Chapter 11 Cervical spine
Reasons for examination
Trauma
Cervical spine injury is relatively common and is typically seen in association with road traffic accidents, falls from a height and sporting injuries. Most neck injuries are caused by transmission of force to the neck from force applied to the head. Consequently, evidence of head or facial trauma, particularly in the comatose patient, requires ‘clearing the cervical spine’.1 The overriding concern is of damage to the spinal cord, as this may result in varying degrees of paralysis or even death.
The tendency in the past has been to order plain X-radiography for all patients who have undergone trauma that might have involved the cervical spine, however minor. The positive yield of such examinations is extremely low, as injuries to the cervical spine have been found to occur in between 2% and 6.6% of patients suffering blunt trauma. Much work has been done, particularly in Canada and the USA (National Emergency X Radiography Utilization Study – NEXUS), to establish criteria for imaging referral.2–7
Application of these clinical criteria has been reported to have the potential to reduce requests for cervical spine radiography by up to 25%.8 Significant savings could be made in staff and patient time, leading to financial savings as well as reductions in radiation dose to the patient.
A small but significant number of all victims of blunt trauma suffer injury to the spinal column, many of whom are young adults under the age of 40 years.9 Damage to the spinal cord, secondary to spinal trauma and due to squeezing or shearing forces caused by displaced bone, herniated disc material or buckling of ligaments, is an important consideration in this group of patients. Despite the fact that at least three times as many spinal column injuries occur without neurological deficit as with neurological deficit, care must be taken and the cervical spine immobilised until the need for it is eliminated.10 This caution must be observed as spinal cord injury without radiographic abnormality is a well-known phenomenon, most commonly described in children.11 In addition, hyperextension injuries of the cervical spine may injure the spinal cord without apparent damage to the spine seen on radiographs.
Another cause of spinal cord injury is the ‘whiplash’ injury, which involves extremes of flexion and extension of the neck. This is most frequently the result of a road traffic accident. As the occupant of a vehicle and restrained by a seatbelt, the patient’s head might be whipped backwards if the vehicle is struck from behind. Alternatively, the vehicle may stop abruptly, causing sudden forward flexion of the neck followed by forced extension. Most commonly muscular injury is seen, but in extreme circumstances quadriplegia may result from a violent whiplash injury.10
Mechanism of injury is an important consideration, as symptoms of spinal injury may be masked by other distracting injuries,12 or difficult to determine because of cranial or facial trauma.13,14 Reliance on the mechanism of injury for referral criteria is controversial,15 but there are specific mechanisms associated with high risk of injury, and work is ongoing in this field.16,17
Spinal clearance should, however, be achieved as promptly as possible, as there is significant morbidity associated with the prolonged use of spinal immobilisation in those who have undergone significant trauma.18
In the cervical spine lateral radiograph, a careful evaluation of the soft tissues may provide significant information about the location and extent of an injury. Even this can be the subject of debate. In adult patients it is said that the normal distance between the posterior aspect of the pharyngeal air column and the anterior vertebral margin measured at the body of C3 should be less than 7 mm;19 however, in their study Herr et al.20 quote less than 4–5 mm. The distance from the posterior aspect of the trachea to the anterior vertebral margin measured at the inferior aspect of C6 is more uniformly referred to as, ‘should be less than 21 mm’.19 An increase in these measurements is strongly indicative of the presence of a haematoma. Considering this information on evaluation of soft tissues, it is clear that inclusion of soft tissue is essential in the lateral projection.
Such prevertebral soft-tissue haematomas are common in patients with injury to the anterior spinal column, commonly avulsion fracture or hyperextension injury.20 Ligament damage can occur without fracture; visualisation of the prevertebral haematoma will help demonstrate the presence of such an injury, but is insensitive as a predictor of fracture or injury site.
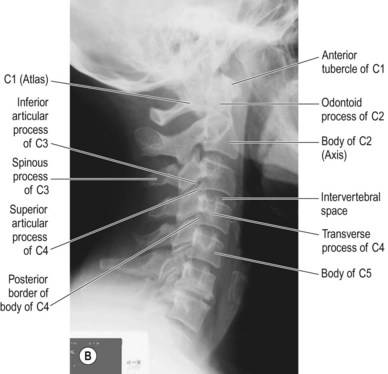
Vertebral alignment can be demonstrated on the lateral cervical spine radiograph and is commonly assessed using examination of continuous convex lines as described below and shown in Figure 11.1.
Line 4: The fourth line joins the tip of the spinous processes.
The cervical spine is normally lordotic in curvature; loss of lordosis has been said to be an indication of severe muscular spasm and is taken as a sign of cervical spine injury,10 commonly seen in ‘whiplash’ type injuries. However, such loss of lordosis can be accentuated by neck position and may be a normal finding if the ‘stiff neck’ is held in a slightly flexed position during imaging. Hence it is not a reliable sign of definite injury.
Neck pain
Radiographic examination of the cervical spine is not recommended for the routine investigation of neck pain. However, cervical spine radiography may be useful where there is a history of trauma, or worsening/unresolved neurological symptoms, and in children where such pain is uncommon without a cause.21
Degenerative disease processes
Symptoms of degenerative disease are commonly due to disk or ligamentous changes not demonstrated by plain film radiography.21
Rheumatoid arthritis
This can cause instability of the atlantoaxial joint. Subluxation may be demonstrated by a lateral view in flexion.21
Recommended projections
Imaging of the cervical spine, particularly in cases of trauma, has been the subject of worldwide debate for some considerable time. Although the cervical spine radiograph has long been the routine method for imaging this anatomical region, imaging department protocols vary widely as to the required ‘routine’ series to be undertaken. More recently, computed tomography (CT) has been used as an additional examination for equivocal findings, but there is a growing body of evidence to suggest that CT should be used as the first-line investigation.2,15,22–24 This already tends to be the case where the patient has a head injury requiring CT,25 owing to the correlation between major head injury and cervical spine injury, especially in the comatose patient. The increased capabilities of multidectector CT allow for better image detail and thereby enable the detection of injuries not seen on plain film.
Despite the growth in use of CT, in many centres the cervical spine is still most rapidly and most commonly initially assessed with plain X-radiography. The NEXUS study4 has looked at its appropriateness for imaging and has proposed that there is no risk of cervical spine injury if ‘low risk’ criteria are met on patient examination. These criteria are:
As previously stated, imaging department protocols vary widely. Many centres perform a three-view series: lateral C1–C7 plus AP C3–C7 and AP C1–C2 (‘odontoid process or peg’/‘open mouth’ view). Unfortunately there is no consensus in the literature as to what should be used. Harris et al.26 reported that whereas 81% of Orthopaedic Trauma Association members responding to his survey used the three-view series, only 31% of the National Association of Spinal Surgeons respondents did so.
Studies such as that performed by West et al.27 compared single-view to three-view screening, finding an increase in sensitivity from 81.8% to 83.3% in a comparatively small sample. A similar study in paediatrics by Baker et al.28 found that a lateral view had a sensitivity of 79% for cervical spine injury, compared to 94% for the three-view series. MacDonald et al.29 had similar findings to West and concluded that the three-view series alone was not always sufficient for adequate diagnosis.
There are other suggestions in the literature. Holliman et al.30 suggest that the AP C3–C7 view adds little to the diagnostic ability of the series; Turetsky et al.31 suggest its replacement by 30° trauma obliques. Doris and Wilson32 advocate the use of obliques in a routine five-view series.
A problem with including oblique views as a five-view series is the question of ‘which obliques?’: 30° as above, 60° as advocated by Abel,33 or something in between, such as 45°, as is a familiar suggestion in radiographic positioning texts.34
Daffner35 goes further and discusses a routine six-view series: the five-view series as discussed above (but again with no mention as to the angle of obliquity) with the addition of a swimmer’s view. It is interesting, from the perspective of a UK radiographer, to look at his results for plain X-radiography: examinations taking up to 46 minutes, with 13 radiographs being taken in one case, and 77% of patients requiring at least one repeat radiograph – standards related to radiation dose and patient care that would be unacceptable in the UK.
Following performance and evaluation of the lateral and such accessory views as may be required, the ‘cervical spine series’, including anteroposterior (AP), open mouth and oblique views, can be completed if no significant instability has been previously demonstrated.36
Some studies advocate the inclusion of flexion and extension radiographs37 in the ‘routine cervical spine series’ (seven-view?), but care must be taken depending on the degree of suspicion of instability. Where a small subluxation is demonstrated, significant ligamentous injuries may be revealed by flexion and extension views. However, Pollack et al.38 found that flexion and extension images failed to demonstrate any injuries not already demonstrated by other images; hence their usefulness must be questioned.
The cost and clinical efficacy of such protocols has also been called into question by Mirvis et al.39 They query the use of ‘routine’ CT for clarifying areas of uncertainty, or non-visualised areas in asymptomatic patients, finding a less than 1% positive yield, and that finding was said to be a clinically unimportant injury. Careful clinical assessment of the patient is held to be more effective.
Also, information gained from the initial lateral image can be readily, if not necessarily fully, interpreted by the attending A&E doctor. This is less likely with CT examination, which requires radiological interpretation. CT has, however, been shown to be a more cost-effective option for imaging medium- to high-risk patients.23
Nunez et al.40 found that 35% of fractures detected by CT were not seen on initial plain radiography in the most seriously ill group of patients, and that a third of these fractures were unstable, located mostly at C1/2 or C7/T1, again stressing the importance of adequate visualisation of C7. Suboptimal examinations were often found to be due to patient condition, and the suggestion is that CT be included for this most seriously injured patient group.
Lateral cervical spine
The image receptor (IR) is vertical.
Positioning
Method 1: patient standing/sitting erect (Fig. 11.2A,B)
• The patient is seated/standing with the lateral aspect of their shoulder resting against the IR
• The median sagittal plane (MSP) is parallel to the IR, with the neck extended to raise the jaw and prevent the angles of the mandible being superimposed over the vertebral bodies
• The shoulders should be relaxed and depressed as much as possible as they may obscure the lower cervical vertebrae and the cervicothoracic junction. It has been suggested that patients with broad muscular shoulders should be given a weight to hold in each hand to help project the shoulder masses below the level of C7.34 However, this is often counterproductive, as patients frequently hunch their shoulders in an attempt to hold the weights firmly while keeping still. This is especially likely if what is being attempted is not carefully explained to the patient. Exposing the radiograph on arrested expiration may help.
Method 2: patient supine (Fig. 11.3)
Superimposition of the shoulders can be more problematic in this position and several methods of applying shoulder traction have been described.41,42 The key to success is again careful explanation to the patient to achieve their cooperation; traction should be applied above the elbow joints, and slowly to prevent the patient working against the application of traction.
• The trolley is positioned to ensure that the long axis of the cervical vertebrae is parallel to the wall or ceiling track of the X-ray tube
• 2 m focus receptor distance (FRD) is selected and the tube is centred approximately to the middle of the lateral aspect of the neck; approximate collimation to the neck should also take place at this point
• The IR is placed vertically at the side of the neck remote from the tube, its long axis parallel to the patient’s MSP. Support for the IR may be via independent support designed for A&E examinations, erect holder as used for chest radiography, or sponge pads and sandbags
Centring point
In the middle of the neck at the level of the thyroid eminence
A range of centring points are quoted for this examination. Fixed centring points, such as ‘2.5 cm posterior and inferior to the angle of mandible’,43 take no account of patient size or shape and in a larger than average person would lead to the beam being centred at soft tissues anterior to C2/3.
Collimation
Soft tissues must be included, particularly in cases of trauma, where, as previously discussed, changes in appearance of the soft tissues can be a strong indicator of the presence of bony injury.18,20
Criteria for assessing image quality
• Atlanto-occipital articulations, body of T1, cervical spinous processes and soft tissue structures of the pharynx are included on the image
• Mandible should be cleared from the vertebral bodies, and the angles of the mandible in close approximation
• Left and right posterior borders of the vertebral bodies are superimposed to show no rotation
• There should be clear intervertebral joint spaces with no overlap of superior and inferior borders of vertebral bodies, to show no tilt of the cervical column
• Sharp image demonstrating soft tissue structures of the pharynx in contrast to bone and air in the trachea, detail of the bony cortex and trabeculae, the joint space between C7 and T1 and spinous processes of the cervical vertebrae
| Common errors | Possible reasons |
|---|---|
| Posterior borders of the vertebral bodies not superimposed |