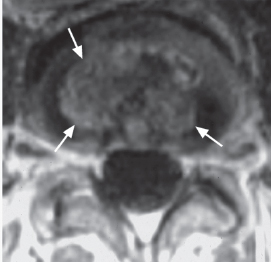
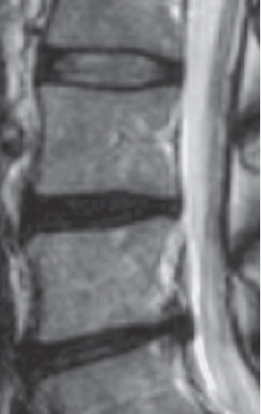
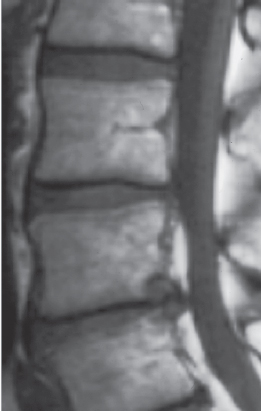
2 Case Studies This woman complained of variable lumbar symptoms, primarily involving the right side, while hospitalized for treatment of an unrelated problem in the foot. The pain radiated down the right posterior thigh and lateral calf to the lateral margin of the foot. Clinical examination revealed tenderness over the right sacroiliac joint. Examination sequences Fig. 2.1a T2 TSE, sagittal, median, Findings: This is a normal study. The annulus fibrosus and nucleus pulposus are well differentiated in both sagittal and axial slices. All lumbar disks are of normal height. There is no disk displacement. The posterior surface of the disk appears normal with a concavity at L3-4 (c1) and a hint of convexity at L5-S1 (c2). The width of the vertebral canal is normal. The facet joints appear normal. Diagnosis: Normal findings. Note: A concave posterior surface is a characteristic feature of all normal lumbar disks, with the exception of L5-S1, which tends to display a hint of convexity. In light of the clearly functional complaints without clinical neurological correlation, conservative treatment consisting of physical therapy and back training was provided. Fig. 2.1a Fig. 2.1b Fig. 2.1c1 This 22-year-old woman complained of deep sacral pain of three days’ duration, without radiation into the legs. Motion in the lumbar spine was painful at the end of the range of motion in every direction, and backward bending was markedly limited. Patrick’s four-part sign was positive, there were no significant neurological findings, and the Lasègue sign was negative on both sides. The clinical diagnosis was lumbar facet syndrome. Examination sequences Fig. 2.2a T2 TSE, sagittal, median, Findings: The nucleus pulposus and annulus fibrosus are of normal signal intensity on the T2 image, with a slight posterior height reduction and minimal posterior bulging in the L3-4 disk (a, b, →). In the axial slice, the concavity of the posterior surface of the disk is preserved (c1); see case study 1. The width of the dural sac is normal. Diagnosis: Discrete degenerative disk disease at L3-4, with otherwise normal findings. The patient’s condition improved markedly over the next few days after treatment with heat and analgesics (aspirin). The clinical findings suggest that this patient’s back pain is attributable to the facet joints of the lower lumbar segments. This is a facet syndrome. MRI is useful for the differential diagnosis, but provides no positive findings contributing to the diagnosis. On the basis of the MR image, one can rule out inflammatory and neoplastic processes in this area of the spine. MRI should be considered the imaging study of choice in future for the exclusion of such processes in young patients, whenever a study for this purpose is indicated. Fig. 2.2a Fig. 2.2b Fig. 2.2c1 This 58-year-old man complained of low back pain of three to four years’ duration and the recent onset of pseudoradicular pain radiating into the posterolateral aspect of both legs. Shortly before these images were obtained, the pain had increased, with paresthesia in both legs and feet when walking, and pain on bending backward, primarily on the left side. Examination sequences Fig. 2.3a T2 TSE, sagittal, paramedian, Findings: The signal intensity is markedly diminished in the two lower disks with only a slight reduction in height (a, b). There is mild posterior displacement of disk tissue at L4-5 and L5-S1, with only mild impression of the dural sac at L5-S1 (c2) but with a relatively intense signal in the posterior periphery of the disk (a, →). The bone marrow is of normal signal intensity. Diagnosis: Disk degeneration with mild protrusions in the two distal segments. Conservative outpatient treatment to flatten the lordosis, facet joint infiltration, abdominal muscle training, relaxation in a supine position with hips and knees flexed, and Discoflex bandage. The symptoms improved slightly with conservative therapy. The protrusions extend only to the outer layer of the annulus fibrosus (grade 2 displacement; see Fig. 1.6) and do not constitute an indication for invasive treatment, especially in light of the mild symptoms. Therapeutic measures to flatten the lumbar lordosis are indicated. Finally, the MRI study itself was not indicated, as an invasive segment-specific therapeutic procedure was not under consideration. Fig. 2.3a Fig. 2.3b Fig. 2.3c1 This 32-year-old woman complained of sacral pain variably radiating into her left and right legs, of three months’ duration. The pain radiated from the buttocks across the posterior aspect of both thighs to the popliteal fossa. The mobility of the lumbar spine was limited, especially on forward bending. Neurological examination revealed no deficit. The Lasègue sign was positive on the left at 70° and on the right at the end of the range of motion. Examination sequences Fig. 2.4a T2 TSE, sagittal, median, Findings: A circumscribed, medial posterior protrusion of the L5-S1 disk is present, accompanied by markedly diminished signal intensity and mildly diminished height. The dural sac is compressed, without displacement or compression of the nerve roots (a-c). Diagnosis: Medial protrusion or medial subligamentous extrusion with osteochondrosis at L5-S1. Note: The relatively thick, dark demarcation (→) represents what is known as the “annuloligamentous complex.” Its individual component structures, which cannot be reliably distinguished from one another, include the peripheral portions of the annulus fibrosus, the posterior longitudinal ligament, the epidural membrane, and the dura mater. The definition of a disk extrusion requires perforation of the annulus fibrosus. As the annulus fibrosus cannot be reliably distinguished from the other structures listed, it is difficult to distinguish a subligamentous extrusion from a circumscribed protrusion in cases like this. In a circumscribed disk displacement, thickening of the annuloligamentous complex most likely represents portions of the annulus fibrosus and would therefore suggest a protrusion. Conservative therapy was provided, as no clear radicular syndrome was present. The patient’s condition improved markedly with relaxation in a supine position with hips and knees flexed, application of a flexion orthosis, and local injections, especially epidural perineural injections and spinal nerve analgesia. Direct nerve root compression was not present, so conservative therapy lasting several months was recommended. No operation should be performed in cases like this, because exposure of the medial protrusion would require strong retraction of the dural sac and nerve roots. Aside from this, the disk in question is intact. If the disk pathology should recur with reappearance of leg symptoms, intradiskal therapy, such as chemonucleolysis with chymopapain, could be considered. Fig. 2.4a Fig. 2.4b This 40-year-old man complained of low back pain and left-sided sciatica of three months’ duration. The band of pain corresponded to the left S1 segment. The pain was of moderate intensity; he was able to sleep at night, and he felt pain during the day only with certain movements. Examination revealed a diminished left Achilles tendon reflex and a positive Lasègue sign on the left at 60°. Examination sequences Fig. 2.5a T2 TSE, sagittal, left paramedian/paramedial (a1) and left paramedial/lateral (a2), Findings: Disk degeneration is present in the last two segments, which are of diminished signal intensity and diminished height (a, b). Marked changes (Modic type II) are seen in the superior and inferior end plate at L4-5. The L4-5 disk and especially the L5-S1 disk (a-c) are posteriorly displaced, narrowing the left caudal intervertebral foramen (c1, →). The subligamentous portions of the disk are of relatively high signal intensity on the T2 image (c1, Diagnosis: Broad-based disk protrusion in the last two segments with stenosis of the left intervertebral foramen at L5-S1 due to a subligamentous extrusion. In light of the moderate pain and the moderate extent of the findings at L5-S1, conservative treatment was provided. The treatment included epidural perineural injections on the left side in segment L5-S1, appropriate relaxation exercises, and physical therapy. The symptoms improved, and the patient returned to his office job. Neither the clinical findings nor the MRI findings are particularly severe. Part of the compressed tissue in the left lateral recess of S1 corresponds to the left S1 nerve root, which is thickened because of edema. Fig. 2.5a1 Fig. 2.5a2 Fig. 2.5b1 Fig. 2.5b2 Fig. 2.5c1 Fig. 2.5c2 This 55-year-old man complained of sciatica in the left S1 distribution, of six weeks’ duration, refractory to orthopedic outpatient treatment with spinal analgesics. There was an ipsilateral postural deformity on forward bending. A band of pain and hypesthesia with formication was present on the lateral margin of the foot. The Achilles tendon reflex was absent on the left side, and the Lasègue sign was positive on the left at 40° and negative on the right. Examination sequences Fig. 2.6a T2 TSE, sagittal, left paramedial, Findings: Left paramedial posterior displacement of disk tissue is seen. The dural sac is not compressed, because the vertebral canal is wide, but there is marked displacement of the left S1 nerve root, which is difficult to distinguish in the T1 and T2 images (→, c, d). The intervertebral disk makes broad-based contact with the nerve root (a, b). Diagnosis: Large left paramedial intervertebral disk extrusion at L5-S1 without sequestration and with compression of the left S1 nerve root. The severe pain (the patient constantly required powerful analgesics, both day and night) and MRI findings demonstrating disk extrusion constituted an indication for surgery, which was scheduled for the next day during normal hours. An interlaminar approach at L5-S1 was used. The ligamentum flavum lay in the middle of the surgical exposure, and the severely thickened S1 nerve root was immediately beneath it. The extruded disk tissue lay directly under the nerve root, part of it projecting into the root axilla. Part of the extruded disk was still located within the posterior confines of the disk space. A fragment of the superior end plate was visible within the intraspinal portion of the extrusion. This fragment was in direct medial contact with the nerve root (see Fig. 1.6; grade 4 displacement). Fragmented disk structures were found, consisting of 50% nucleus pulposus, 40% annulus fibrosus, and 10% superior end plate fragment. The patient was free of pain immediately postoperatively. Some residual formication was present on the lateral margin of the foot. There was hardly any need for postoperative analgesics. Three months postoperatively, the patient remained free of symptoms with the exception of formication on the lateral margin of the foot. Severe pain due to nerve root compression by hard, extruded fragments provided the surgical indication. Because of this compression by hard fragments, the patient still had paresthesia in the distal S1 dermatome postoperatively. Given the clear clinical situation and MRI correlation, surgery could have been performed earlier. Fig. 2.6a Fig. 2.6b Fig. 2.6c This 47-year-old man had suffered from low back pain radiating into the left leg for five years. At the time of examination, he complained of formication and mild pain in the left S1 dermatome. There was no neurological deficit. Examination sequences Fig. 2.7a T2 TSE, sagittal, median, Findings: The L5-S1 intervertebral disk is of diminished signal intensity (a). Marked posterior displacement of disk tissue is seen in segment L5-S1, with only mild compression of the dural sac in a relatively wide vertebral canal (a-c). The extruded tissue remains continuous with the parent disk and elevates the posterior longitudinal ligament (a, b, →). Diagnosis: Medial and right paramedial extruded disk at L5-S1, without sequestration. Note: The MRI examination failed to identify an imaging correlate for involvement of the left S1 nerve root (c, →). Because of the discrepancy between the imaging studies, which showed right L5-S1 disk pathology, and the symptoms affecting the left S1 dermatome, and because the latter were only mild, conservative treatment was provided. This consisted primarily of left spinal nerve analgesia, epidural perineural injections, appropriate relaxation exercises, back training, etc. The left-sided symptoms gradually improved, but the sacral pain remained unabated. The left-sided symptoms are not explained by the images. Conceivably, the partially medial extrusion on the right could have caused traction displacement of the left S1 nerve root, which over a period of years of chronic involvement has become adherent to adjacent structures. Any surgical intervention at L5-S1 would have had to be bilateral. Here the risk of further symptoms due to postoperative scarring would not have been justified, in light of the mild presenting symptoms. Fig. 2.7a Fig. 2.7b This 32-year-old man complained of pain radiating into the right leg in an S1 dermatomal pattern, of several months’ duration. There was no significant postural deformity. Examination revealed moderate weakness of the right plantar flexors, a band of hypesthesia in the right S1 dermatome, and an absent right Achilles tendon reflex. The Lasègue sign was positive on the right at 30°, and negative on the left. Examination sequences Fig. 2.8a T2 TSE, sagittal, right paramedian, Findings: The lowest disk is of diminished height and signal intensity. There is circumscribed posterior displacement of disk tissue, primarily in the medial zone, without significant compression of the dural sac or nerve roots (a-d). The posterior portion of the disk and the extruded tissue are of low signal intensity (a, b, c, →). A hypointense line is seen along the posterior surface of the extrusion; an interruption of this line is seen only on the sagittal FLASH image (c, Diagnosis: Medial and paramedial subligamentous extrusion in segment L5-S1 without significant compression of neural structures. Note: The signal intensity on the T1 and T2 images is nonspecific, but the areas of diminished intensity in the FLASH sequence suggest a circumscribed calcification or ossification, indicative of an earlier “hard” extrusion. CT can provide precise information in this setting. The hypointense line along the posterior surface of the extrusion appears to be interrupted on the sagittal FLASH image only. This line represents the annuloligamentous complex or a portion of it. This finding alone, however, does not suffice for MRI diagnosis of a transligamentous extrusion (see also case study 56). Surgery was indicated in light of the severe pain and failure to respond to previous treatment. Exposure at L5-S1 revealed a medial area of hard resistance due to a subligamentous extrusion at the disk level, part of which extended to the infradiskal level. The posterior portion of the annulus fibrosus was opened to reveal sequestrated fragments of cartilaginous end plate, which were easily extracted with holding forceps and required no additional mobilization. Hard extruded components undergo very little enzymatic resorption. Thus, surgical removal was indicated in this case, also because of the severe pain. Fig. 2.8a Fig. 2.8b Fig. 2.8c This 50-year-old woman complained of low back pain radiating into the left leg, in a pattern corresponding to the S1 dermatome and part of the left L5 dermatome, of two months’ duration. There were no motor or sensory deficits, and the left Achilles tendon reflex was absent. The Lasègue sign was positive at the end of the range of motion on the left side. Examination sequences Fig. 2.9a T2 TSE, sagittal, left paramedial, Findings: The L5-S1 disk is of diminished signal intensity and normal height (a, b). There is circumscribed paramedial displacement of the disk in segment L5-S1 (a, b, →), with relatively high signal intensity on the T2 image (c, →). The dural sac is mildly compressed and the left S1 nerve root, which is poorly distinguishable, is displaced (c2, Diagnosis: Left paramedial extrusion in segment L5-S1 at the disk level with partial stenosis of the superior portion of the left S1 lateral recess. Because of the relatively mild clinical findings with a small extrusion at L5-S1 and a wide vertebral canal, conservative therapy was provided. The patient reported marked subjective improvement after combined injection therapy with epidural perineural injections and spinal nerve analgesia. These findings do not require surgery, and the extruded disk tissue is not accessible to treatment with intradiskal procedures. Fig. 2.9a Fig. 2.9b Fig. 2.9c1 This 48-year-old woman had undergone surgery for an acute right-sided disk extrusion at L5-S1 (at disk level) three years previously. She presented a second time with acute pain radiating into her left leg of one week’s duration. The pain radiated across the buttocks to the posterolateral aspect of the left high. Examination revealed marked weakness in the left dor-siflexors, such that the patient was unable to walk on her heels. There was an area of hypesthesia and hy-palgesia corresponding to the left L5 dermatome. The Achilles tendon reflexes were symmetrically strong. Abnormal spontaneous activity was found in the left L5 index muscles (tibialis anterior and extensor hal-lucis longus), with high potentials and no more than mild evidence of reinnervation, indicative of acute injury to the left L5 nerve root. Examination sequences Fig. 2.10a T2 TSE, sagittal, left paramedian (a1) and left lateral (a2), Findings: Left cranial displacement of disk tissue originating from the L5-S1 disk is seen, with stenosis of the left L5-S1 intervertebral foramen (a-d). Demarcation is much less distinct on the T2 image (a, →) than the T1 image (b, →), but the T2 image exhibits considerable motion artifact. The extruded tissue →) is in contact with the left L5 spinal ganglion ( Diagnosis: Supradiskal, intraforaminal left L5-S1 disk extrusion. It was decided that immediate surgery was indicated because of the position of the herniated tissue with weakness of the dorsiflexors and signs of acute nerve root injury at electromyography. The inferior margin of the L5 vertebral arch was removed to expose the supradiskal space. Findings superior to the last intervertebral disk included a supradiskal, lateral extrusion projecting into the intervertebral foramen, directly adjacent and inferior to the exiting left L5 nerve root. The patient was free of symptoms immediately postoperatively. The dorsiflexor weakness regressed during the first few days after surgery and was absent three months later. Surgery was clearly indicated by the relatively acute dorsiflexor weakness, with evidence of acute denervation. The disk operation that had been performed under the operating microscope three years earlier had evidently left no more than a few, barely visible contralateral changes. This effectively rendered the current operation equivalent to an initial intervention. Fig. 2.10a1 Fig. 2.10a2 Fig. 2.10b1 Fig. 2.10b2 Fig. 2.10c This 50-year-old man had suffered from sacral pain for several years, which had initially radiated in a pseudoradicular pattern. He recently began complaining of left-sided sciatica radiating into the L5 dermatome and partially into the S1 dermatome on the left, of three months’ duration. Conservative treatment was initially provided, consisting of epidural perineural and paravertebral injections, bed rest, and a flexion orthosis, without significant improvement. Upon admission to the hospital, the patient had no postural deformity and reported pain in a left L5 and S1 distribution. The dorsiflexors were of normal strength. The Achilles tendon reflex was slightly diminished on the left side. The Lasègue sign was positive at 60° on the left side, and negative on the right. Examination sequences Fig. 2.11a T2 TSE, sagittal, left paramedian, Findings: There is markedly diminished signal intensity in the last two intervertebral disks, accompanied by diminished height in disk L4-5 with slight protrusion, and type II medullary changes as described by Modic (a, b). The L5 vertebra is anteriorly displaced relative to S1, and disk tissue is displaced cranially posterior to the vertebral body of L5 as far as its cranial third, without stenosis of the dural sac (a-d, →). The left lateral recess of the L5 vertebra is narrowed, and the left L5 nerve root cannot be distinguished, while the other nerve roots are well visualized (c, d, Diagnosis: Spondylolisthesis at L5-S1 with a left paramedial, supradiskal disk extrusion and secondary involvement of the left L5 nerve root. Osteochondrosis and protrusion are present at L4-5. Note: Cranial displacement of disk tissue in spondylolisthesis is a common finding (a, b) that should not be mistaken for a true extrusion or protrusion. In this case, a genuine extrusion (c, d) causing radicular symptoms is present in addition to the “pseudoex-trusion.” Because of the persistent, intractable symptoms and the correlated MRI findings, it was decided that diskectomy without spinal fusion was indicated as regularly scheduled surgery. Access was gained to the left side of L5-S1, and the inferior margin of the L5 vertebral arch was removed to expose the supradiskal space. A subligamentous or submembranous sequestrum was found in a lateral supradiskal position, causing compression of the L5 nerve root from cranially to caudally, and of the dural sac with the exiting S1 nerve root medially. The disk protrusion could be followed back to the L5-S1 intervertebral space. The symptoms improved postoperatively. The distal leg pain disappeared, but formication persisted in both the L5 and the S1 dermatomes on the left side. The three-month follow-up revealed marked improvement of the radicular symptoms. The sacral pain and proximal band of pain were still present. Because this case involved both spondylolisthesis and disk protrusion, intensive conservative therapy was first attempted, but this failed to bring significant relief. The most important consideration at surgery was to decompress the L5 and S1 nerve roots by removing the displaced disk tissue. The patient’s further course will reveal whether the local and radicular pain due to the spondylolisthesis remain within acceptable limits. If necessary, a posteroanterior spinal fusion may be considered as a revision procedure. Fig. 2.11a Fig. 2.11b Fig. 2.11c This 29-year-old woman complained of acute back pain radiating into the left leg in a pattern corresponding to the S1 dermatome. Severe lumbar spasm was present. Examination revealed mild weakness of the left plantar flexors, and a diminished Achilles tendon reflex on the left. Examination sequences Fig. 2.12a T2SE, axial, L5-S1 (a1) and L5 inferior end plate (a2). Findings: There is an extrusion originating at the L5-S1 disk and extending to the infradiskal level with compression of the dural sac and displacement of the left S1 nerve root (a, →). Three years later, only a small amount of soft tissue is seen at the same site, without compression of the dural sac (b2, c, →). The L5-S1 intervertebral disk is of diminished signal intensity. The disks of the upper segments of the lumbar spine appear normal. Lumbarization of S1 is seen, with a hypoplastic intervertebral disk (d, →). Diagnosis: a A large infradiskal medial and left paramedial extrusion is present at L5-S1. b-d Subtotal regression of the extrusion has occurred, with residual disk tissue or scar tissue anterior to the dural sac, and without compression of the dural sac or nerve root. The L5-S1 intervertebral disk is degenerated. The patient underwent conservative treatment consisting of relaxation in a supine position with hips and knees flexed, analgesics, and local injections (spinal nerve analgesia). Subjective improvement was reported within a few days, and surgery was deemed unnecessary. The patient returned for examination three years later. Mild back pain was still present, occasionally radiating into the left leg, especially with weather changes. There was no motor deficit nor positive findings other than a diminished left Achilles tendon reflex. The extruded L5-S1 disk was largely resorbed by enzymatic action. Remnants persist in the form of fibrous tissue in the anterior epidural space, without compression of the root or dural sac. Even a large, extruded disk does not require immediate surgery if there is no major neurological deficit and the pain is only moderately severe. In young patients, the extruded tissue consists primarily of nucleus pulposus tissue, and will be more readily broken down by enzymatic action than a comparable amount of extruded tissue in older patients. Fig. 2.12a1 Fig. 2.12a2 Fig. 2.12b1 Fig. 2.12b2 Fig. 2.12c This 42-year-old patient had previously suffered from sacral pain, but not from sciatica. She began complaining of unbearable pain in the right leg of two weeks’ duration, requiring continuous analgesic medication (opioids and other medications). An ipsi-lateral sciatic postural deformity was present, with a band of pain in the right S1 dermatome. There was moderate weakness in the right plantar flexors, and the right Achilles tendon reflex was absent. The Lasègue sign was positive on the right at 40° and negative on the left. Examination sequences Fig. 2.13a T2 TSE, sagittal, right paramedial, Findings: The last two lumbar disks are of markedly diminished height and signal intensity. Right paramedial posterior displacement of disk tissue is seen at the L5-S1 level, with severe compression of the dural sac (a-d) and the right S1 nerve root (d), which cannot be clearly defined. The arrow indicates the left S1 nerve root (d2). Soft-tissue structures of higher signal intensity than the L5-S1 disk are also seen posterior to S1 in the T2 image (a). The sagittal T1 images, in particular, demonstrate that this tissue is clearly separated from the disk (a, b, c, →). The distance from the posterior superior margin of the sacrum to the center of the sequestrum is approximately 1 cm. There is marked peripheral contrast enhancement around the extrusion (c, d2, →). Diagnosis: Paramedial extrusion at the disk level at L5-S1 on the right side, with a free infradiskal sequestrum. The right S1 nerve root could not be visualized. Because of the patient’s severe pain and correlative MRI findings, diskectomy was performed the next day during normal operating hours. After fenestration at L5-S1, disk tissue was immediately seen protruding from the disk level into the root axilla, between the medial margin of the nerve root and the lateral wall of the dural sac. The red and edematous S1 nerve root was readily identifiable. The sequestrum was located further distally and was extracted after a laminectomy of the sacrum. The patient showed marked improvement immediately postoperatively. Formication in the right S1 dermatome persisted after surgery, but was only mild on follow-up three months later. Dorsiflexor strength was normal. Immediate surgery was performed because of the severe pain and the correlative MRI findings, although the symptoms of nerve root irritation had been present for only two weeks. The MRI finding of a sequestrum 1 cm inferior to the superior margin of the sacrum was helpful for the microsurgical procedure. Inadequate imaging findings could have led the surgeon to concentrate on the disk level and overlook the sequestrum in the sacral canal. Fig. 2.13a Fig. 2.13b Fig. 2.13c Fig. 2.13d1 This 55-year-old man had suffered for several years from low back pain and sciatica, occurring alternately on both sides, which had never been accompanied by weakness and had always been treated conservatively. He recently started complaining of pain in the right posterior calf in an S1 dermatomal distribution and weakness of plantar flexion on the right, of about three weeks’ duration. On examination, he could not walk on tiptoe with the right foot, and the right Achilles tendon reflex was absent. There was hypesthesia on the lateral margin of the patient’s right foot and the posterolateral aspect of the calf. The Lasègue sign was positive on the right at the end of the range of motion. Examination sequences Fig. 2.14a T2 TSE, sagittal, right paramedian, Findings: Posterior to the first sacral vertebra, there is a soft-tissue mass of inhomogeneous signal intensity that does not communicate with the L5-S1 intervertebral disk (a, b, →). There is marked compression of the dural sac and the right S1 nerve root, which is poorly visualized (c, d, →). All of the lumbar disks are of diminished height, and some of them exhibit marked protrusion. Disk degeneration and Modic type II bone marrow changes are present in the L4-5 segment. (P = extrusion) Diagnosis: A right paramedial infradiskal sequestrum is present at the S1 level; the parent intervertebral space cannot be identified with certainty. Several segments exhibit disk degeneration, with posterior and anterior protrusion and Modic type II bone marrow changes. The severe pain, paralysis of plantar flexion, and relatively large sequestrum in the sacral canal, with severe compression of the dural sac and a high risk of cauda equina syndrome, constituted an urgent indication for surgery, which was scheduled for the next day during normal hours. The skin incision was centered 2 cm inferior to the marked disk level. A lateral flavectomy was performed in the inferior portion of the interlaminar window. The superior margin of the sacrum was removed. Sequestrated disk tissue was found anterior to the ligamentum flavum and sacrum, and lateral and posterior to the S1 nerve root. The opening of the sacral canal on the right side was carried well inferior to the point of exit of the S1 nerve root. The S1 nerve root was found to be edematous, with bluishred discoloration, over a length of more than 2 cm. The sequestrum lay well inferior to the L5-S1 intervertebral space. It was decided to remove the sequestrum without performing a diskectomy at L5-S1 or at higher levels. The specimen consisted of fibrous cartilage with focal degenerative changes of intermediate severity. Focal areas of myxoid necrosis were present. An analysis of the percentages of the various components was not performed. Leg pain was markedly diminished, but formication in the right S1 dermatome remained and was still present three months later. The sacral pain was unchanged. This patient had suffered from disk-related symptoms in the lumbar spine for years, with sacral pain and sciatica occurring alternately on both sides. The symptoms became acutely severe when a large sequestrum was extruded into the vertebral canal on the right side at level L5-S1. This produced neurological deficits relating to the right S1 nerve root. Surgery was indicated only for relief of the symptoms due to the sequestrum in the sacral canal. The MRI findings correlated with the clinical neurological findings. The associated changes at levels L4-5 and L3-4 were not clinically relevant. The medial compression of the dural sac at level L4-5 demonstrated by MRI did not correlate with the patient’s symptoms. Therefore, the decision was made not to undertake any surgical correction of levels L3-4 or L4-5, and the operation was limited to the removal of the sequestrum. Further correction would have produced epidural scarring which, in combination with the protrusions at L3-4 and L4-5, might well have caused a worsening of symptoms postoperatively. The changes at levels L3-4 and L4-5 were managed conservatively, as before. Fig. 2.14a Fig. 2.14b Fig. 2.14c This 36-year-old man had suffered from back pain for 14 years, usually on weekends after athletic activity. One week before presentation, during a severe bout of sneezing, he suddenly felt pain in his back with intense radiation into the right leg in the S1 dermatome, which persisted thereafter. There was subjective numbness in the foot and calf. In the days immediately before presentation, he required large quantities of analgesics. Examination revealed weakness of both plantar and dorsiflexion on the right side, and a band of hypesthesia in the S1 dermatome, corresponding to the area of the pain. The right Achilles tendon reflex was diminished. The Lasègue sign was positive on the right at 40°, and negative on the left.. Examination sequences Fig. 2.15a T2 TSE, sagittal, right paramedial (a1), and left paramedial (a2). Findings: A circumscribed, posterior disk displacement is seen, with high signal intensity on the T2 images (→, a2, c1). Furthermore, a soft-tissue mass of homogeneous signal intensity, separate from the disk, can be followed to ca. 18mm below the disk level, obscuring the right S1 nerve root, but only moderately compressing the dural sac (→, a-c). Diagnosis: Circumscribed medial subligamentous extrusion of disk L5-S1 accompanied by an infradiskal right paramedial sequestrum. Note: The presence of a sequestrum can be diagnosed only on the T2-weighted images. Because of the severe pain and the demonstration of a massive sequestrum on MRI, urgent surgery was indicated and was scheduled for the next day during normal hours. The incision was centered 2 cm inferior to the marked disk level. A lateral flavectomy was performed in the inferior portion of the L5-S1 interlaminar window. The superior margin of the sacral hemilamina was removed down to 2 cm inferior to the disk level, as determined from the preoperative MR image. Several sequestrated fragments were found in the sacral canal, some medial to the right S1 nerve root and some lateral to it. The right S1 nerve root was exposed to a point 2.5 cm inferior to the disk marking. The specimen consisted of 10% hyaline cartilage, 65% annulus fibrosus, and 25% nucleus pulposus. The patient was free of pain immediately postoperatively, but mild formication remained on the lateral margin of the foot and was still present three months later. Severe pain, a massive sequestrum, and paresis both of the dorsiflexors and of the plantar flexors provided clear indications for surgery. The dorsiflexor weakness is referable to the L5 nerve root and cannot be explained by the position of the sequestrum in the sacral canal. Conceivably, severe anterior displacement of the dural sac may have exerted traction on the L5 nerve root in the right intervertebral foramen at L5-S1. The surgical opening of the sacral canal was carried to a point 2 cm inferior to the disk marking, in accordance with the precise information derived from MRI. We were thus able to avoid unnecessary removal of bone either from the sacrum or from the L5 hemilamina, which would have been associated with an increased risk of scarring. Fig. 2.15a1 Fig. 2.15a2 Fig. 2.15b1 Fig. 2.15b2 Fig. 2.15c1 This 63-year-old man complained of severe pain radiating into the right leg, of one week’s duration. He required analgesics constantly, but did not complain of weakness. Lumbar spasm was evident, and there was a band of pain and hypesthesia in the S1 dermatome on the right. There was no motor deficit. The right Achilles tendon reflex was absent, and the Lasègue sign was positive on the right at 30°. Examination sequences Fig. 2.16a T2 TSE, sagittal, median, Findings: There is posteriorly displaced disk tissue originating from the L5-S1 intervertebral disk. This tissue communicates with the parent disk only on the images shown here (a, b, →), but otherwise appears to be sequestrated. This tissue extends approximately 1.5 cm below the level of the disk, down to the mid-S1 level. There is no significant compression of the dural sac, but the right S1 nerve root is markedly compressed (c, d, Diagnosis: Almost completely sequestrated right paramedial infradiskal disk extrusion at L5-S1. The patient was admitted to the hospital and underwent a regime of appropriate relaxation exercises. Infusions and paravertebral injections failed to bring about any improvement. The patient continued to require large amounts of analgesics, and it was decided that surgery was indicated. Because the sequestrum was displaced quite far caudally, a flavectomy was performed in the inferior portion of the L5-S1 interlaminar window, and part of the sacral hemilamina was removed. The sequestrum consisted partially of hard components (see below). Annulus fibrosus components accounted for 70% of the specimen, hyaline cartilage for 15%, and nucleus pulposus for 15%. The patient was free of leg pain immediately postoperatively. Mild hypesthesia persisted on the lateral margin of the foot and was still present three months later. The patient was still free of leg pain on repeated follow-up. Surgery was performed early in the course of the disorder because of the severe pain, even though there was no neurological deficit. The dramatic pain associated with the sequestrated tissue in this location was primarily attributable to the consistency of the extruded tissue, which mainly consisted of fragments of annulus fibrosus and cartilaginous end plate. Fig. 2.16a Fig. 2.16b Fig. 2.16c This 37-year-old patient complained of severe pain in the left leg and less severe pain in the right leg, radiating across the posterolateral aspect of the leg to the heel. There was weakness of the urinary sphincter as well as “saddle” hypesthesia, more pronounced on the left side. Examination sequences Fig. 2.17a T2 TSE, sagittal, paramedian, Findings: Posteriorly displaced disk tissue is seen (a, b, c1, d1) which communicates with the parent disk (→). There is also sequestrated disk material (a, b, c2, d2) in the vertebral canal ( Diagnosis: Massive extrusion with sequestration at the infradiskal level of segment L5-S1, about 2 cm inferior to the disk space. Note: The relatively high signal intensity on the T2 image suggests that the displaced material consists of nucleus pulposus tissue or of inner portions of an annulus fibrosus that has not yet undergone marked degeneration. The presence of cauda equina syndrome constituted a surgical emergency, and the patient underwent immediate surgery. A massive sequestrum was found in the sacral canal, medially displacing the dural sac. Portions of the sequestrum were situated directly beneath the ligamentum flavum. The cauda equina findings and leg pain subsided immediately postoperatively. Emergency surgery was clearly indicated by the clinical findings. MRI revealed the size of the sequestrum and thereby enabled performance of this intervention as a microsurgical procedure through a narrow exposure. The preoperative images clearly showed absence of disk-related pathology cranial to the L5-S1 disk level and thus obviated the need for exploration above this level. Fig. 2.17a Fig. 2.17b Fig. 2.17c1 Fig. 2.17c2 Fig. 2.17d1 This 43-year-old woman complained of pain in both legs, more intense on the right, in an S1 dermatomal pattern. There was marked lumbar spasm. Examination revealed mild weakness of plantar flexion on the right, and a positive Lasègue sign on both sides at 60°. There were no findings suggestive of cauda equina syndrome. Examination sequences Fig. 2.18a T2 TSE, sagittal, median, Findings: The last intervertebral disk is of diminished height and signal intensity (a, b). There is posterior displacement of disk tissue in the medial zone, a small portion of which is located at the infradiskal level and communicates with the parent L5-S1 disk (a, b, c1, →). An additional soft-tissue mass is seen in the posterior portion of the vertebral canal and is in contact with the posterior hemilamina of S1 (a, b, c, Diagnosis: A medial extrusion is present with a short infradiskal extension and a large sequestrum that may have migrated to an intradural (i.e., intrathecal) location. Note: The tentative diagnosis of a sequestrum in a partially intradural position is made because images obtained in several axial planes (c2) fail to visualize a clearly demarcated right border of the dural sac and because sequestrated fragments are demonstrated medial to what is thought to be the dura (c1). Surgery was performed because of the severe pain and the MRI findings suggesting an intradural sequestrum. Surgery revealed a large interlaminar sequestrum lying directly on the dura mater at L5-S1, causing marked compression of the dural sac. The dura mater was found to be intact. There was also a small, covered extrusion of the L5-S1 intervertebral disk, with infradiskal extension. The patient showed marked improvement immediately postoperatively. Formication was still present in the S1 dermatome on the right side. The weakness of the plantar flexors subsided. Intrathecal sequestra have been described in the literature but are seen extremely rarely, if at all. In our series of 2000 disk operations, we have never observed an intrathecal sequestrum. Fig. 2.18a Fig. 2.18b Fig. 2.18c1 Fig. 2.18c2 This 48-year-old woman had undergone a disk operation at level L5-S1 one year earlier and complained of persistent pain. The original pain had never fully subsided after surgery, and there was further development of severe back pain radiating into the right leg in the S1 dermatome in every bodily posture, but particularly on standing and sitting. Examination reveled a well-healed 8-cm scar in the lumbosacral region. There was no weakness. A band of pain and hypesthesia was present in the right S1 dermatome and part of the right L5 dermatome. The Achilles tendon reflex was diminished on the right side. The Lasègue sign was positive on the right at 30° and on the left at 50°. The distance from the patient’s fingertips to the floor on maximal forward bending was 50 cm. Examination sequences Fig. 2.19a T2 TSE, sagittal, right paramedial, Findings: The L5-S1 intervertebral disk is of markedly diminished height and signal intensity (a). The T1 image reveals a hypointense soft-tissue mass at the level of L5-S1, which appears slightly hyperin-tense in the T2 image (a, b, →). The axial T2 image (c) reveals a circumscribed mass of low signal intensity (-0 that mildly compresses the dural sac. The right intervertebral foramen is obstructed by a soft-tissue mass (→). The right S1 nerve root is poorly visualized. The axial T1 image reveals a hypointense soft-tissue mass in the vertebral canal on the right side (d, →), which enhances markedly with contrast. The right S1 nerve is also readily seen in this image (e, →) Diagnosis: Circumscribed medial recurrent protrusion and perineural scarring involving the right S1 nerve root, after a previous diskectomy at L5-S1. Conservative therapy was provided. Subsequent spinal fusion may be indicated in case of failure to respond to treatment. Conservative therapy with a total of two epidural perineural injections and 10 spinal nerve analgesic treatments resulted in marked improvement. By eight months after treatment, the pain had largely, but not fully, resolved. This case involved a decompensated postdiskectomy syndrome. Irritation of the right S1 nerve root persisted despite removal of an extruded disk at L5-S1, and edematous inflammatory changes ensued (see MRI findings). Epidural perineural injections around the right S1 nerve root, together with a series of spinal nerve analgesic treatments, successfully desensitized the nerve root and reduced inflammation, and the symptoms resolved accordingly. The symptoms were due to perineural scarring. Any possible segmental instability at L5-S1 would not be affected by this treatment. Physical therapy and back training can control the symptoms. A posteroanterior spinal fusion at L5-S1 should be considered in the event of recurrent decompensation. Fig. 2.19a Fig. 2.19b Fig. 2.19c Fig. 2.19d This 49-year-old man had undergone surgery one year previously for a right-sided disk extrusion at L5-S1 and had never been completely free of pain thereafter. He recently started complaining of severe pain in the right leg, and occasionally also in the left leg, of two days’ duration. This was accompanied by a sensation of numbness in the perianal region. Sphincter function was unimpaired. Examination sequences Fig. 2.20a,f T2 TSE, sagittal, paramedian, Images f-i were obtained 6 months after images a-e. Findings: The last two intervertebral disks are of diminished height and signal intensity. The first postoperative study (a-e) revealed a small residual or recurrent protrusion (extrusion?) at L5-S1 with scarring (a, b, e, →) around the right S1 nerve root. The second study (f-i) revealed a massive recurrent extrusion that is well demarcated from the parent disk (f, Diagnosis: The initial postoperative scan revealed a small residual or recurrent protrusion or extrusion, with postoperative perineural scarring. The current scan reveals a massive, recurrent, right paramedial extrusion at L5-S1, with what appears to be a subli-gamentous sequestrum. Note: Only the T1 contrast series, and the fat-saturated images in particular, show a distinction between the nerve root and the extruded tissue. The massive extrusion with incipient cauda equina syndrome constituted a surgical emergency, and the patient underwent immediate surgery. A large extrusion originating from the L5-S1 intervertebral disk was found beneath the scar and was removed in its entirety. The patient showed marked improvement immediately postoperatively. Residual formication persisted, as did a band of pain in the S1 dermatome in the right leg. Emergency surgery was indicated by the perianal numbness, severe pain, and correlative MRI findings. It is highly surprising that the disk at L5-S1 was able to produce such a large extrusion after having undergone surgery before. Fig. 2.20a Fig. 2.20c Fig. 2.20d Fig. 2.20e1 Fig. 2.20e2 Fig. 2.20f Fig. 2.20g Fig. 2.20h This 46-year-old man had undergone disk surgery on the left side at L5-S1 one and a half years previously. Three months postoperatively, he developed increasing pain, primarily in the left leg, radiating into the S1 dermatome. He reported frequent cramps in the left calf. At the time of imaging, a band of pain and hypesthesia was present in the S1 dermatome bilaterally, more pronounced on the left. There was no motor deficit; flexion and extension of the left foot were limited by pain. The Lasègue sign was positive on the left at 40° and on the right at 60°. Examination sequences Fig. 2.21a T2 TSE, sagittal, left paramedian (a1) and left paramedial (a2), Findings: The L5-S1 intervertebral disk, which had been operated upon previously, is of mildly diminished height and markedly diminished signal intensity. A soft-tissue mass is seen posterior to the disk on the left side, and the left S1 nerve root is thickened (a2, b2, d, →). The soft-tissue mass is of markedly increased signal intensity (→, c) and cannot be differentiated from the left S1 nerve root. The arrowhead indicates the normal left L5 nerve root (a2, b2). Diagnosis: Extensive epidural scarring involving the left S1 nerve root. There is no evidence of a recurrent extrusion. The patient was hospitalized for conservative therapy with epidural perineural injections, spinal nerve analgesia, and an accompanying program of physical therapy. The patient showed marked improvement after a total of three epidural injections. The pain resolved and did not recur by the time of the next follow-up three months later. Only the formication and limited range of motion of the lumbar spine persisted. The patient found these symptoms tolerable. MRI clearly demonstrated the absence of any recurrent or residual extrusion. The S1 nerve root was markedly thickened and was edematous distal to the scar. The vertebral canal was wide and contained a large amount of epidural fatty tissue. Local anti-inflammatory treatment with cortisone may help in such cases, but the injection must be epidural, directly at the affected nerve root. Back training can lessen irritation of the S1 nerve root due to improper movement. If this treatment proves unsuccessful, neurolysis with a lateral fat flap may be considered, as part of a lumbar lateral release. Fig. 2.21a1 Fig. 2.21a2 Fig. 2.21b1 Fig. 2.21b2 Fig. 2.21c1 Fig. 2.21c2 This 44-year-old woman had undergone disk surgery at L5-S1 on the right side three and four years previously. The second operation was for revision of the epidural scarring. The symptoms in the right leg recurred six weeks postoperatively and worsened over time. The pain was particularly severe in the distal portion of the right S1 dermatome (i.e., the posterior aspect of the calf and the lateral margin of the foot). Outpatient treatment, including CT-guided injections into the right L5-S1 intervertebral foramen, failed to bring about any marked improvement. She presented to us again for the management of postdiskectomy syndrome. Examination revealed a 10-cm cutaneous scar, indicating extensive reoperation. A band of pain and hypesthesia was present on the right side in the L4 and L5 dermatomes, with formication on the dorsum and lateral margin of the foot. The Achilles tendon reflex was absent on the right side, and the Lasègue sign was positive at 30° on the right and at 60° on the left. Examination sequences Fig. 2.22a T2 TSE, sagittal, right paramedial, Findings: There is an area of high signal intensity on the T2 image (a, c, →) and of low signal intensity on the T1 image (b, d, →) to the right of the dural sac, which is not displaced (c-e). This area becomes inhomogeneous, with greater signal intensity at the periphery (e), after i. v. administration of gadolinium. In some of the images, this area cannot be differentiated from the right S1 nerve root, which appears thickened further inferiorly (c2, d2, e2, →). Marked degeneration of the L5-S1 intervertebral disk is seen, with diminished signal intensity, diminished height, and disk protrusion. Diagnosis: Right peridural scarring after two disk operations, without evidence of recurrent extrusion, but with residual protrusion and disk degeneration at L5-S1. Note: Given the primarily peripheral contrast enhancement and the absence of mass effect, we interpret these findings as peridural scar tissue with thickening of the right S1 nerve root. The patient was hospitalized for conservative therapy with epidural perineural injections. After three treatments with epidural perineural injections of 1ml of bupivacaine, combined with acupuncture, appropriate relaxation exercises, back training, and motion therapy, a 50% reduction in pain was achieved during the in-patient stay. Follow-up examination three months later revealed further marked improvement but not complete resolution of the symptoms. Should conservative treatment fail to bring about marked improvement, surgical intervention may be considered. This may include neurolysis primarily in segment L5-S1, with a lateral release of the dural sac and the S1 nerve root at the disk and infradiskal levels, and the application of fat flaps between the margin of the nerve root and the vertebral canal. Fig. 2.22a Fig. 2.22b Fig. 2.22c1 Fig. 2.22c2 Fig. 2.22d1 Fig. 2.22d2 Fig. 2.22e1 This 79-year-old man presented to the emergency room with excruciating pain in the right leg radiating into both the anterior aspect of the right leg (L4 dermatome) and the posterolateral aspect of the right leg (L5 and/or S1 dermatomes). The pain had greatly increased within the last few days prior to admission and was also present when the patient was supine. There was hardly any pain in the back or sacral area. Neurological examination revealed no weakness or reflex abnormality. Areas of hypesthesia were present in the right L4, L5, and S1 dermatomes. The Lasègue sign was positive on the right at 50°. Examination sequences Fig. 2.23a T2 TSE, sagittal, right paramedial, Findings: A sharply demarcated, round mass of low signal intensity on the T1 image and high signal intensity on the T2 image is seen anteromedial to the right L5-S1 facet joint (d1, →). This mass is distinct from the posteriorly displaced L5-S1 intervertebral disk and extends upward into the right lateral recess of the L5 vertebra (c-e), where it markedly compresses the dural sac at the origin of the right L5 nerve root (d2, →), while the origin of the contralateral nerve root (d2, Diagnosis: Synovial cyst of the right L5-S1 facet joint with compression of the right L5 nerve root. Slight protrusion of the L5-S1 intervertebral disk was also present. Surgery was performed because of the severe pain and unequivocal, correlative MRI findings. A right flavectomy was performed and the right part of the L5 inferior vertebral arch removed to expose an extensive cyst displacing the dural sac far medially. Solid granulation tissue was found in the superior part of the cyst. The patient was free of leg pain immediately postoperatively. Mild formication was present for a few days afterward on the right side in the L5 dermatome and part of the S1 dermatome, but then subsided. The patient was still free of symptoms at follow-up examination three months later. Percutaneous cyst aspiration might have been an alternative emergency treatment but would have provided only temporary relief. It was thus decided to resect the large cyst which was markedly compressing the dural sac. The operation was performed exclusively in the posterior epidural space and did not require access to the anterior epidural space, in which venous bleeding is usually more pronounced. Fig. 2.23a Fig. 2.23b Fig. 2.23c Fig. 2.23e Fig. 2.23d1 This 42-year-old man complained of the recent exacerbation of back pain from which he had suffered for three years. The question of spondylodiskitis was raised. Examination revealed tenderness to deep palpation over the spinous processes of vertebrae L3, L4, and L5, and over parts of the sacrum, without segmental radiation. The erythrocyte sedimentation rate was 15/31, and the CRP and leukocyte count were within the normal range. AP and lateral lumbar spine radiographs revealed slight narrowing of the L4-5 and L5-S1 intervertebral spaces but were otherwise normal. Examination sequences Fig. 2.24a T2 TSE, sagittal, Findings: Markedly decreased signal intensity is seen in the lowest three intervertebral disks, accompanied by diminished height of the last two (a, b). The dural sac is slightly compressed by disk tissue of the lowest three segments. The portions of vertebral bodies L4 and L5 adjacent to the disks are of slightly decreased signal intensity on the T1 images and increased signal intensity on the T2 images. Diagnosis: Protrusions and disk degeneration are present in the lowest three segments. In segment L4-5, these are accompanied by Modic type I bone marrow changes. Note: These findings suggest an edematous process in vertebral bodies L4 and L5, probably secondary to relatively acute disk degeneration. The absence of increased signal in the intervertebral disk on the T2 images, the intact end plates on the T1 images, and the relative mildness of the signal changes are all inconsistent with spondylodiscitis. Conservative treatment (physical therapy, back training). Spondylodiscitis was ruled out by MRI and clinical follow-up examination. The protrusions of the lowest three intervertebral disks (see MRI) are not clinically significant. Fig. 2.24a This 47-year-old man complained of low back pain of two years’ duration, without satisfactory response to conservative treatment. The patient was afebrile, and the laboratory findings were normal. Examination sequences Fig. 2.25a T2 TSE, sagittal, median, Findings: The noncontrast T1 and T2 images reveal markedly increased signal intensity in the L4 and L5 vertebrae, while the fat-saturated T1 images after gadolinium injection reveal markedly decreased signal intensity in portions of these vertebrae (a-c). The L4-5 intervertebral disk is markedly narrowed, and there are contour irregularities of its delimiting end plates (a, b). Marked, inhomogeneous contrast enhancement is seen in the L4-5 intervertebral disk (c, d2, →) and, to a lesser extent, in the superior half of the L5 vertebral body. Diagnosis: Active, erosive osteochondrosis in segment L4-5, with Modic type II bone marrow changes. There is no evidence of disk protrusion or extrusion. Note: The findings of this study are unchanged in comparison with the study of one and a half years earlier. Laboratory parameters of inflammation are negative. Spondylodiscitis is ruled out on MRI by the absence of bone marrow edema, the intact marginal ridges of the inferior and superior end plates, and the minimal or absent contrast enhancement of the vertebral bodies. Enhancement in the L4-5 intervertebral disk is consistent with erosive osteochondrosis. Conservative therapy was provided instead of disk aspiration for putative spondylodiskitis, because of the negative laboratory findings and the unequivocal exclusion of spondylodiskitis by the plain radiographs and MR images. Conservative treatment, with physical therapy and local infiltration, yielded only mild improvement. The negative laboratory findings, the images obtained over a period of years, and the MRI images all support the diagnosis of advanced degenerative changes in segment L4-5. Fusion is not indicated as there are no radicular findings, and the intervertebral space will solidify further over time. Fig. 2.25a Fig. 2.25b Fig. 2.25c Fig. 2.25d1 This 50-year-old man complained of chronic, recurrent low back pain occasionally radiating into the left buttock and lateral thigh. These symptoms had been present for several years and increased in intensity over the course of the day. Examination revealed lumbar spasm limiting the range of motion of the lumbar spine in every direction. No sensory or motor deficit was found, the deep tendon reflexes were normal, and the Lasègue sign was negative on both sides. Examination sequences Fig. 2.26a T2 TSE, sagittal, median, Findings: The lowest three intervertebral disks are markedly diminished in height and signal intensity, indicating degenerative disk disease (a). Mild disk protrusions, without significant compression of the dural sac, are present at multiple levels, most pronounced at L4-5 (a-c). A circumscribed area of hypointensity (→, c2) is seen medial to the left L5 nerve root. It cannot be determined whether this represents a calcification, an osteophyte, or a small sequestrated fragment. Diagnosis: Mild protrusion of the intervertebral disks of the lower three segments, most pronounced at L4-5. Conservative treatment was provided, with stabilizing physical therapy and positioning to flatten the lumbar lordosis. Facet joint infiltration and epidural infiltration may be indicated if the left L5 radicular symptoms persist. Segments L3-4, L4-5, and L5-S1 showed obvious degenerative changes in the form of “black intervertebral disks,” in addition to other signs of degenerative disk disease. The subsidence of the L4-5 and L5-S1 intervertebral spaces, in particular, gave rise to a facet joint syndrome. The circumscribed area of hypointensity medial to the left L5 nerve root (c2, →),whether it represents an osteophyte or a calcified sequestrated fragment, may be responsible for the radicular symptoms. Surgical correction was not recommended as postoperative scarring would probably have worsened the patient’s symptoms. Spinal fusion at L4-5 was also contraindicated, for the following reasons: 1 The symptoms were only moderately severe. 2 The adjacent L3-4 and L5-S1 intervertebral disks were markedly degenerated and might have be come increasingly symptomatic after fusion at L4-5. Fig. 2.26a Fig. 2.26b Fig. 2.26c1
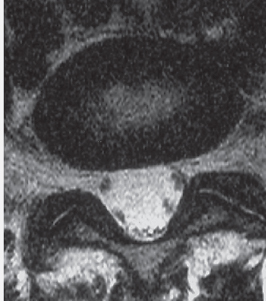
Case Study 1: Normal Findings
Clinical Presentation
MRI
b T1 SE, sagittal, median,
c T2 TSE, axial, L3-4 (c1) and L5-S1 (c2).
Treatment Rendered


