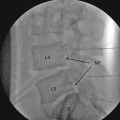
Fig. 25.1
Quieting dorsal nerve roots – alcohol and phenol
There are arguments for and against administration of a test dose. It is difficult to make local anesthetic as hypobaric as alcohol to determine accurately the behavior of the proposed alcohol injection. A small dose of lidocaine can be used to minimize the burning and unpleasant sensation associated with alcohol injection, but this will prevent the use of the symptoms of burning after alcohol injection as a valuable indicator of the particular segments which are going to be involved. Alcohol should be injected in 0.1-ml increments from a tuberculin syringe to ensure accuracy of volume administered. The patient should be asked to report the development of any burning sensation after each aliquot of injection and the location of such burning. The presence of a burning sensation at the painful area gives a strong indication that the injected drug has reached the corresponding site. The maximum injected volume required to produce the beneficial effect is usually 1 ml. If the patient indicates a burning sensation just cephalad or caudal to the original area of pain, the table can be tilted head up or down to modify the spread of neurolytic agent. However, if the unpleasant sensation is perceived distant from the painful areas, the spinal needle should be withdrawn and reinserted at a level below or above the initial site of injection as directed by the patient’s perception of dysesthesia relative to the site of pain.
The needle should be flushed free of the alcohol or phenol with 0.2–0.3 ml of preservative-free normal saline or CSF before its withdrawal in order to avoid spilling of the drug in the subcutaneous tissue. Injection of 0.1–0.2 ml of neurolytic drug at a discordant site is associated with minimal demonstrable neurological damage. Constant communication and feedback from the patient is crucial to the success of the procedure and can greatly prevent unintentional neurologic deficits from occurring. If pain is present covering three or four segments, separate injections should be made at each level, observing the above precautions with each injection.
Phenol Neurolysis
As phenol is hyperbaric, the patient should be positioned with his/her painful side in a dependent position with slight posterior tilt to the torso so as to direct the solution to the posterior rootlets (Fig. 25.1). In patients with sacral pain, this procedure can be done in sitting position. Phenol is a viscous solution necessitating a larger bore needle to perform this procedure. Warming the phenol by immersing the ampoule in hot water prior to aspiration into the syringe reduces the viscosity and makes it easier to inject. The bevel of the needle should be directed inferiorly. Extreme care should be taken to minimize the likelihood of splashing phenol by creating a firm seal between the syringe and hub of the needle. Otherwise, due to the extreme viscous nature of the solution and subsequent increased pressure to inject the solution, the seal can break and the phenol solution can splash onto intact skin of the patient or even into the eyes of the clinician. Unlike alcohol, phenol does not produce any burning sensation during injection. It actually produces relatively mild warmth and tingling due to its local anesthetic properties. After the injection, the stylet should be replaced into the needle and the needle tip washed by the CSF to minimize the potential for sinus formation and backache due to the escape of residual drug as the needle is withdrawn.
Neurolysis is less common in the cervical region due to several factors. Compactness of the spinal cord and nerve roots make it difficult to perform a selective block. The compactness of neural elements in the cervical region makes selective neurolysis of sensory nerve roots more challenging to accomplish without causing unwanted adverse effects. Moreover, since the brachial plexus is in the cervical region, these adverse effects can be quite troublesome. In cases where the brachial plexus itself is involved in the pain syndrome, it may be a neuropathic rather than a somatic type of pain and therefore often resistant to successful treatment with subarachnoid neurolysis. Subarachnoid neurolysis for pain in the thoracic region is very effective but technically challenging compared to performance in the lumbosacral region due to the presence of the spinal cord. However, the consequences of motor dysfunction are less pronounced in the thoracic area, and paralyses of intercostal muscles usually are well tolerated. Intrathecal neurolysis in the lumbosacral region can be very effective for pain in the pelvic, perineal, rectal, and genital area, especially when it has been refractory to traditional therapeutic options.
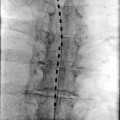
A subarachnoid catheter technique has also been reported for use in neurolysis of selective thoracic posterior nerve roots for provision of analgesia in patients with lung cancer and pain [22]. The advantage of the catheter technique is simplicity and avoidance of multiple injections. A 19-G radiopaque catheter was inserted into the subarachnoid space through a 17-G Tuohy needle and was guided fluoroscopically cephalad to the spinal segment where analgesia was desired. After confirming the placement of the subarachnoid catheter, 0.4 ml of alcohol was injected at each level as the catheter was withdrawn slowly. Alcohol was injected at each level to produce the desired effect until a predetermined inferior level to be blocked was achieved.
Epidural Neurolytic Block
Despite the fact that epidural injection and catheter placement is a commonly performed technique, epidural neurolysis has been very disappointing in its results, probably because of reduced contact of neurolytic agent with the nerve roots due to the dural barrier. The potential for alcohol neuritis and disastrous complications of inadvertent intrathecal injection have made this technique less popular. This technique has been reported as early as 1940 for the treatment of pain due to general carcinomatosis. Nevertheless, there is less risk of bladder and bowel dysfunction with this approach. Solutions can be injected in an incremental fashion daily until the desired effect is obtained. CT scan or MRI should be performed prior to initiation of the procedure to rule out the presence of epidural tumor which could bleed during epidural needle placement. Uncontrolled bleeding, especially with tumor invasion and neovascularization, can lead to epidural or spinal hematoma.
Epidural neurolysis is more useful for midline and bilateral pain, as gravity plays little role in the spread of alcohol and phenol in the epidural space. Epidural administration is more preferable over the subarachnoid technique in patients with extensive topographic distribution of pain. Intracranial spread and meningeal irritation are uncommon. Overnight stay in the hospital may be required to titrate the injection to desired therapeutic effect given the need for multiple injections and titration to desired effect [23]. Use of at least a 20-G epidural catheter is required to allow for the injection of highly viscous phenol solutions in the epidural space. The suggested dosages are 0.5–5.0 ml, starting with the lower dosage. Confirmation of the site of injection and spread of medications with fluoroscopy and radiopaque contrast dye is highly desirable [24]. Fluoroscopy confirmation of the tip should be performed for every additional injection. Butamben has been successfully used via the epidural route for the treatment of both malignant and nonmalignant pain [25].
Although subdural neurolysis has been described in the older literature, particularly in the cervical region, due to technical difficulties and unpredictable distribution of drugs in the space, it is not used.
Efficacy
Patient selection and meticulous procedural technique are essential for the success of neuraxial neurolysis. Often, incomplete analgesia results, and therefore, patients should be informed realistically about reasonable expectations from the procedure. It is difficult to compare results of various studies, as the site of injection, choice of drug, presence and growth of tumor, and definition of pain relief vary between different investigations. The success rate of subarachnoid neurolysis is slightly better with alcohol than of that with phenol, and complications are slightly higher with phenol than with alcohol [11, 15, 26, 27]. Table 25.1 illustrates the complications from two different types of neurolytic agents although there are no randomized studies. Phenol has been reported to give moderate to excellent pain relief in at least 50 % of the patients for at least a month.
Table 25.1
Comparison of reported complications due to intrathecal phenol or intrathecal alcohol
Neurolytic agent | Phenol (n = 704) (%) | Alcohol (n = 704) (%) |
|---|---|---|
Bladder dysfunction | 9.0 | 3.5 |
Rectal sphincter dysfunction | 2.0 | 0.0 |
Headache | 3.0 | 0.0 |
Paresis | 12.9 | 3.9 |
Dysesthesia | 8.0 | 3.8 |
Follow-up Care
Follow-up care is essential and obligatory following neuraxial neurolytic blockade. The aim of the post-procedural examination is to assess the efficacy of the block, taper systematically the dosage of systemic analgesic medications, and to address any adverse effects which may have occurred.
Functional pain scores and activity levels should be monitored. It can take up to a week for the patient to sense and appreciate the complete efficacy of the block. Hence, a 1-week follow-up is necessary to determine if there are any unblocked segments and to discuss the requirement of an additional procedure. Systemic opioid dose should be reduced gradually to avoid precipitation of any withdrawal symptoms. A suggested plan would be to reduce the dosage by a quarter to a third every week [28]. This reduction in opioid dosage may help minimize systemic opioid side effects and avoid sedation. This follow-up opportunity may also be utilized to identify adverse effects and institute appropriate rehabilitation as necessary.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree