, Joon Woo Lee1 and Jong Won Kwon2
(1)
Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Kyonggi-do, Republic of Korea
(2)
Department of Radiology, Samsung Medical Center, Seoul, Republic of Korea
9.1.2 Atlas Fracture
9.1.5 Hangman’s Fracture
9.2.1 Flexion Injuries
9.2.3 Extension Injuries
9.6.2 Atlas Fracture
9.6.5 Hangman’s Fractures
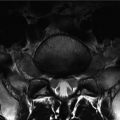
9.6.8 Intraspinal Hemorrhage
Abstract
In this chapter, we will describe upper cervical spine injury (atlanto-occipital dislocation, atlas fracture, atlantoaxial rotatory fixation, odontoid process fracture, and hangman’s fracture) and lower cervical spine injury (flexion injury, flexion–rotation injury, extension injury, and vertical compression injury). We also include spinal cord contusion and intraspinal hemorrhage (epidural, subdural, and subarachnoid).
In this chapter, we will describe upper cervical spine injury (atlanto-occipital dislocation, atlas fracture, atlantoaxial rotatory fixation, odontoid process fracture, and hangman’s fracture) and lower cervical spine injury (flexion injury, flexion–rotation injury, extension injury, and vertical compression injury). We also include spinal cord contusion and intraspinal hemorrhage (epidural, subdural, and subarachnoid).
9.1 Upper Cervical Spine (Occiput (C0)–C1–C2)
Injury of upper cervical spine is defined as injury of skull base (C0, occiput)–atlas (C1)–axis (C2) complex which are the atlanto-occipital articulation and atlantoaxial articulation. The convex occipital condyles articulate with concave joint surfaces of the atlas. The atlantoaxial joint is composed of both lateral mass articulations and an atlantodental articulation. Both paired alar ligaments bilaterally connect the dens with the occiput condyle. The transverse ligament protects the atlantoaxial joints from instability or subluxation.
9.1.1 Atlanto-occipital Dislocation
Atlanto-occipital dislocation is characterized by complete disruption of all the stabilizing ligaments between the occiput and atlas (C1). This injury has high fatality because of stretching of the brainstem, resulting in respiratory arrest. Plain radiograph and CT with coronal and sagittal reformats will demonstrate increased distance between the occipital condyles and the lateral masses of C1. MR imaging is rarely performed because of the patient’s unstable vital status.
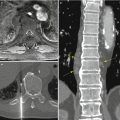
9.1.2 Atlas Fracture
The atlas fracture is caused by vertical compressive force to C1, usually from the occipital condyles to the lateral masses of C1. The lateral masses are driven laterally away from odontoid process of C2, resulting in unilateral or bilateral fractures at the anterior and posterior junctions of the arches with the lateral masses. Displacement of the lateral masses may result in either disruption of the transverse ligament or an avulsion fracture of the lateral masses of C1. The open-mouth (odontoid) view may show unilateral or bilateral displacement of the C1 lateral masses with respect to the articular pillars of C2. The fractures can consist of 2–4 fragments and this injury is mechanically unstable. On MRI, the injury in the transverse ligament of the atlas means the unstable injury. The atlantoaxial instability is determined using the following criteria: the sum of displacement of the lateral masses of C1 compared to C2 > 8 mm on the open-mouth view (rule of Spence) (Spence et al. 1970), the atlantodental interval (ADI) >4 mm in adults, and MRI evidence of ligamentous disruption or avulsion. Atlas fractures are classified into four types: isolated posterior neural arch fracture (type I), isolated anterior neural arch fracture (type II), anterior and posterior neural arch fracture (type III, Jefferson fracture), and comminuted lateral mass fracture (type IV). The lateral mass fracture may occur because of a lateral tilt or eccentric axial loading.
9.1.3 Atlantoaxial Rotatory Fixation
Atlantoaxial rotatory fixation is defined as persistent pathological fixation of the atlantoaxial joints in a rotated position, from rotatory fixation within the normal range of C1–C2 motion to obvious rotatory atlantoaxial dislocation. The open-mouth view shows an asymmetry of the lateral masses of C1. CT demonstrates the displaced and rotated atlantoaxial articulation. The rupture of the transverse ligament or alar ligaments may result in a neurologic injury because of the spinal canal compromise. Atlantoaxial rotatory fixations usually occur in children but rarely in adults. Atlantoaxial rotatory fixation can be classified into four types, based on the direction and degree of displacement: atlantoaxial rotatory fixation with no anterior displacement (type 1, the most common, intact transverse ligament), rotatory fixation with anterior displacement of 3–5 mm (type 2), rotatory fixation with atlantoaxial subluxation of more than 5 mm (type 3), and rotatory fixation with posterior displacement (type 4, extremely rare) (Looby and Flanders 2011).
9.1.4 Odontoid Process (Dens) Fractures
There are three types of odontoid fractures (Rao et al. 2005). Type I fracture is an infrequent, stable avulsion fracture of the tip and should be distinguished from an os odontoideum. Type I fracture will have irregular noncorticated borders unlike an os odontoideum. Type II fracture, the most common, is a transverse fracture through the base of the odontoid process. This type is unstable and needs surgical intervention to prevent spinal cord compression. Type III fracture is a stable fracture that passes through the superior body of C2 (Anderson and D’Alonzo 1974). Odontoid fractures are best visualized on the coronal or sagittal MR imaging or reformatted CT imaging but can be visualized with open-mouth view as well.
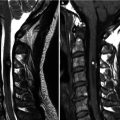
9.1.5 Hangman’s Fracture
Hangman’s fracture is traumatic spondylolisthesis of the axis (C2), which can arise from forcible hyperextension of the head and distraction of the neck. This would occur during judicial hanging. It can occur in rapid deceleration of the head caused by motor vehicle accidents, diving accidents, and falls. Spinal cord damage is uncommon and most patients do not have neurologic symptoms because the spinal canal is wide at the C2 level. Hangman’s fractures are classified into three types based on their displacement and mechanism of injury (Levine and Edwards 1985). Type I hangman’s fracture (axial loading and hyperextension) is bilateral C2 pedicle fractures with minimal (less than 3 mm) displacement of the body of C2. Type II (hyperextension and rebound flexion) is an isolated fracture, with more than 3 mm fragment displacement, greater than 15° angle at the fracture site, and an abnormal C2–C3 disk space. Type IIA hangman’s fracture subtype (flexion distraction) demonstrates no anterior displacement but severe angulation at the fracture site, resulting in disruption of the C2–C3 disk space. Type III (primary flexion and rebound extension) consists of the type II changes and a C2–C3 articular facet dislocation. The angulation is also much more severe in type III fractures.
Plain radiograph demonstrates anterior displacement of C2 on C3. CT better demonstrates the pattern and extent of injury. MRI is helpful in detecting such soft tissue injuries, as well as possible spinal cord injury. Fat-saturated T2-weighted image or STIR image can demonstrate abnormal increased signal intensity in the cervical cord, anterior longitudinal ligament, posterior spinal soft tissues, and intervertebral disk compatible with edema or hemorrhage.
9.2 Lower (Subaxial) Cervical Spine (C3–C7)
Lower cervical spine injuries result from hyperextension, hyperflexion, axial load, and rotational forces and are most commonly associated with motor vehicle accidents. Instability of the cervical spine can remain undetected on flexion/extension plain radiograph or CT. Recent imaging protocols for the assessment of cervical trauma patients include routine CT of the entire cervical spine with three-dimensional reformation and the utilization of MR imaging with fluid-sensitive sequences. MRI has been found to be superior to CT in the detection of nonosseous cervical injuries. MR imaging has become a valuable tool for the detection of traumatic anterior and posterior longitudinal ligament, disk and cord injury, and cervical instability.
9.2.1 Flexion Injuries
Simple Wedge Compression Fracture
A simple wedge compression fracture occurs from a flexion injury with loss of height of the anterior vertebral body and buckling of the anterior cortex. The posterior column remains intact. Lateral plain radiograph shows the wedge-shaped height loss of anterior vertebral body with swelling of the prevertebral soft tissues, increased density of the endplate due to bony impaction, and loss of definition of the superior endplate. An AP view has limited value and may show increased interspinous distance and loss of definition of the superior endplate.
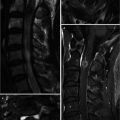
Flexion Teardrop Fracture
The flexion teardrop fracture is an avulsion of the anteroinferior corner of a vertebral body (most commonly at C5) with a forceful hyperflexion and vertical axial compression. The triangular-shaped bony fragment is displaced anteriorly and resembles a teardrop. This fracture is associated with anterior and posterior ligamentous disruption and distorted facet joints. The retropulsed posterior cortex may compress the spinal cord, resulting in spinal cord contusion and quadriplegia. Lateral plain radiograph shows teardrop fracture fragment of the anteroinferior corner of a vertebral body, alignment abnormalities due to ligamentous instability, and diffuse prevertebral soft tissue swelling. CT helps to determine the extent of the fracture of the involved vertebra and the displacement of the fragment into the spinal canal and to assess the adjacent vertebrae. MRI is helpful to detect the spinal cord injury, ligamentous, and disk injury. Ligament injury is best evaluated on fat-suppressed, midsagittal images. Nuchal ligament injury is commonly seen as high signal intensity between the spinous processes and at the tips of the spinous processes on fat-suppressed T2-weighted sagittal image or STIR sagittal image (Dundamadappa and Cauley 2012).
Anterior Subluxation
Anterior subluxation or hyperflexion sprain occurs in the cervical spine when the posterior ligament complex is disrupted in flexion. The posterior ligament complex consists of the posterior longitudinal ligament, the ligamentum flavum, the capsular ligaments, and the nuchal ligament. The facet joints may be subluxed anteriorly and the bony structure remains intact. Unrecognized and untreated anterior subluxation may cause cervical instability. The radiological findings are hyperkyphosis at the level of injury, widening of the interspinous space, anterior narrowing and posterior widening of the disk space, displacement of subluxed vertebra, and the subluxed facet joints. CT images and an adequate lateral plain radiograph can help diagnose these injuries.
Bilateral Facet Dislocation
Bilateral facet dislocation is the most severe type of hyperflexion injury and highly unstable. The ligamentous structures (the posterior ligamentous complex and the anterior longitudinal ligament) are disrupted, and the injured vertebral body is displaced anteriorly (50 % or more). Both inferior articular facets dislocate anterior to the superior facets of the subjacent vertebra. Bilateral facet dislocations can be associated with spinal cord injury and traumatic disk herniation (tear of the annulus fibrosus) at the level of the injury. Sagittal reformatted CT can show the dislocated vertebral body and articular facets anterior to the subjacent vertebral body and facets (Daffner and Daffner 2002). MRI should be performed to evaluate the spinal cord and other intraspinal injuries.
Clay Shoveler Fracture
The clay shoveler fracture is an oblique avulsion fracture of the spinous process in lower cervical spine, most commonly C6–T1. This injury occurs in abrupt flexion with lower neck muscular contraction or direct blow to the spinous process. Since this injury involves only the spinous process, the clay shoveler fracture is a stable fracture, and it is not associated with neurologic impairment. This injury is well detected on the lateral view as an avulsed bony fragment of the spinous process.
9.2.2 Flexion–Rotation Injuries (Unilateral Facet Dislocation)
A unilateral facet dislocation occurs with hyperflexion in combination with rotation. One inferior articular facet of an upper vertebra is displaced anterior to the superior articular facet of a lower vertebra. The posterior ligaments may be disrupted, but this injury is mechanically stable due to locked-in-place vertebra. The cervical nerve root can be compressed by the displaced inferior facet. Radiographic findings are anterior displacement of less than 50 % of one cervical vertebra, rotation of the affected vertebra, and lateral displacement of spinous process. The AP view may show a disruption of the line connecting the spinous processes. The dislocated inferior articular facet of the upper vertebra is seen projecting within the neural foramina.
9.2.3 Extension Injuries
Hyperextension injuries occur when there is forceful posterior displacement of the head or upper cervical spine such as in a motor vehicle accident. Extension injuries are more common in patients with ankylosing spondylitis, diffuse idiopathic skeletal hyperostosis (DISH), or congenital spinal stenosis because of the less flexibility from ossification of the ligamentous complexes and disk spaces. Hyperextension injuries to the soft tissues can occur in the longus colli and capitis muscles, the anterior longitudinal ligament, the intervertebral disk, and the posterior longitudinal ligament. Hyperextension fracture more commonly occurs in the articular pillars, the posterior vertebral body, the laminae, the spinous processes, or the pedicles.
The extension teardrop fracture usually occurs when a hyperextension force produces an avulsion fracture of the anteroinferior corner, in contrast to the flexion teardrop fracture in which the fragment is produced by vertebral compression (Stabler et al. 2001). This fracture only involves the anterior column and therefore is stable in flexion and unstable in extension. On the lateral view, there is a diffuse prevertebral soft tissue swelling with a characteristic triangular avulsion fracture fragment.
Laminar fractures are uncommon and usually occur after a hyperextension injury. This injury is mechanically stable, but neurologic stability depends on the location of bony fragments in the spinal canal.
9.2.4 Vertical Compression Injuries
Vertical compression fractures are much more common in the thoracolumbar spine, but can also occur in the cervical spine (Table 9.1). The burst fractures cause anterior cord compression. Radiographic findings are vertical fracture line in AP view, protrusion or retropulsion of the vertebral body. CT and MRI are required to document the exact displacement of the fractured bony components, retropulsed fragments, and their relationship to the spinal cord.
Table 9.1
Cervical spine injuries: mechanism of injury
Mechanisms | Injuries |
|---|---|
Hyperflexion | Simple wedge compression fracture |
Flexion teardrop fracture | |
Anterior subluxation (hyperflexion sprain) | |
Bilateral facet dislocation | |
Clay shoveler fracture | |
Hyperflexion + rotation | Unilateral facet dislocation (locked vertebra) |
Hyperextension | Hyperextension dislocation (hyperextension sprain) |
Avulsion fracture of the anterior arch of the atlas
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|