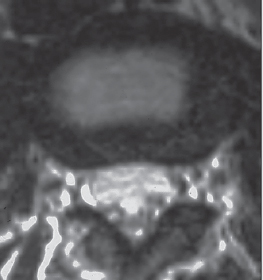
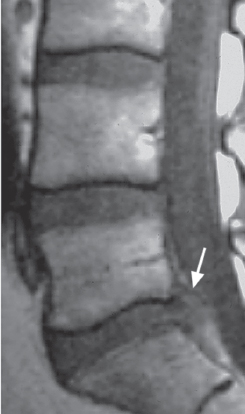
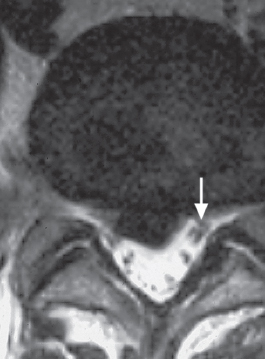
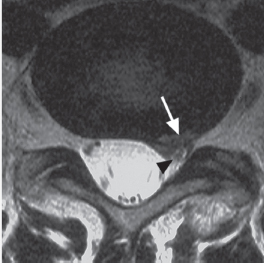
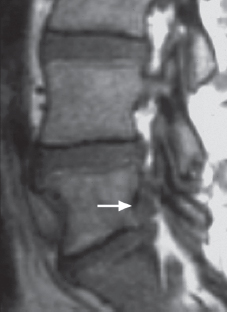
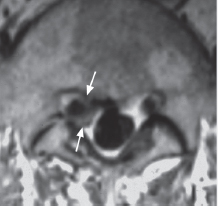
Case Study 2: Monosegmental Degenerative Disk Disease
Clinical Presentation
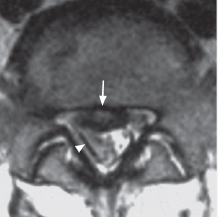
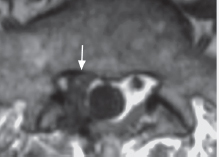
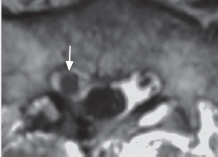
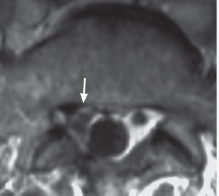
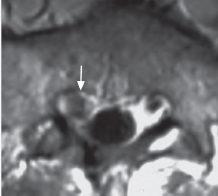
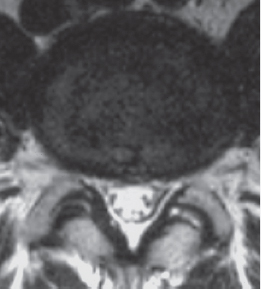
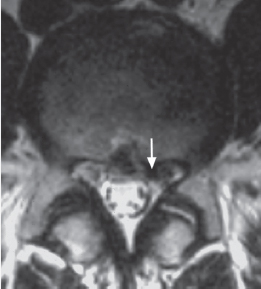
MRI
b T1 SE, sagittal, median,
c T2 TSE, axial, L3-4 (c1) and L5-S1 (c2).
Clinical Course
Comments


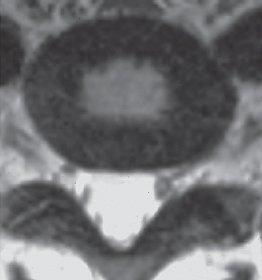
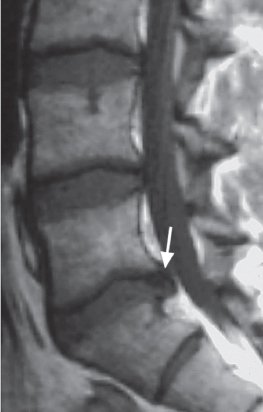
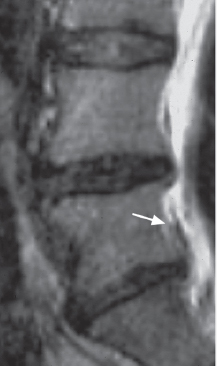
Case Study 3: Protrusions in Segmental Degenerative Disk Disease
Clinical Presentation
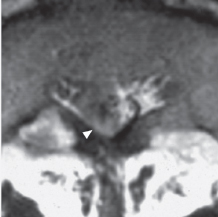
MRI
b T1 SE, sagittal, paramedian,
c T2 TSE, axial, L4-5 (c1) and L5-S1 (c2).
Treatment Rendered
Clinical Course
Comments
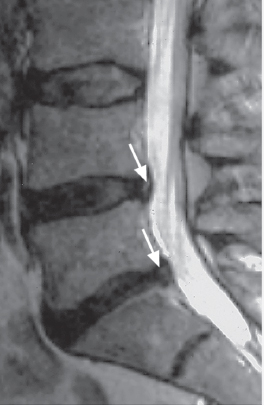


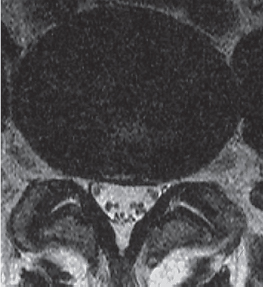
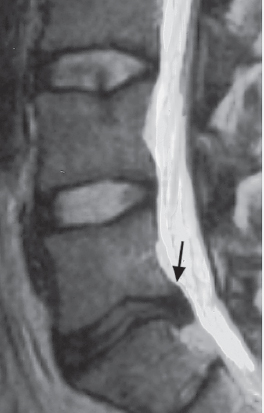
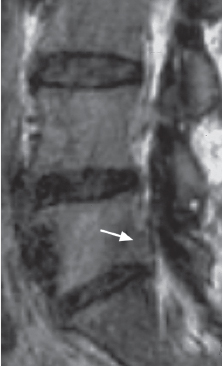
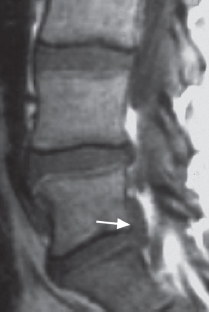
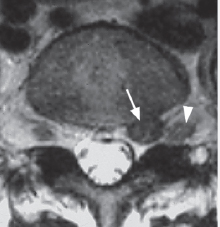
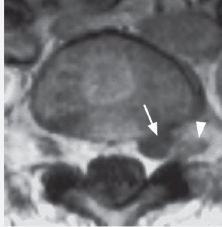
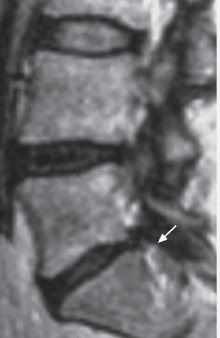
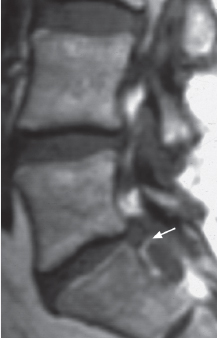
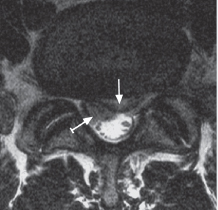
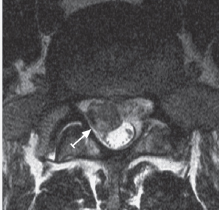
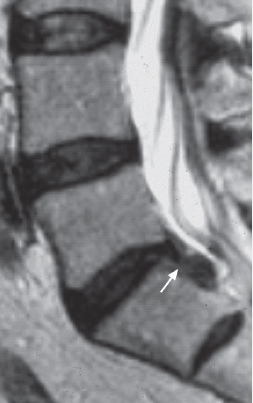
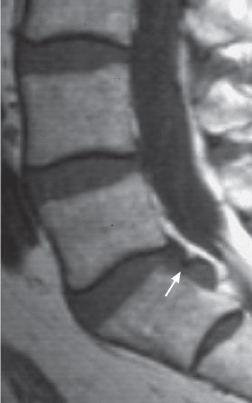
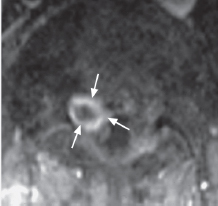
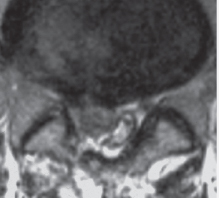
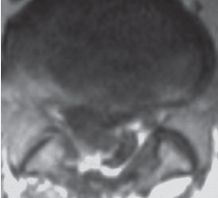
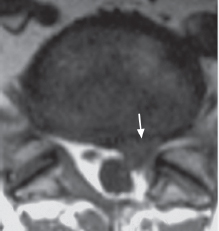
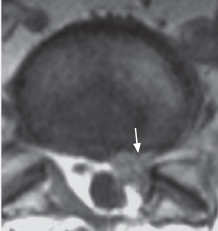
Case Study 4: L5-S1, Protrusion or Extrusion
Clinical Presentation
MRI
b T1 SE, sagittal, median,
c T2 TSE, axial, L5-S1.
Treatment Rendered
Clinical Course
Comments


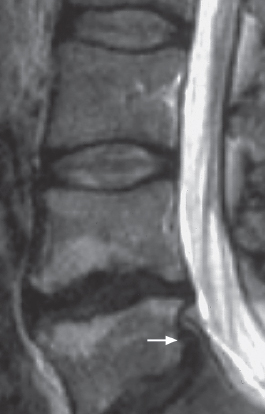
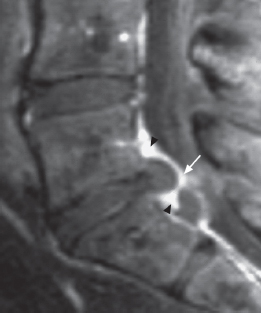
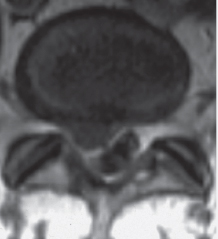
Case Study 5: L5-S1, Protrusion and Extrusion
Clinical Presentation
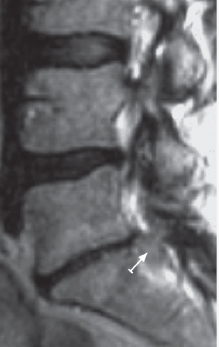
MRI
b T1 SE, sagittal, left paramedian/paramedial (b1) and left paramedial/lateral (b2),
c T2 TSE, axial, L5-S1 (c1) and superior end plate (c2).
 ). The left S1 nerve root is thickened (a, b, c2, →).
). The left S1 nerve root is thickened (a, b, c2, →).
Treatment Rendered
Clinical Course
Comments



Case Study 6: L5-S1, Extrusion at the Disk Level
Clinical Presentation
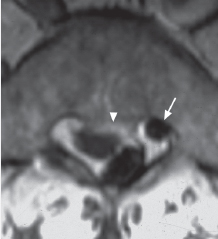
MRI
b T1 SE, sagittal, left paramedial,
c T2 TSE, axial, L5-S1,
d T1 TSE, axial, L5-S1.
Treatment Rendered
Operative Findings
Histological Findings
Postoperative Course
Follow-up Examination
Comments


Case Study 7: L5-S1, Extrusion at the Disk Level
Clinical Presentation
MRI
b T1 SE, sagittal, median,
c T2 TSE, axial, L5-S1.
Treatment Rendered
Clinical Course
Comments
Case Study 8: L5-S1, Extrusion at the Disk Level
Clinical Presentation
MRI
b T1 SE, sagittal, right paramedian,
c FLASH 2-D, sagittal, median,
d T1 SE, axial, S1 superior end plate.
 ).
).
Treatment Rendered
Operative Findings
Comments
Case Study 9: L5-S1, Extrusion at the Disk Level
Clinical Presentation
MRI
b T1 SE, sagittal, left paramedial,
c T2 TSE, axial, L5 inferior end plate (c1) and L5-S1 (c2).
 ), with marked narrowing of the superior portion of the left S1 lateral recess. The facet joints (c) exhibit degeneration.
), with marked narrowing of the superior portion of the left S1 lateral recess. The facet joints (c) exhibit degeneration.
Treatment Rendered
Clinical Course
Comments

Case Study 10: L5-S1, Extrusion with Supradiskal Extension
Clinical Presentation
Electromyography
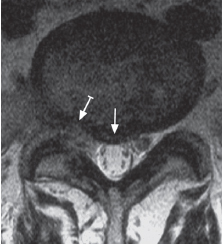
MRI
b T1 SE, sagittal, left paramedian (b1) and left lateral (b2),
c T2 TSE, axial, L5-S1,
d T1 SE, axial, L5-S1 with i. v. injection of gadolinium.
 ), which appears slightly swollen (c, d). No significant scarring is present from the prior disk surgery on the right side at L5-S1.
), which appears slightly swollen (c, d). No significant scarring is present from the prior disk surgery on the right side at L5-S1.
Treatment Rendered
Operative Findings
Postoperative Course
Comments
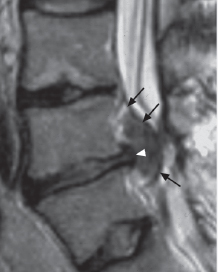
Case Study 11: L5-S1, Extrusion with Supradiskal Extension Associated with Spondylolisthesis
Clinical Presentation
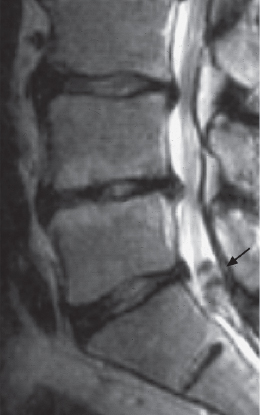
MRI
b T1 SE, sagittal, left paramedian,
c T1 SE, sagittal, left paramedial/lateral,
d T2 TSE, axial, cranial third of the L5 vertebral body.
 ).
).
Treatment Rendered
Operative Findings
Clinical Course
Comments

Case Study 12: L5-S1, Extrusion with Infradiskal Extension
Clinical Presentation
MRI
b T1 SE, axial, L5-S1 (b1) and S1 superior end plate (b2).
c T2 TSE, axial, L5-S1 at S1 superior end plate.
d T2 TSE, sagittal, median. Images b-d were obtained three years later.
Clinical Course
Comments




Case Study 13: L5-S1, Extrusion with Infradiskal Extension
Clinical Presentation
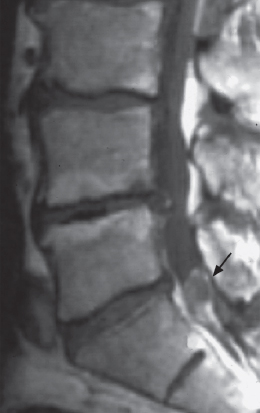
MRI
b T1 SE, sagittal, right paramedial,
c T1 SE, sagittal, median, fat-saturated with i. v. injection of gadolinium,
d T1 SE, axial, L5-S1 (d1) and cranial third of S1 vertebra (d2) with i. v. injection of gadolinium.
Treatment Rendered
Operative Findings
Clinical Course
Comments
Case Study 14: L5-S1, Extrusion with Infradiskal Extension
Clinical Presentation
MRI
b T1 SE, sagittal, right paramedian,
c T2 TSE, axial, S1,
d T1 SE, coronal.
Treatment Rendered
Operative Findings
Histological Findings
Postoperative Course
Comments
Case Study 15: L5-S1, Extrusion with Infradiskal Extension
Clinical Presentation
MRI
b T1 SE, sagittal, right paramedial (b1), and left paramedial (b2).
c T2 TSE, axial, L5-S1 (c1) and at S1 superior end plate (c2).
Treatment Rendered
Operative Findings
Histological Findings
Postoperative Course
Comments

Case Study 16: L5-S1, Extrusion with Infradiskal Extension
Clinical Presentation
MRI
b T1 SE, sagittal, median,
c T2 TSE, axial,
d FISP 3D, MIP reconstruction.
 ) and cannot be clearly distinguished from the extrusion (P) in the MR myelogram. The arrow indicates the left S1 nerve root (c).
) and cannot be clearly distinguished from the extrusion (P) in the MR myelogram. The arrow indicates the left S1 nerve root (c).
Treatment Rendered
Operative Findings
Histological Findings
Clinical Course
Comments
Case Study 17: L5-S1, Extrusion with Infradiskal Extension and Cauda Equina Syndrome
Clinical Presentation
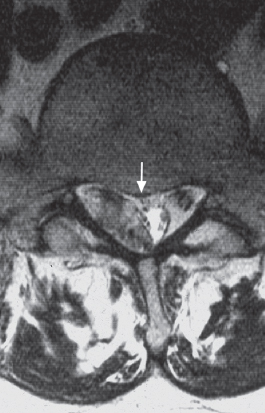
MRI
b T1 SE, sagittal, paramedian,
c T2 TSE, axial, L5-S1 (c1) and at S1 superior end plate (c2),
d T1 SE, axial, L5-S1 (d1) and at S1 superior end plate (d2).
 ), extending inferiorly as far as the rudimentary S1-2 intervertebral disk. The left S1 nerve root is markedly displaced and, in some images, poorly visualized (c, d). The truncated arrow indicates the right S1 nerve root (d2).
), extending inferiorly as far as the rudimentary S1-2 intervertebral disk. The left S1 nerve root is markedly displaced and, in some images, poorly visualized (c, d). The truncated arrow indicates the right S1 nerve root (d2).
Treatment Rendered
Operative Findings
Postoperative Course
Comments


Case Study 18: L5-S1, Extrusion with Infradiskal Extension and Possible Intradural Migration
Clinical Presentation
MRI
b T1 SE, sagittal, median,
c T2 TSE, axial at the superior end plate of S1 (c1) and at the middle third of S1 (c2),
d T1 SE, coronal.
 ). Part of the right margin of the dural sac cannot be clearly identified (c2). The extrusion (P) compresses the dural sac considerably at the entire S1 level, down to the level of the rudimentary disk at S1-2 (d).
). Part of the right margin of the dural sac cannot be clearly identified (c2). The extrusion (P) compresses the dural sac considerably at the entire S1 level, down to the level of the rudimentary disk at S1-2 (d).
Treatment Rendered
Operative Findings
Clinical Course
Comments

Case Study 19: L5-S1, after Previous Surgery
Clinical Presentation
MRI
b T1 SE, sagittal, right paramedial,
c T2 TSE, axial, L5-S1,
d T1 TSE, axial, S1 superior end plate,
e T1 TSE, axial, S1 superior end plate with i. v. injection of gadolinium.
Treatment Rendered
Clinical Course
Comments

Case Study 20: L5-S1, after Previous Surgery
Clinical Presentation
MRI
b,g T1 SE, sagittal, paramedian,
c,h, T2 TSE, axial, L5-S1,
d,i T1 TSE, axial, L5-S1 with i. v. injection of gadolinium (i),
e T1 SE, axial, L5-S1 with i. v. injection of gadolinium, fat-saturated (e2).
 ), although it is not clear whether this represents a transligamentous sequestrum; the posterior longitudinal ligament is displaced and apparently intact (f, →).
), although it is not clear whether this represents a transligamentous sequestrum; the posterior longitudinal ligament is displaced and apparently intact (f, →).
Treatment Rendered
Operative Findings
Clinical Course
Comments


Case Study 21: L5-S1, after Previous Surgery
Clinical Presentation
MRI
b T1 SE, sagittal, left paramedian (b1) and left paramedial (b2),
c T1 SE, axial, L5-S1 before (c1) and after (c2) i. v. injection of gadolinium,
d T1 SE, axial, S1.
Treatment Rendered
Clinical Course
Comments




Case Study 22: L5-S1, after Previous Surgery
Clinical Presentation
MRI
b T1 SE, sagittal, right paramedial,
c T2 TSE, axial, L5-S1 infradiskal level,
d T1 SE, axial, L5-S1 infradiskal level, plain scan,
e T1 SE, axial, L5-S1 infradiskal level with i. v. injection of gadolinium.
Treatment Rendered
Clinical Course
Comments

Case Study 23: L5-S1, Synovial Cyst
Clinical Presentation
MRI
b T1 SE, sagittal, right paramedial,
c T2 TSE, axial infrapedicular slice of L5 vertebra,
d T1 SE, axial inferior end plate of L5 vertebra (d1) and pedicle (d2),
e T1 SE, axial infrapedicular slice of L5 vertebra with i. v. injection of gadolinium, fat saturated.
 ) is normal. There is no enhancement after gadolinium injection (e). A hypo-plastic intervertebral disk is seen at S1-S2 (a, b,
) is normal. There is no enhancement after gadolinium injection (e). A hypo-plastic intervertebral disk is seen at S1-S2 (a, b,  ).
).
Treatment Rendered
Operative Findings
Clinical Course
Comments


Case Study 24: L4-L5, Protrusion and Degenerative Disk Disease, Possibly Accompanied by Spondylodiscitis
Clinical Presentation
MRI
b T1 SE, sagittal.
Treatment Rendered
Comments


Case Study 25: L4-5, Erosive Osteochondrosis
Clinical Presentation
MRI
b T1 SE, sagittal, median,
c T1 SE, sagittal, median, fat-saturated with i. v. injection of gadolinium,
d T1 SE, axial, L4-5 before (d1) and after (d2) i. v. injection of gadolinium.
Treatment Rendered
Clinical Course
Comments



Case Study 26: L4-5, Protrusion
Clinical Presentation
MRI
b T1 SE, sagittal, median,
c T2 TSE, axial, L4-5 (c1) and superior end plate of vertebra L5 (c2).
Treatment Rendered
Comments
Case Study 27: L4-5, Protrusion and Annular Tear
Clinical Presentation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree