Cervical Pathology
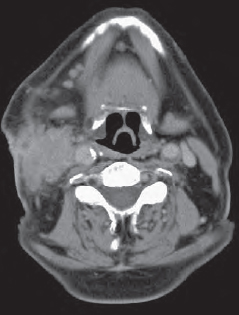
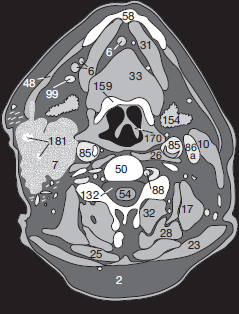
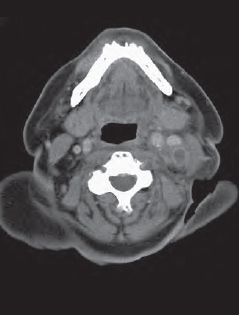
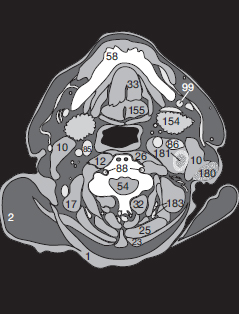
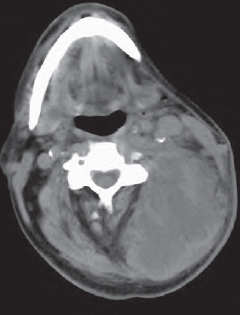
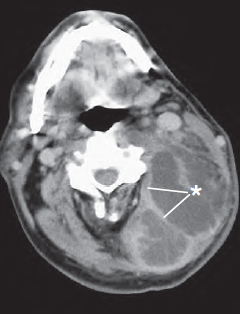
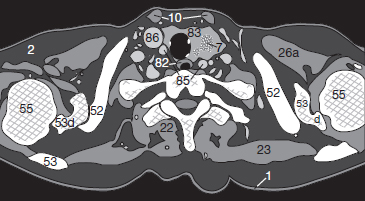
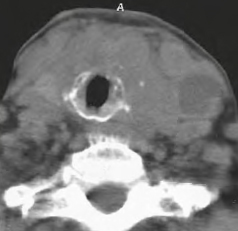
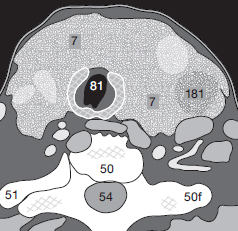
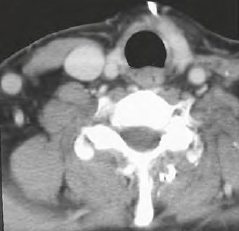
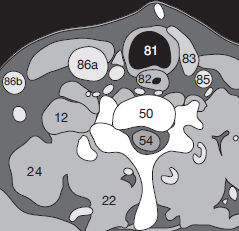
Enlarged cervical LNs ( Fig. 70.1a ) appear conspicuously as isolated nodular masses (6) that cannot be followed into adjacent levels (see p. 15). Large lymphomas (7) or conglomerate LN masses ( Fig. 70.1a ) often develop central necrosis (181). It is sometimes difficult to distinguish them from abscesses with central necrosis (181) as shown, for example, in Figure 70.2a . Abscesses typically infiltrate the surrounding adipose tissue with a streaky pattern of edema (180) so that structures such as arteries, veins, or nerves (on the left side of the neck in Fig. 70.2a ) become difficult to identify. In immune-suppressed patients, abscesses can become remarkably large. Compare the scans in Figures 70.3a (unenhanced) and 70.3b (enhanced): after injection of CM, the outer wall of the abscess (*) as well as the central septa have become enhanced. These appearances are so similar to large hematomas or necrotic tumors that a differential diagnosis may be difficult without a detailed clinical history.
Note also the atherosclerotic plaques or thromboses in the lumen of the carotid artery (85) as in Figure 70.1a .
The parenchyma of the thyroid gland (83) should appear sharply demarcated and have an homogeneous pattern in CT scans. The average transverse diameter of each lobe is 1-3 cm, 1-2 cm sagittally and 4-7 cm in craniocaudal direction. The total volume of the thyroid gland varies between 15 and 25 ml in adults. If the thyroid is enlarged, check for tracheal compression or stenosis (81) and the caudal border of the goiter should be determined.
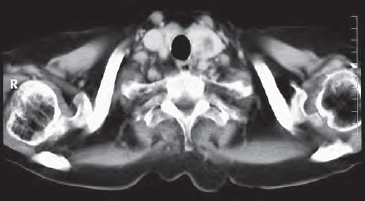
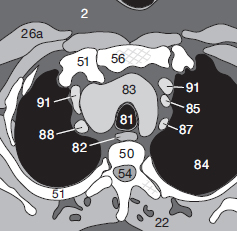
A benign struma (83) may extend into retrosternal regions and laterally displace supra-aortic vessels (85, 87, 88) ( Fig. 71.2 ).
The parenchymal structure of a thyroid carcinoma (7) appears inhomogeneous, and the contours are not easily distinguished from the remaining normal parenchyma (83) ( Fig 71.1a ).
In advanced stages of carcinoma ( Fig. 71.3 ), cervical vessels and nerves are completely surrounded by tumor, and areas of necrosis (181) appear. The tracheal walls (81) are compressed and may become infiltrated. After partial resection of a struma ( Fig. 71.4 ), some thyroid tissue (83) may still be seen close to the trachea. In this case the left internal jugular vein was also removed and the lumen of the right one (86a) is therefore larger than normal.

Before continuing to the next chapters, these exercises give you an opportunity to check your knowledge. The questions become increasingly difficult as you go along: the first question should pose no problems, whereas the last ones of each chapter will be a real challenge. Make the most of this opportunity for self-assessment and take it in good grace if you find you missed something. In our experience these little tests will help you to remember better what you have learned.
It is much more effective to look up each gap in your knowledge as it occurs than to skip a problem and turn directly to the answer. You should therefore only turn to the answers at the back of the book when you have solved each problem by yourself. That way you will not see answers to questions you haven’t tackled yet. It will keep you in suspense!
Exercise 9: Which window setting (window center and window width in HU) would you select for an optimal brain CT? Why? Before beginning the examination, what gantry angle do you choose for your slices in the planning topogram and what section thickness and section increments do you use? Why did you choose these settings?
Exercise 10: What do you remember about the criteria with which to distinguish the four types of intracranial hemorrhage? With which kinds of hemorrhage are you familiar? How can you differentiate between them in CT morphology? What complications or consequences must you particularly watch out for (consult pp. 54–57 for help)?
Type of hemorrhage:
Characteristics:
Exercise 11: How can you recognize a subarachnoid hemorrhage in children?
Exercise 12: Imagine the anatomy of the cerebral basal ganglia and then draw a transverse section at the level of the internal capsule. Compare your sketch with Figures 30.2a and 30.2b . Repeat this exercise occasionally until you can do it with ease.
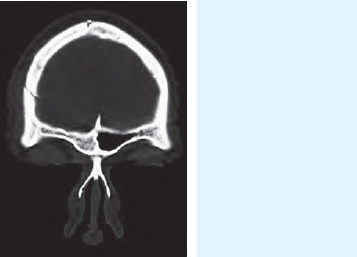
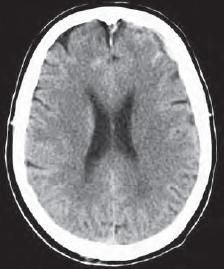
Exercise 13: Examine Figure 72.1 carefully. The patient was involved in a car accident. Do not settle for the most obvious feature; look for other variations or abnormalities. What do you suspect?
Exercise 14: Figure 72.2 contains an unusual variation; can you find it? After having noted it, look again to see whether you have really discovered all pathologic features.

Exercise 15:
The CCT in Figure 73.1 is of a 43-year-old patient. Make a note of your tentative diagnosis and how you would proceed.
Exercise 16:
Do you recognize anything unusual in Figure 73.2 ? Is there a pathologic abnormality? Or is it simply an artifact or even a normal finding?
Exercise 17:
Is there any feature in this orbital scan ( Fig. 73.3 ) that would not be considered a normal finding? Note your observations below. Don’t give up too quickly!

Exercise 18:
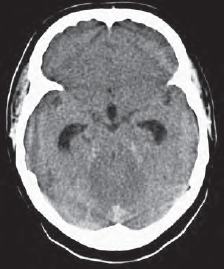
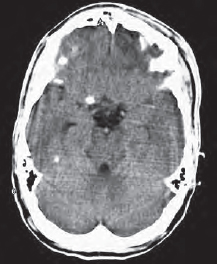
A confused patient, from a home for the elderly, with sus-pected intracranial bleeding is brought in for a CCT. How many fresh hemorrhages ( Fig. 73.4 ) do you see? What is your differential diagnosis? Which of them is the most probable diagnosis? Which additional information could also be helpful?

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree