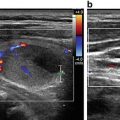
Fig. 31.1
This is an image depicting the true (TC) and false (FC) vocal cords on transcutaneous laryngeal ultrasound using the ventral approach
31.3 Steps and Tips in Carrying Out a TLUSG of the VCs
Similar to performing an USG for the thyroid or parathyroid gland, it is recommended that the patient should be placed in a supine position with the neck slightly extended and arms resting on the side. After applying ample amount of gel over the thyroid cartilage area, a linear transducer is placed transversely in the middle of the thyroid cartilage. It is important that the transducer is placed gently on the cartilage rather than pressing too forcefully onto the cartilage. The reason for using ample amount of gel is maximize the physical contact while avoiding air between the linear probe and the concavity of the cartilage. This is particularly crucial in male patients because the thyroid cartilage is usually more angulated in the middle than female patients and so there is less direct contact between the probe and cartilage. In terms of selecting the most appropriate USG probe for TLUSG , we believe the lower the frequency (i.e., 5–10 MHz) the better because the lower frequency helps with the tissue penetration and as mentioned earlier, the quality of the images depends on how well the USG waves could propagate through the thyroid cartilage. After placing the probe transversely on the body of the cartilage, the region is scanned cranio-caudally along the sagittal plane until either the true or false VCs are clearly visualized. In the transverse plane, the false VCs are located immediately above the true VCs while the arytenoids are usually in the same transverse plane as the false VCs. To enhance visualization, it is recommended to turn up the gain or gray-scale during examination until the false VCs become hyperechoic. Based on the experience of previous authors, probably among the three moving landmarks on TLUSG (namely, false VCs, true VCs and arytenoids), the most easily visible landmark (at least initially) is the false VCs [15]. This is supported by a study that showed the rate of visualization of false VCs is almost three times higher than that of true VCs (92.7 % vs. 36.7 %, p < 0.05) and is also slightly higher than that of the arytenoids (89.8 %) [16]. Once one or more landmarks are visualized on TLUSG , there are two types of VC movement that one should observe to determine if the function of the VCs has been compromised. First is passive (where a patient is breathing normally) and the other is active (where a patient is instructed to either phonate or perform a Valsalva maneuver). To date, there is no consensus on which type of VC movement or active maneuver provides the most reliable assessment. However, given that passive movement is technically the easiest to do, most clinicians prefer passive movement alone to determine if a patient has a unilateral VCP or not. For a patient without VCP , during passive movement, one could observe spontaneous, subtle symmetrical movement of both VCs with each cord moving in a rhythmic matter along with respiration while for a patient with an unilateral VCP , this passive movement either becomes asymmetrical or completely absent on the affected side. However, it should be noted that there is a small percentage of patients who do not have spontaneous passive movement in their VCs and so, it is not unreasonable to combine the finding of passive movement with at least one other active maneuver to confirm the motility in both VCs. In terms of active maneuvers, the recommended technique is the Valsalva maneuver because it is the technically easiest to learn [5, 17]. During Valsalva maneuver, if the patient has normal VCs, one could see both VCs adducting symmetrically to the midline (see Video 31.1). On the other hand, when a patient suffers from a unilateral VCP , one would see either reduced (Video 31.2) or completely absent movement (Video 31.3) on the affected side (i.e., asymmetrical movement). Other maneuvers such as active phonation at times may induce movement in other laryngeal muscles and therefore not prefer. The other trick one could also try to induce voluntary movement of VCs is to ask the patient to swallow his or her own saliva for a few times.
31.4 Factors Leading to Non-visualization of VCs
Since visualization of the VCs really depends on whether the USG waves could travel from the skin to the VCs and the landmarks via the thyroid cartilage, the presence of ossification in the thyroid cartilage is the major reason for unclear VC visualization. There is little controversy that patients with ossified thyroid cartilage are not good candidates for TLUSG . Ossification itself blocks the propagation of USG waves onto the VCs and therefore, on imaging, one could see that there is a large acoustic shallow over the VCs and arytenoids making evaluation of VCs impossible (Fig. 31.2). Nevertheless, there are patient factors that could help to predict the presence of ossification. First is age. It has been well demonstrated that the extent of ossification gradually increases with age. This is compatible with our and others’ experience that it is much easier to image VCs in young patients [12–15]. In fact, a previous study found that almost 100 % of patients aged <30 years old had clear VC visualization while this rate dropped to <90 % in patients aged >70 years old [15]. A recent anatomical study of 200 healthy individuals of all ages have shown that this ossification process begins at the age of 18–20 years in the posterior part of the thyroid cartilage regardless of sex and over time, the ossification process slowly moves in an anteromedial direction until the entire cartilage has been completely replaced by bone (i.e., ossified) [18]. In this study, the authors found that the thyroid cartilage is not consistently denser (as measured by Hounsfield units) on CT scan until after the age 40 [18]. Consistent with this, some studies have reported that the entire cartilage only becomes replaced by bone by age of 65 [19]. Fortunately, this process appears to be less complete in females and therefore, some females may still have a small non-ossified ventral window in their thyroid cartilage making TLUSG possible [20]. Partly because of this difference in ossification between the two sexes, male patients generally have significantly lower rate of VC visualization than female patients. By adjusting for other significant clinical variables, one study found male patients to be 13 times more likely to have non-visualized VCs than females [15]. The other reason for this gender difference might be due to the thickness of the thyroid cartilage as males tend to have thicker and larger thyroid cartilage than females leading to poorer propagation of USG waves.
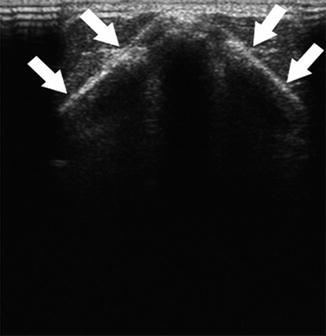
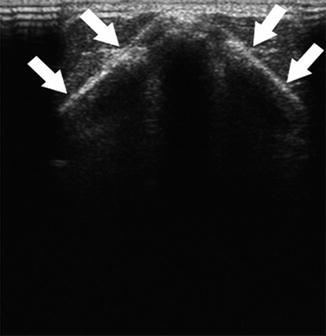
Fig. 31.2
This is an image depicting the presence of ossification at both lamina of the thyroid cartilage. Please also note the large post-acoustic shallow posterior to the cartilage
In addition to age and sex, patient height and the placement of neck incision in relation to the cricoid cartilage have also been found to be independent factors for non-visualization of VCs in postoperative TLUSG . For patient height, it was shown that even after adjusting for sex and age, those who were taller were significantly less likely to have non-visualized VCs on TLUSG than those who were shorter in height. Using a median cutoff of 158 cm, the non-visualization rate for patients taller than 158 cm was significantly higher than those shorter than 158 cm (9.0 % vs. 1.0 %, p < 0.001). Similarly, using a median distance of 60 mm from skin incision to the cricoid cartilage, those with distance less than 60 mm were significantly more likely to have non-visualized VCs than those with distance ≥60 mm (6.9 % vs. 3.9 %, p = 0.050) [15]. The reason why the distance between wound and cricoid cartilage is an independent factor for non-visualization is probably related to the presence of subplatysmal swelling or edema after thyroidectomy. Therefore, it may still be possible to visualize the VCs in patients with short distance between wound and cricoid cartilage provided that a longer waiting period is allowed for the resolution of swelling and edema.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree