Sonographic pattern
US features
Estimated risk of malignancy, %
FNA done for diagnosis size cutoff (largest dimension)
High suspicion
Solid hypoechoic nodule or solid hypoechoic component of a partially cystic nodule with one or more of the following features: irregular margins (infiltrative, microlobulated), microcalcifications, taller-than-wide shape, rim calcifications with small extrusive soft tissue component, evidence of extrathyroidal extension
>70–90
Recommend FNA at ≥1 cm
Intermediate suspicion
Hypoechoic solid thyroid nodule with smooth margins without microcalcifications, ETE, or taller-than-wide shape
10–20
Recommend FNA at ≥1 cm
Low suspicion
Isoechoic or hyperechoic solid nodule or partially cystic nodule with eccentric solid areas, without microcalcification, irregular margin or ETE, or taller-than-wide shape
5–10
Recommend FNA at ≥1.5 cm
Very low suspicion
Spongiform or partially cystic thyroid nodules without any of the sonographic features described in low, intermediate, or high suspicion patterns
<3
Consider FNA at ≥2 cm
Observation without FNA is also a reasonable option
Benign
Purely cystic thyroid nodules (no solid component)
<1
No biopsy

Fig. 15.1
Thyroid nodule with normal or elevated TSH
15.2 Challenge #1: Wide Spectrum of Practitioners Performing Thyroid Ultrasound
Practitioners who perform and interpret thyroid ultrasound range from radiologists to surgeons and endocrinologists. Each of these specialists brings their own background and experience into image interpretation and may perform ultrasound for different reasons. These reasons include diagnosis of thyroid nodules , localization for biopsy, or assessment of characteristics to assist in surgical planning (e.g., proximity to the recurrent laryngeal nerve or malignant involvement of lymph nodes). Furthermore, some practitioners may interpret the images in real time, while others retrospectively view saved cine-images acquired by a technician. This heterogeneity brings with it challenges in the standardized assessment of thyroid nodules. The level of adequacy of training for radiology residents in ultrasound has been addressed in multiple studies. One of the main issues for the radiologist appears to be lack of detailed anatomic knowledge and an overall inability to identify key anatomic landmarks [7].
Most clinicians who use ultrasound in their practices who are not radiologists will learn enough ultrasound skills to be able to provide a careful and systematic assessment of the thyroid and surrounding structures during their daily practice. Precisely because they are not radiologists, they bring unique additional skills that aid in the care of the patient. For the endocrinologist this added value includes knowing the basics of the endocrine diseases that are affecting any particular patient’s thyroid, often including a longitudinal relationship with the patient and their long-standing endocrine history as well as laboratory and biomarker values. Surgeons who use ultrasound have the additional benefit of being able to correlate ultrasound findings with intraoperative findings which over time provide an impressive learning tool for correlating pathology, anatomy, and ultrasound images. Of course, the training these clinicians have cannot replace the long and arduous training which a radiologist undergoes, but with adequate time commitments, non-radiologist clinicians can come to recognize the most important patterns in thyroid ultrasound that are commonly seen in their patients.
Unfortunately training of non-radiologist specialists in ultrasound at this time is not an integral process of the training in general surgery or head and neck surgery or medical specialties such as endocrinology. Other residencies such as Obstetrics and Gynecology have successfully integrated ultrasound training into their programs for more than a decade. Efforts to include ultrasound training during surgical residency or fellowship are ongoing. Postgraduate thyroid ultrasound courses are available from multiple organizations in the United States: examples include The American Association of Clinical Endocrinologist, the American College of Surgeons, and the American Academy of Otolaryngology Head and Neck Surgery. Most of these organizations offer 1–2-day courses including didactics and hands-on practice sessions. Furthermore, some of these organizations have created programs with the American Institute of Ultrasound in Medicine to create a voluntary peer review process after which initial accreditation is given enough for a 3-year period.
Clinician performance in the tasks of pattern recognition in ultrasound will surely be influenced by various factors such as fatigue, emotion, reading time, environment, and previous biases. These factors have not been well studied in non-radiologists performing ultrasound, but clinicians should try to minimize fatigue and distractions that will influence their ability to formulate complex images into clear-cut patterns.
15.3 Challenge #2: Training in Pattern Recognition
Practically speaking, basic ultrasound course offerings do not provide an extensive experience in pattern recognition of common thyroid ultrasound findings. While there is no consensus on how many examinations are required to achieve an acceptable level of competency with head and neck ultrasound, several studies focusing on the learning curve in ultrasound examinations have established that approximately 25–50 focused examinations are needed to achieve greater than 90 % concordance with a radiologist interpretation of the same examination [7, 8]. One article recently addressed the issue of observer experience in the evaluation of thyroid malignancy and lymph node metastases. Moon et al. looked at the use of ultrasound by clinicians with less than 2 years of experience versus greater than 7 years of experience in preoperative ultrasound staging in 1421 patients. Preoperative staging ultrasound included an assessment for extrathyroidal extension and ultrasound features of lymph node metastasis, including shape, echogenicity, microcalcifications, cystic change , and vascularity. Their data showed that the two groups differed only in their ability to assess the lateral neck compartment lymph node involvement with the more experienced group showing a 64 % ability to correctly diagnose lateral nodal involvement versus 39 % for the less experienced group [9]. The complexity generated when combining these individual factors into various clinical possibilities requires the practitioner to be well versed in recognizing multiple patterns of pathology, which requires extensive practice and experience.
A number of methods are used to characterize ultrasound targets including pattern recognition, simple scoring systems, and complex classification systems, some of which use mathematical models. Some of these models have been elaborated on in the previous chapter on risk stratification strategies. The technological ability to acquire higher and higher resolution and thus the ability to reliably and reproducibly visualize smaller anatomic structures have come at the cost of increasing number of images per patient that need to be interpreted and mentally analyzed. Pattern recognition training by individuals happens over time and evolves from looking for patterns in a particular nodule to looking at patterns in the entire examination. An example of combining individual features to see the “pattern of a malignant nodule” is shown in Fig. 15.2. An example of combining individual features of an entire thyroid ultrasound to recognize a “pattern of aggressive malignancy” is shown in Fig. 15.3.



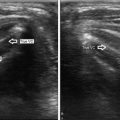
Fig. 15.2
Pattern recognition : combining individual features helps recognize thyroid nodule as malignant

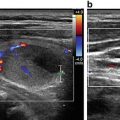
Fig. 15.3
Pattern recognition: combining individual features helps recognize aggressive malignancy with extrathyroidal extension and lateral nodal involvement
In addition, post-ultrasound activities such as analyzing gross and pathologic specimens and comparing them to the ultrasound images will result in dramatically improved clinical judgment over time (see Figs. 15.3 and 15.4, e.g., of how this kind of correlation helps clinicians).


Fig. 15.4
Pattern recognition: comparing individual features helps recognize thyroid nodule as lymphoma
15.4 Challenge #3: Recognizing the Pattern of Benign Nodules
Combining ultrasound features to predict benignity is included in all recent thyroid nodule guidelines since they impart the largest cost saving when applied over large populations [5]. For example, on a group of patients with a prevalence of thyroid cancer set at 10 %, 1000 nodules lacking the future features of hypoechogenicity, taller-than-wide shape, calcifications, and irregular borders would have to be biopsied to detect ten cancers. Pure cysts, small <1 cm colloid-filled cystic nodules, “white knights” (diffuse hyperechoic nodule in the setting of Hashimoto’s), and spongiform nodules meet these criteria in multiple studies, and thus most society guidelines report that the chance of malignancy in these nodules is so low that most do not recommend FNA unless there are other factors that drive the need for aspiration [4, 5, 10, 11]. A nodule with diffuse internal cysts described as spongiform (or honeycombed) or an image described as a “puff pastry pattern ” with the appearance similar to a many layered flaky puff pastry appears to be characteristic of benign colloid nodules or goiters [2, 3]. When these criteria are applied strictly and with confidence, many FNAs on benign nodules can be avoided. To recognize benign patterns, clinicians must be familiar with the validity of these in their own local referral patterns and assess their own confidence in recognizing these patterns.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree