Fig. 34.1
Positioning: The neck hyperextended after potential sites for the incision were mapped in the preoperative holding area
34.2 Thyroid
Surgeons often review cervical ultrasonography results, whether performed by the surgeon themselves or by another provider, prior to an operation. However, useful information can be obtained when the surgeon repeats the ultrasound in the operating room for several reasons. The surgeon can re-familiarize herself or himself with the unique anatomy of the patient’s gland including size, location of the poles and isthmus, and involvement of adjacent structures such as the trachea, esophagus, or strap muscles. In addition, the surgeon can assess the gland’s firmness and vascularity, which is helpful when operating on patients with Graves’ disease or Hashimoto’s thyroiditis . Moreover, ultrasound has high sensitivity for identifying vascular anomalies associated with a nonrecurrent laryngeal nerve, such as an aberrant right subclavian artery [5]. Re-familiarization with the anatomy is useful for shaping intraoperative expectations and tailoring the operative approach .
Furthermore, the surgeon may detect new findings when repeating the ultrasound in the operating room. With the patient’s neck hyperextended, the central neck is better visualized, enhancing the detection of enlarged lymph nodes. Additionally, if there has been a significant time interval between the preoperative ultrasound to the operation or if there is particularly aggressive malignant behavior, the ultrasound may demonstrate advancement of disease. Lastly, the ultrasound findings can influence where and how large to make the incision. Ideally, the incision is centered over the gland and/or isthmus, is appropriately sized to access all poles, and is placed in a natural skin crease. The surgeon can mark all natural skin creases in the preoperative holding area with the patient sitting upright and awake (Fig. 34.2), and once the patient is under anesthesia and the neck is extended, the ultrasound is used to identify which crease will be most favorable given the patient’s unique gland anatomy (Fig. 34.3).



Fig. 34.2
Incisional mapping : The patient’s natural skin creases are marked in the preoperative holding area

Fig. 34.3
Individualized incision-making: (a) The choice of incision location is influenced by intraoperative ultrasound , which reveals each patient’s unique anatomy. The incision that grants adequate access and also enhances the cosmetic result is used. (b) The appearance of the incision after closure
34.3 Parathyroid
Surgeon-performed ultrasound is a highly sensitive preoperative localization study for patients with primary hyperparathyroidism [6]. Occasionally, repeating the ultrasound in the operating room after the patient has been optimally positioned can identify parathyroid adenomas that were not visible in the office (Fig. 34.4). The necessary amount of pressure with the transducer can be obtained because the patient has received anesthetics. Applying pressure with the transducer on the neck can distinguish the relationship of parathyroid adenomas to the thyroid, elucidating the likely embryologic origin of the gland and producing real-time information to target the dissection. Similar to IOUS of the thyroid, repeating the exam can re-familiarize the surgeon with the patient’s unique anatomy to identifying the relationship of enlarged parathyroid adenomas to the thyroid gland, tubercle of Zuckerkandl, vasculature, thymus, and sternothyroid muscle. In the event that no abnormal parathyroid gland is found during exploration, IOUS can be performed to scrutinize the remainder of the neck, especially regions historically known to harbor ectopic glands. For example, IOUS can reidentify thyroid nodules and their laterality, prompting the consideration of an intrathyroidal parathyroid adenoma if the intraoperative findings warrant this possibility (Fig. 34.5).



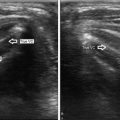
Fig. 34.4
Parathyroid adenoma identified on intraoperative ultrasound: (a) During ultrasound in the office setting, no parathyroid adenomas were identified in the neck. The subsequent nuclear medicine imaging (not shown) was also negative. (b) In the operating room, the patient received anesthetics and the neck was hyperextended. After gentle pressure with the transducer, a parathyroid adenoma was identified posterior to the right thyroid lobe

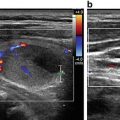
Fig. 34.5
Intrathyroidal parathyroid adenoma : During parathyroid exploration, the operative findings and intraoperative PTH levels indicated persistent disease. A hypoechoic lesion in the right thyroid lobe was identified during ultrasound. A right thyroid lobectomy was performed, which resulted in an appropriate decline of the intraoperative PTH level. Frozen section examination and final pathology confirmed intrathyroidal parathyroid adenoma
Perhaps the most valuable use of IOUS for parathyroid operations is in setting of a previous neck operation, referred to as reoperative parathyroidectomy . Reoperative parathyroidectomy is a challenging clinical scenario, and many surgeons require more than one preoperative localizing study to plan parathyroidectomy . Cervical ultrasound is 55–69 % successful in identifying the offensive gland in patients with persistent or recurrent disease [7, 8]. If the patient’s offending gland was identified on preoperative ultrasound, repeating the ultrasound in the operating room can facilitate targeted dissection in the scarred, reoperative field.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree