where V is voltage, I is current, and R is impedance.
CRF involves controlled administration of alternating current electrical energy at 500 kHz (kilocycle/s) range. Current is utilized at the kilocycle Hz range, as alternating current (AC) at a lower frequency would be very painful in clinical use [6]. Direct current is not utilized in this radiofrequency technology as the frequency of this energy is zero and would lead to less precision during lesion formation.
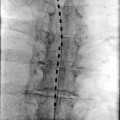
The setup of a radiofrequency circuit [4–6] involves a generator to produce and drive the energy, a dispersive pad (grounding plate) to return energy to the generator, an insulated introducer needle to prevent dispersal of energy outside of the targeted area, and an electrode with a thermocouple to provide a precise area of therapy and temperature measurement.
The description of the electrical field that is responsible for the clinical effect of CRF is governed by Maxwell’s equations on electromagnetism [4]. At the frequencies utilized in RF technology, electrical and magnetic fields are generated; however, the magnetic field’s effect is negligible [7]. The current density that is responsible for clinical effect is a function of the electrical conductivity of tissue [8]. Structures that readily conduct electrical energy such as nervous tissue and water will have higher current density than those structures with a lower conductivity (bone). Also, the coagulated tissue that is produced during CRF may serve to affect impedance as the resultant tissue may decrease the flow of energy into tissues.
As energy flows from the generator via electrical current to the electrode, ions in tissue electrolytes are activated and oscillated [6–8]. As a result of the kinetic energy produced by this Brownian motion, heat is dispersed from the ions and is measured by the thermocouple. Increasing the flow of current will increase the resultant temperature, known as ohmic or resistive heating of tissue, as measured at the thermocouple. In summary, the tissue heats up the electrode, and the electrode does not heat up the tissue.
Temperatures utilized typically range from 80 to 90 °C, although the minimum temperature to produce irreversible neuronal interruption is 44 °C [9]. Higher temperatures may lead to side effects including hematoma, smoke, and gas formation, along with adherence to tissues to the probe [9]. Nociceptive input is theoretically reduced as the therapy is aimed for sensory nerve fibers.
Utilizing a temperature-time controlled process, a lesion is produced with treatment. Precision in lesions developed with the introduction of a 22-G RF cannula, smaller than previous devices [10]. The size of the lesion is affected by factors including the diameter of the electrode, the active tip length, tissue characteristics, and vascular supply near the lesion site. The lesion size and tissue injury can be evaluated through the relation between the current divided by the electrode surface area known as the current density. For a given constant current, with a decrease in electrode surface area, a greater current density, tissue heating and resultant lesioning will occur.
Power [11] provided by the generator, along with lesion time, also affects lesion size. Lesion time has been found to be significant in increasing the size of the heat effect up to 40 s. The temperature at the thermocouple along with the cannula size is an important factor in the size of the lesion, as heat generated in the process believed to be responsible for the clinical effects of radiofrequency.
Due to the shape of the needle and the electrode, an oblate spheroid lesion is produced [6, 8, 9, 11]. A temperature-controlled system is preferred over a voltage-controlled system as lesion size and temperature achieved can more reliably result, leading to a more predictable lesion. Voltage-controlled lesioning may produce temperatures below or above target range, leading to lesions of variable efficacy [9].
Physics of Pulsed Radiofrequency
Pulsed radiofrequency differs from CRF in that pulsed radiofrequency does not lead to a neurodestructive process [3, 4]. This theoretical benefit is important for sensitive nerves such as peripheral nerves in the head and neck, dorsal root ganglia, trigeminal ganglia, and peripheral nerves in the abdominal and inguinal regions [12, 13], and the lower extremity.
During the developmental phases of what is now known to be pulsed radiofrequency, interest was sought for the possible beneficial role of the magnetic field in treatment. Cosman et al. [14] determined that the magnetic component was an incidental vector that would have negligible effects toward clinical benefit [7]. It was then proposed to deliver energy in waves or pulses with a short rest period between generator activation. This rest period would allow the dispersal of the heat that was generated (as in CRF). This interrupted treatment would theoretically deliver electrical energy to elicit a clinical response, but not lead to the side effects of denervation and its resultant complications. In the initial description by Sluijter et al. [14], the pulses were for 20 ms separated by 0.5 s. This separation allowed for a rest period whereby heat that is generated by oscillatory motion would be allowed to dissipate via vascular runoff. Still, this treatment should not be thought of as a “nonthermal” lesion as there is increased temperature at the thermocouple. Consequently, as the pulse duration is a fraction of total pulse time (pulse duration + interpulse duration), voltage utilized during PRF is higher without risking increased temperature change with the higher energy.
PRF technology, however, may also lead to lesion injury. Heavner et al. [15] however showed that when PRF is utilized (10 ms duration at 2 Hz), coagulation begins to occur in egg-white media at a temperature of 60 °C. Therefore, regardless of technology, PRF vs. CRF, increased temperature at the tip can lead to coagulation and tissue injury. In essence, PRF as is currently used is a neuromodulatory treatment option as opposed to the ablative CRF.
The exact mechanism of PRF’s clinical benefit is unclear; initially, PRF was believed to play a role in causing neuronal plasticity with upregulating of c-Fos [16] in rat DRG. c-Fos is a proto-oncogene that is expressed in response to neuronal activity and may have a role in nociceptive transmission. Animals were exposed to RF at the C6 dorsal root ganglion, via CRF at or PRF, at 38 °C for 120 s. Immunohistochemical assays for c-Fos were performed, and animals with PRF had an increased expression of the protein in laminae I and II of the spinal cord; this expression was not seen in animals exposed to CRF.
Additionally, c-Fos staining cells were found ipsilateral and contralateral to the side of PRF treatment. The implication of this finding is that PRF activates the dorsal horn laminae I and II neurons and could be a possible explanation for the clinical benefit of PRF, as both CRF and PRF animals were subject to the same temperature. This choice to have the temperatures of both CRF and PRF by the authors in the experimental design of this study leads to the possibility of deducing that a factor intrinsic to PRF not seen in CRF would lead to c-Fos expression.
This c-Fos selectivity for PRF-treated animals was subsequently refuted in a study by Van Zundert et al. [17] where sham, PRF, and continuous RF were applied adjacent to the cervical DRG of rats. All three groups had induction of c-Fos with staining that was noted 7 days after treatment study. Additional research is warranted regarding the genetic changes that may result and be responsible for the clinical effect of PRF.
Cahana et al. [18] evaluated in vitro neuronal preparations to determine tissue effects of CRF at 42 ° C versus PRF at 38 and 42 °C. The electrical energy required in CRF was less than that in PRF, yet CRF was found to be a destructive lesion in which heat was generated, with PRF specimens showing less tissue injury [18].
Cosman and Cosman [6] have opined that the heat produced with the pulsed energy may be responsible for the clinical benefit of PRF. This heat is subsequently removed during the rest phase, however. Additionally, they suggest that electroporation may be a factor in leading to the clinical effect of PRF. This concept is the alteration in electrical conductance and membrane permeability of a cell membrane in response to an applied electrical field, theoretically leading to analgesic benefit after PRF.
Hagiwara et al. [19] have opined that the analgesic action of PRF involves the action of the accessory adrenergic pain pathways. Hamann et al. [20] have looked at the possible mechanism of PRF and suggest that PRF targets neurons with small diameter axons by evaluating the role of activating transcription factor 3 (ATF-3), a marker of cellular stress, in rats. DRG application of PRF led to an increased presence of ATF-3 in neurons. The authors suggest that PRF can lead to increased cell stress in the absence of direct thermal lesioning. The role of this factor and others in regards to PRF is yet to be fully elucidated.
A proteomic study [21] has also been performed in rats to look at protein expression in animals treated with PRF. L5 dorsal root ganglia were exposed to PRF and sham therapy. Western blotting of samples showed increased levels of gamma-aminobutyric acid (GABA) and decreased 4-aminobutyrate aminotransferase (enzyme involved in production of GABA) in animals treated with PRF. GABA is a neurotransmitter regulating neuronal excitability. Further studies are warranted in exploring the role of PRF on GABA [22, 23].
Histological Effects of Radiofrequency
Animal studies have been performed evaluating the histological effects of CRF therapy. In a study involving CRF of goat (DRG), de Louw et al. [24] found that a temperature of 67 °C at the DRG can lead to hemorrhagic loss of myelinated fibers. This neural destruction is absent if the CRF is performed adjacent to the DRG. Consequently, the heat lesion leads to neuronal injury after a radiofrequency procedure. Animal research has led to the theory that CRF was a selective lesioning modality, preferentially targeting C and A-δ fibers occurred before affecting the larger myelinated A-α and A-β fibers. Other studies have contradicted this result, and CRF is now widely thought of as leading to heat-induced equal destruction of all nerve fibers. Dreyfuss et al. [25] showed that RF neurotomy is a nonselective treatment that affects and coagulates all nerves as a result of EMG studies [26].
Vatansever et al. [27] compared the effects on the sciatic nerve of male Wistar rats. Five groups were studied: no procedure, sham procedure, 40 °C CRF for 90 s, CRF 80 °C for 90 s, and PRF for 240 s. CRF 40 °C showed the presence of endoneurial edema in the subperineurial and perivascular areas of the nerve. Light microscopy specimen evaluation demonstrated transverse myelin fibers damaged along with separation of the axoplasma. This separation would lead to impaired nerve transmission. Electron microscopy also confirmed alteration of myelin configuration. Additionally, lamellous separation with protrusion of myelin and accumulation of neurofilaments was found, pointing to a diagnosis of neurodegeneration.
CRF 80 °C showed significant endoneurial edema and evidence of Wallerian degeneration. Electron microscopy showed evidence of neurodegeneration, including epineurial thickening, lamellous separation, intra-axonal vacuolization, increased intracellular endoplasmic reticulum, and Schwann cell damage.
PRF demonstrated changes similar to CRF 40, but the severity of lesions was less.
Podhajsky et al. [28] observed effects of 80 °C CRF and 42 °C PRF lesions on rat DRG and sciatic nerves for 2, 7, and 21 days after initial treatment and found similar results. Massive edema in specimens was seen on day 2 with 80 °C treatment. Wallerian degeneration and tissue coagulation were observed on the 7th day after treatment. With 42 °C, edema was also seen on the 2nd day of treatment, but regressed and resolved by the 7th day.
Animal studies were also performed in rabbits [29] to evaluate PRF vs. CRF current on the DRG. Animals were in a PRF, CRF, control, or sham grouping. No changes noted at 2 weeks after treatment under light microscopy. By electron microscopic sections, CRF-DRG specimens showed degenerative changes including evidence of cytoplasmic vacuoles, a large endoplasmic reticulum, mitochondrial degeneration, and the loss of nuclear membrane material. PRF did not show the intensity of these changes, with just the presence of large vacuoles throughout the cytoplasm.
Studies on the Efficacy of Radiofrequency
Trigeminal Neuralgia
CRF has been utilized for patients with trigeminal neuralgia, a devastating neuropathic pain state, often very difficult to treat. Radiofrequency has been shown to be the best option for complete pain relief when compared to other approaches including surgical treatments [30]. Kanpolat et al. [31] performed radiofrequency trigeminal rhizotomy on patients with trigeminal neuralgia, looking at 1,600 patients over a 25-year period. Excellent relief of pain symptoms was noted initially with a decrease of 57.7 % at 5-year follow-up. The number of patients with complete relief after a single procedure decreased to 52.3 % by the time a 10-year follow-up was performed. The study also provided side effects that may be present in patients undergoing an ablative procedure on the gasserian ganglion, highlighting the risks of corneal reflex changes, keratitis, masseter muscle dysfunction, cranial nerve II and VI paralysis, and anesthesia dolorosa. PRF has been evaluated against CRF [32], with the former not as effective as the latter in treating the pain of trigeminal neuralgia.
Cervical Zygapophyseal Joints
The “facets” are in actuality the zygapophyseal joints (z-joints) that are made of adjacent articular processes. The term facet describes the curved cartilaginous lining of the z-joints. The joints are involved in the range of motion of the cervical spine. The zygapophyseal joints in the cervical spine may be implicated in 54–60 % of patients with chronic neck pain [33]. Neural innervation of the joint is provided by medial branches of the spinal nerves with each joint is innervated by the adjacent two medial branches.
After successful block of the joint or the medial branches that supply the joints, radiofrequency treatment can be performed for longer-term benefit of painful symptoms. Cohen et al. [34] have evaluated in a multicenter analysis the factors that predict success for cervical radiofrequency denervation and noted the presence of pre-procedure paraspinal tenderness as the best prognostic sign. Lord et al. [35] evaluated patients with chronic z-joint pain after motor vehicle accident in a double-blinded randomized controlled trial, treated with CRF for analgesic relief. A positive result of 100 % pain relief with three diagnostic/therapeutic blocks with local anesthetic and steroid was required prior to inclusion in the study. Patients had a median time from initial relief to 50 % of pain returning at 263 days.
Sapir et al. [36] evaluated patients with cervical whiplash symptoms undergoing cervical neurolysis. There was a statistical significance in improvement in patients VAS scores regardless of litigation status by patients. Long-term follow-up and benefit was noted of the radiofrequency procedure in a paper by McDonald et al. [37]. The median duration in their study of 28 patients diagnosed as having cervical zygapophyseal joint pain was 219 days. In a Cochrane analysis, Niemisto et al. [38] evaluated the efficacy of cervical radiofrequency and found limited evidence for short-term benefit.
Other Painful Conditions of the Cervical Spine
Slappendel et al. [39] published a report of the results of a randomized, double-blinded multicenter trial on the effect of CRF of the cervical DRG to treat cervicobrachial pain. This study evaluated the difference in temperature between two groups: one population was treated with CRF at 67 °C and the other group at 40 °C. Both patient groups developed a decrease in VAS scores; however, the 40 °C group maintained their decrease at 3-month follow-up. Van Zundert et al. [40] have evaluated PRF in the treatment of cervical radicular pain adjacent to the cervical DRG and found the technique be satisfactory at reducing discomfort for a mean duration of 9 months.
The concept of cervicogenic headache is a controversial topic in pain management circles. Difference of opinion exists between physicians as to whether this entity deserves a diagnosis or not [41].
Multiple papers [41–43] have provided a description of this unilateral headache that is present in the occipital or neck region, radiating to the temporal and/or frontal aspect of the cranium. Stovner et al. [44] have evaluated the use of radiofrequency denervation of facet joints for cervicogenic headache via a double-blinded, sham-controlled randomized double-blinded study. Twelve patients with unilateral cervicogenic headache were evaluated with half randomized to receive C2–C6 neurotomy and the others to receive sham therapy. Patients were followed for 2 years, with improvement noted at 3 months in the treated group. The authors followed patients for 2 years after the initial treatment and found no significant benefit for the use of this technology. Haspeslagh et al. [45] compared the use of radiofrequency of the medial branches supplying the z-joints, the dorsal root ganglion against an injection of local anesthetic at the greater occipital nerve with subsequent application of transcutaneous electrical nerve stimulation. There was no evidence that cervical z-joint radiofrequency was superior to injection of the greater occipital nerve and TENS application. The results of this study may be questioned, however, because of the small sample size (15 patients) and a relatively large number of patient dropouts. Govind et al. [46] have evaluated radiofrequency denervation for headache pain by targeting the third occipital nerve a particularly tenacious nerve. Multiple lesions, larger electrode (greater than 22 G), were utilized for best clinical effect. Untoward side effects such as ataxia, paresthesia, numbness, and dysesthesia may result from this procedure.
Navani et al. [47] presented their report of the use of PRF in a patient with occipital neuralgia. The patient underwent PRF at the medial branches of C1 and C2 dorsal rami with three cycles of 42 °C for 120 s. The patient subsequently underwent another PRF treatment 4 months after initial therapy with improvement of symptoms. As with PRF in other cervical applications, the benefits of treatment as compared to CRF here are evident with less potential risk of neuritis pain induced by heat lesions. Further research is warranted for the use of PRF for this indication.
Thoracic
The thoracic zygapophyseal joints may be a source of discomfort in patients. These joints may be the source of thoracic spine and segmental discomfort in the thoracic region. Stolker et al. [48] evaluated thoracic facet joint CRF and reported benefit of neurolysis. Nearly half of patients were noted to be pain free after 2 months, 83 % of patients achieving greater than 50 % pain relief after 18–54-month follow-up. Cohen et al. [49] evaluated patients who were treated for post-thoractomy pain with PRF of thoracic DRG vs. those patients treated with analgesics or PRF of the intercostal nerves and found that PRF of the DRG was superior.
Lumbar Pain
The lumbar z-joints are also paired, diarthrodial joints that are involved in the range of motion of the lumbar spine. Goldthwait [50] first presented the lumbosacral articulation as a source of low back pain in 1911. After a series of medial branch or z-joint injections, radiofrequency therapy may theoretically improve patient pain for a longer period than the duration of the agents utilized during injection therapies. Cohen et al. [51] also studied the predictors of success for a radiofrequency procedure in the lumbar region and again found paraspinal tenderness to be the most significant predictor of success. Additionally, the degree of pre-radiofrequency analgesia (percent improvement after block) had no effect on post-radiofrequency effect in patients who had at least 50 % pain relief with blocks.
Dreyfuss et al. [25] found that patients with the longest time of relief were those patients who had resultant multifidus muscle denervation based on EMG study after CRF. Nath et al. [52] evaluated patients receiving a positive facet joint injection block who subsequently underwent sham or CRF. Patients who were actively treated had a statistically significant improvement in back and leg pain with improved range of motion, indicating that the beneficial effects noted by patients were not due to placebo effect.
Gallagher et al. [53] evaluated radiofrequency for the z-joints as a treatment for low back pain in a double-blinded prospective study. The visual analog scale (VAS) was utilized to evaluate pain scores and relief after therapy. Patients receiving radiofrequency were compared to sham therapy with VAS was improved at 1 month and 6 months versus sham therapy. Van Kleef et al. [54] also demonstrated the benefit of radiofrequency by studying a group of 31 patients in a prospective double-blind randomized trial. Patients with lumbar facet degeneration after chronic low back pain who had benefit (50 % pain relief) with medial branch blocks underwent CRF vs. sham-treated patients. Test subjects were evaluated 8 weeks after the trial, then at present at 3, 6, and 12 months after initial therapy. There was statistically significant difference between the groups with CRF patients exhibiting lower analgesic requirements and improved disability status vs. patients receiving the sham therapy. The goal of DRG CRF is to perform a selective blockade of afferent nerve conduction with avoidance of damage to the ganglion. Geurts et al. [55] published a multicenter randomized control trial for evaluating lumbar DRG CRF in patients with chronic lumbosacral pain. Patients were evaluated with VAS and also the SF-36 quality of life pain measure. The results of this randomized double-blinded placebo-controlled study were that there was that CRF of lumbar DRG should not be routinely performed as benefit was not seen.
Radiofrequency ablation in the lumbar z-joint region did not have benefit in one study [56]. This placebo-controlled clinical trial resulted in negative recommendation for lumbar radiofrequency ablation. The criticism of this study is that there was a high inclusion rate of patients in this study. Slipman et al. [57] showed that radiofrequency ablation while leading to clinical improvement of pain was rated as having level III evidence based on evidence-based medicine criteria based on review of the literature. Manichikanti et al. [58] performed their own review of the literature that resulted in strong evidence for short-term relief of pain symptoms, but moderate evidence for lumbar radiofrequency for longer-term relief. Kornick et al. reported on complications [59] of lumbar radiofrequency noting that in 116 denervation procedures in 92 patients that no motor or sensory deficits were present in patients. This of course assumes that motor and sensory checks are performed by the operator before the lesioning procedure occurs.
Radiofrequency ablation has had effects for 6 months to a year [4]. In those patients who had repeat radiofrequency procedures, benefit may be achieved with the subsequent procedure. Schofferman and Kine [60] showed in a retrospective chart review of 20 patients who had an initial successful benefit with radiofrequency subsequently developed pain and then had a repeat radiofrequency procedure. Larger needle sizes (20-G electrode with a 10-mm active tip or a 16-G rhizotomy electrode) were utilized. Also, the CRF was 80 °C for 70 s. The mean duration of relief with the repeat RF was 11.6 months for a second RF procedure. Overall, improvement after repeat RF treatments was 10.6 months.
The first use of PRF was described by Sluijter in 1998 [14]. This prospective-controlled trial compared the results of utilizing the new technology with CRF at 42 °C. The authors concluded that PRF was superior to CRF at the parameters used due to a global perceived effect (GPE) that was higher in the former group.
Teixera has suggested the use of lumbar DRG PRF for surgical candidates with radicular pain. PRF DRG was recommended as an alternative to lumbar epidural injections as a treatment option, and 12/13 patients studied were able to avoid surgery for at least 1 year [61].
PRF has also been evaluated for use in patients having pain attributed to the z-joints in the lumbar region. Linder et al. performed a retrospective review [62] of patients undergoing PRF for low back pain. Patients in this study included those having back surgery and those with no history of prior surgical intervention. Prior to CRF, patients had analgesia with one diagnostic medial branch block. The authors found that PRF was beneficial in both patient populations, but more effective in patients who did not have prior back surgery. Mikeladzke et al. [63] evaluated the technology in patients with chronic z-joint pain and found that PRF was beneficial in providing pain relief lasting for almost 4 months.
Kroll et al. [64] performed a randomized double-blinded prospective study comparing CRF vs. PRF in the treatment of chronic z-joint pain. CRF was performed at 80 °C for 75 s and pulsed radiofrequency of 42 C with a pulse duration of 20 ms with a pulse rate of 2 Hz for 120 s. The VAS and the Oswestry Disability Questionnaire were utilized to gauge patient response to treatment at baseline and interval follow-up. There was no significant difference between CRF and PRF in long-term outcome. Additionally, there was greater improvement over time within CRF. A criticism of this study is the large dropout rate of 48 %.
Tekin et al. [65] evaluated the effects of CRF vs. PRF in 40 patients, with an additional 20 patients as control. The VAS and ODI were also utilized for evaluation at procedure, 6-month and 1-year follow-ups. While PRF and CRF patients had improvement in measured parameters, the maintenance of the decrease in VAS was greatest in patients who had CRF as opposed to patients with PRF. The result of therapy was longer lasting in the CRF group.
PRF has also been used in the lumbar region to treat discogenic pain [66]. High-voltage, long-duration PRF has been utilized to treat 8 patients. A 15-cm 20-G needle was placed in the nucleus pulposus for 20 min PRF at 2 × 20 ms at 60 V. The study achieved 100 % improvement of pain on a VAS query. Further controlled studies are mandated for applicability in this domain.
Sacroiliac
The sacroiliac joint may be a common cause of back pain. Goldthwait and Osgood [67] proposed the SI joint to be an independent source of back pain. Estimates of the source of discomfort attributed to the SIJ range from 18 to 30 % [68, 69].
RF ablation of the sacroiliac joint has also been attempted with mixed results. Ferrante et al. [70] published the first description of an RF technique of this pain generator by describing a “leap frog” technique of overlapping bipolar lesions, less than 1 cm apart, along the length of a sacroiliac joint. Lesions were created at 90 °C for 90 s. The distance between lesions was questioned for this bipolar approach [71]. Cohen and others [72, 73] then presented a description of a lateral branch block radiofrequency.
Burnham and Yasui [74] have also described the use of a lateral branch approach for CRF of pain attributed to the SI joint. Nine subjects underwent strip RF lesions at the lateral dorsal foramina at S1–S3 along with monopolar lesions at the L5 dorsal ramus. Patients were then evaluated every 3 months up to a year. The results of this small-numbered, prospective cohort study indicated a decrease in analgesic requirements and back and leg pain.
Cooled RF has also been described [75, 76]. This is a technology devised to decrease the heating occurring at the electrode tip during CRF. The result is decreased impedance at the electrode tip, with a theoretical delivery of higher energy, with a larger lesion size than CRF.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree