Abstract
The examination of the cerebellum is an integral part of prenatal second trimester ultrasound. During the examination the transcerebellar diameter, the size of the posterior fossa, and the presence of the vermis are studied. The diferential diagnosis between a normal cerebellum, its different normal variants, and some pathologies are discussed, including possible pitfalls.
Keywords
brain, cerebellum, congenital malformations, fetus, magnetic resonance imaging, ultrasound
Introduction
The fetal cerebellum develops throughout pregnancy and may be visualized starting from the first trimester. By the seventh week of gestation, the rhombencephalic vesicle, the precursor of the fourth ventricle and cisterna magna, is the most prominent structure of the brain. By the eighth week, the cerebellar hemispheres may be seen lateral to the fourth ventricle; the choroid plexus of the fourth ventricle is also present. The cerebellar hemispheres grow and develop toward the midline, and by 12 to 13 weeks’ gestation, the superior portion of the vermis appears in the midline between them. The vermis develops caudocranially and usually, but not always, finishes this “rotation” before 20 weeks’ gestation.
Disease
Anomalies of the posterior fossa typically manifest either by cystic dilatation or by an obliterated cisterna magna on prenatal ultrasound (US). Biometry of the cerebellum and, in particular, the cerebellar vermis measured by US or magnetic resonance imaging (MRI) often reveals specific cerebellar or vermian variants or anomalies, many of them with well-known prognoses. Possible fetal anomalies include cerebellar hypoplasia (CH) (isolated, or in fetuses with intrauterine growth restriction [IUGR]), rhombencephalosynapsis, Dandy-Walker malformation (DWM), cerebellar hemispheric asymmetry, vermian agenesis, pontocerebellar hypoplasia, and other syndromes associated with a small vermis.
Definition
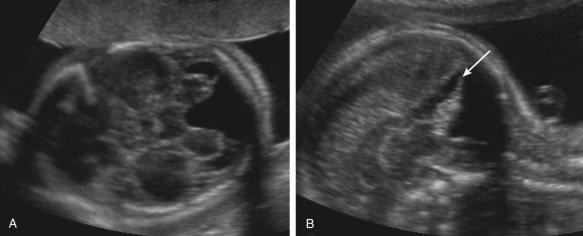
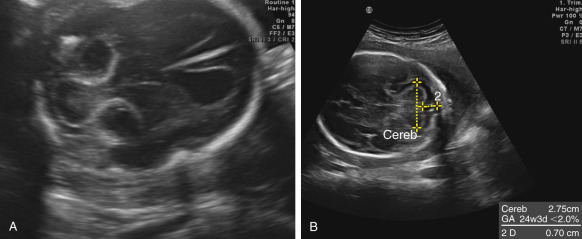
The transverse cerebellar diameter (TCD) ( Fig. 37.1A ) is a well-established measurement used for estimation of gestational age because it is less affected by IUGR than other parameters. The main differential diagnoses of a too-small TCD are two rare conditions: CH (see Figs. 37.1B and 37.2B ) and rhombencephalosynapsis ( Fig. 37.2A ). The TCD may also be small in 26% of fetuses with IUGR.
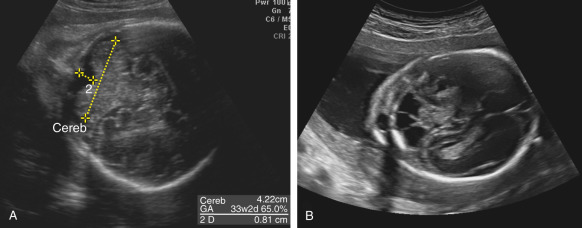
Cerebellar hypoplasia (CH) is essentially a growth disorder with intact major subdivisions of the cerebellum but reduced number of folia. In some cases, the pons may be also involved; this condition is called pontocerebellar hypoplasia and is usually transmitted as an autosomal recessive trait. CH is rarely diagnosed in utero and is usually associated with the presence of other anomalies or chromosomal defects, in particular, trisomy 18 (see Figs. 37.1B and 37.2 .B). In the fetus, CH cannot be differentiated from cerebellar atrophy, and it is usually not present or not diagnosed by the time of second-trimester anatomy screening scans, and sometimes even during third-trimester US examinations. When TCD is in the low-normal range or when there is a familial risk of CH, follow-up interval measurements should be performed until close to term; however, even this approach, including neurosonography and T2-weighted MRI sequences, may fail to reveal cases with proven molecular diagnosis.
Rhombencephalosynapsis is an even rarer condition; less than 200 cases have been reported in the world literature. It is defined as a total or partial agenesis of the vermis with fusion of the cerebellar hemispheres. The degree to which TCD is reduced varies, but usually a small TCD is clearly apparent (see Fig. 37.2A ). The diagnosis is confirmed if continuity of the folia from one hemisphere to the other (in axial and coronal planes) can be shown, and the vermis and a normal, triangular fourth ventricle (in coronal and midsagittal planes) cannot be seen. Rhombencephalosynapsis may occur as an isolated finding, or as a part of malformative syndromes; the best-known syndrome is Gomez-Lopez-Hernandez syndrome characterized by rhombencephalosynapsis, parietooccipital alopecia, trigeminal nerve anesthesia, intellectual impairment, craniosynostosis, short stature, and craniofacial anomalies. Prenatal diagnosis of this condition has been reported in at least 40 cases. Patients without associated malformations may have normal, or almost normal, neurodevelopment.
IUGR may present a diagnostic challenge when gestational age is unknown. Fetuses with a well-established diagnosis of IUGR and a small cerebellum have a twofold increase in perinatal mortality compared with other fetuses with IUGR.
Cerebellar hemispheric asymmetry is being diagnosed with increasing frequency in fetuses and newborns. Data obtained from the follow-up of children with cerebellar hemispheric asymmetry indicate that most cases are due to disruptive prenatal cerebellar insults, most likely hemorrhagic, leading to the development of unilateral hypoplasia. Other possible etiologies include cerebellar infarction, infection, and bleeding in a cavernous angioma or tumor. Regardless of etiology, it is believed that unilateral CH originates in the prenatal period. The clinical picture ranges from asymptomatic cases to severe impairment; patients with involvement of the vermis or the pons probably have a poorer prognosis. The natural history in cases diagnosed in utero may be dynamic over time, with intracerebellar hyperechogenicities that gradually develop into a cystic lesion leading to a small cerebellar hemisphere ( Fig. 37.3 ).
A small cisterna magna (less than 2 mm) should raise the suspicion of Chiari II malformation with open spinal dysraphism (see Chapter 41 ). This finding is usually associated with ventriculomegaly, abnormal skull shape, and disappearance of the subarachnoid spaces around the brain. Although identification of spinal dysraphism may be difficult, it almost always can be shown eventually using either a transabdominal or a transvaginal approach.
Identification of a large cisterna magna (greater than 10 mm) is an indication for a detailed examination of the vermis using orthogonal planes. A persistent Blake pouch may produce the false impression that the vermis is not completely formed, but in these cases the posterior fossa is usually of normal size, and the tentorium is not elevated. The differential diagnoses in patients with a large cisterna magna include mega cisterna magna, retrocerebellar arachnoid cyst, DWM, and other conditions affecting the vermis. In these patients, the first step is to study the normality of the vermis (see Imaging Technique and Findings). Although difficult to establish using US or MRI, a morphologically normal vermis reduces the differential diagnoses to only two entities: mega cisterna magna or retrocerebellar arachnoid cyst. When the vermis seems abnormal, DWM should be suspected.
Mega cisterna magna is defined as a cisterna magna larger than 10 mm. In many cases of apparent large cisterna magna (greater than 10 mm), a measurement in a wrong plane with the transducer in a plane between the axial and the coronal plane is the cause. Mega cisterna magna does not exert pressure on the adjacent cerebellum or cause ventriculomegaly. A large cisterna magna may be associated with macrocephaly. Isolated mega cisterna magna may be considered a normal variant and is not associated with neurodevelopmental delay.
Arachnoid cysts may be present at different locations in the fetal brain, but infratentorial retrocerebellar cysts are the most common arachnoid cyst diagnosed in utero. These cysts rarely may cause pressure on the cerebellum and brainstem; these fetuses may develop progressive ventriculomegaly and need surgical treatment comprising decompression of the cyst or ventriculoperitoneal shunt. Generally, the prognosis is similar to mega cisterna magna.
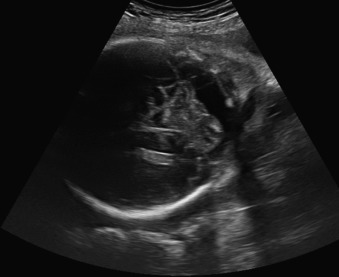
Dandy-Walker malformation (DWM) is defined by the presence of a cystic dilatation of the posterior fossa communicating with the fourth ventricle with varying degrees of hypoplasia or agenesis of the vermis and elevation of the tentorium ( Fig. 37.4 ). DWM may be accompanied by ventriculomegaly of different degrees of severity. The prevalence of DWM is unknown; its incidence has been reported to be 1 : 100,000 live births. An unusually wide communication between the fourth ventricle and the cisterna magna, and elevation of the tentorium are the additional required US signs of DWM. The degree of development of the vermis, in particular the presence of normal primary and secondary fissures, is important in establishing the prognosis (see Imaging Technique and Findings). The mass effect produced by dilatation of the fourth ventricle and cisterna magna makes the task of measuring the vermis and assessing its structure difficult even by MRI; in these patients, the presence of a normal or abnormal pons may be important (see subsequent discussion of pontocerebellar hypoplasia). Prognosis is related not only to the presence of associated malformations but also to degree of hypoplasia of the vermis. Survival rates range from 6% to 75% of affected newborns.