Key Points
- ▪
Contrast-enhanced CT scanning is well suited to imaging congenital anatomic variants of the cavae as well as caval pathologies, including caval thrombi, tumors, obstructions, and occlusions.
- ▪
Congenital variants of the cava are not uncommon and may be complex.
The cavae are large vessels with near-vertical orientation, which makes them particularly accessible for assessment by all manner of contrast-enhanced CT examinations, such as axial source imaging, as well as sagittal and coronal projections.
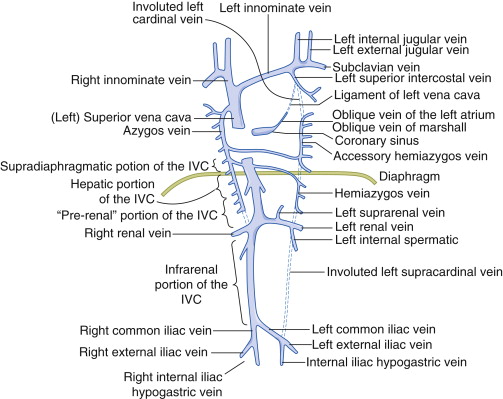
In addition to being diseased, both the superior (SVC) and inferior (IVC) venae cavae have congenital variants that are regularly encountered and that have clinical relevance. Familiarity with the congenital variants of IVC is important so as not to misinterpret them as adenopathy or other structures on cross-sectional imaging, particularly when the degree of venous opacification is poor. Venous anomalies often are dilated and may be tortuous, increasing the risk of surgical injury and bleeding. Preoperative identification of anomalies allows for better surgical planning and may avoid potentially disastrous errors.
Anatomy Of the Superior Vena Cava
The SVC (or precava) returns deoxygenated blood from the upper half of the body to the right atrium. Its proximal aspect is the union of the left and right brachiocephalic veins; its distal aspect is the union with the superomedial aspect of the right atrium ( Fig. 29-1 ).
Branches and Tributaries of the Superior Vena Cava
- □
Left brachiocephalic (innominate) vein
- •
Left subclavian vein
- •
Left internal jugular vein
- •
Left superior intercostal vein
- •
- □
Right brachiocephalic (innominate) vein
- •
Right subclavian vein
- •
Right internal jugular vein
- •
- □
Azygos vein
- •
Hemiazygos vein
- •
Accessory hemiazygos vein
- •
Congenital Variants
Persistent Left Superior Vena Cava
See Figures 29-2 through 29-6 ;
- □
Incidence:
- •
Isolated: 0.3% to 0.5%
- •
Presence of congenital heart disease: 3% to 10%
- •
- □
Results from failure of involution of the left cardinal vein
- □
The right SVC is absent in 30% of cases.
- □
The left SVC usually drains into the coronary sinus, which is dilated. Rarely, the left SVC may drain into the left atrium.
- □
Clinical relevance:
- •
Association with congenital heart disease
- •
May confer difficulty in catheterizing the right heart, in placement of pacemakers or implantable cardioverter defibrillators
- •
Alters the technique of placing the heart on bypass
- •





Double Superior Vena Cava
- □
Incidence:
- •
Isolated: 0.3%
- •
Presence of congenital heart disease: 11%
- •
Superior Vena Cava Agenesis and Drainage into the Inferior Vena Cava via the Azygos Vein
- □
Total absence of the SVC
- □
Due to lack of development of the right anterior cardinal vein
- □
The azygos vein is dilated and carries blood posterior to the diaphragm to the IVC.
- □
Incidence: rare
Superior Vena Cava Obstruction/Superior Vena Cava Syndrome
Caval obstruction may be partial or complete (occlusion) and may result from any combination of extrinsic compression, intramural scarring, and intraluminal thrombosis or other mass lesion. Etiologies are diverse and include:
- □
Extrinsic compression:
- •
By tumor: 90% of cases of SVC syndrome are due to malignant compression of the SVC, especially by:
- •
Bronchogenic carcinoma
- •
Lymphomas
- •
Breast carcinoma
- •
- •
By ascending aortic aneurysms
- •
Syphilis
- •
Tuberculosis
- •
- •
- □
Iatrogenic intraluminal thrombosis due to instrumentation of the SVC
Superior Vena Cava Stenosis
Caval stenosis is evident on contrast-enhanced CT scanning by focal narrowing and proximal venous engorgement, with or without venous collateral formation.
SVC Occlusion
SVC occlusion is evident on contrast-enhanced CT scanning by the absence of contrast enhancement within the cava. CT is able to image structures near the cava and elsewhere inside the body that may explain or suggest the cause of the obstruction. Proximal venous distention is usual. The presence of collateral vessels indicates chronicity.
Intraluminal Thrombus Versus Tumor Mass
Distinguishing thrombosis from tumor (angio) invasion may be possible and requires finding the origin of the soft tissue caval intraluminal mass. Chronic thrombosis organizes and usually contracts the cava, whereas acute thrombosis distends the cava. Indwelling lines, pacemaker wires, and implantable cardioverter defibrillator leads that are the source of thrombosis confer artifacts. Streaming artifacts from the contralateral venous drainage, and also from the azygos vein, may make it difficult to confirm thrombosis. ( Figs. 29-7 through 29-9 ; ).