Chapter 10 Miscellaneous
Scott Stevens, Halemane Ganesh, and Adrian Dawkins
10 Questions and Answers
Question 10.1: This sonographic image below demonstrates a color Doppler overlay in the region of the main portal vein. What accounts for the incomplete color fill-in?

A. Nonocclusive thrombus.
B. Incorrect color priority setting.
C. Color box set too wide.
D. Color scale set too high.
Answer:
D. Correct. The color scale is set to +/-77 cm/second. When the color scale is set to this high value, there is also an unavoidable increase in the wall filter. This results in obscuration of low-velocity flow, hence the incomplete portal venous color fill-in.
A. Incorrect. The incomplete color fill-in is artifactual.
B. Incorrect. The color priority setting affects which shades of gray can be replaced by color, since the display has to choose between the grayscale and color. The color priority bar is seen as the progressively darkening band adjacent to the color bar. In this example, the color priority is set high (green line at top of band), therefore optimized for the detection of flow.
C. Incorrect. The color box should be positioned tightly around the structure being interrogated. In this example, there is perhaps opportunity to decrease the width; however, this measure would not improve the color fill-in.
Question 10.2: With reference to the image below, which statement is correct?

The angle correction is poorly aligned resulting in an inaccurate resistive index measurement.
The lack of any “blue” areas within the renal parenchyma suggests occlusion of the renal vein.
The resistive index is being measured incorrectly.
The beam is focused incorrectly.
Answer:
C. Correct. The resistive index is obtained by dividing the difference of the peak systolic velocity (PSV) and end diastolic velocity (EDV) by the PSV, that is, (PSV − EDV)/PSV. In this example, the second caliper is not positioned at the EDV, since the EDV occurs just before the sharp systolic upstroke. In the case presented, the error is perhaps not significant since the second half of the cycle is fairly flat. However, this is not always the case and significantly erroneous measurements could be obtained.
A. Incorrect. The resistive index measurement is not dependent on angle correction, since both the PSV and EDV will be affected by the same factor, cancelling out during calculation.
B. Incorrect. The color bar displays graded shades of pink, a frequent color assignment for power Doppler. Power Doppler typically yields no directional information but is very useful at demonstrating areas of slow flow. Consequently, when using this display setting, there will be no “blue” areas to indicate flow in the opposite direction.
D. Incorrect. The ultrasound beam is focused appropriately at the level of the renal parenchyma as illustrated by the focus position bar (yellow star).
Question 10.3: Regarding this image, which statement is correct?

The findings are within normal limits.
Aliasing within the transjugular intrahepatic portosystemic shunt (TIPSS) is suggestive of malfunction.
The direction of flow within the left branch of the portal vein (yellow arrow) is suggestive of malfunction.
None of the above.
Answer:
A. Correct. The color scale (+/− 18.5 cm/second) has been optimized to demonstrate flow within the portal vein. However, as a result of this relatively low scale, there is commensurate aliasing within the TIPSS because of the normal higher velocities within the TIPSS (90–190 cm/second). Reversal of flow with the left branch of the portal vein is a sign of a proper functioning TIPSS.
B. Incorrect. Aliasing occurs because of the normal higher velocities within the TIPSS.
C. Incorrect. Reversal of flow within the left branch of the portal vein is a sign of a proper functioning TIPSS.
D. Incorrect.
Question 10.4: This 67-year-old patient presents with abdominal pain and undergoes an abdominal ultrasound. The patient’s symptoms are likely worsened by which factor?

Fasting.
Expiration.
Erect posture.
None of the above.
Answer:
B. Correct. The image demonstrates the celiac axis ( yellow arrow) and superior mesenteric artery (green arrow) in the longitudinal plane, as they originate from the aorta (star). At grayscale, the celiac axis origin is seen to be severely narrowed. The color Doppler overlay reveals aliasing in this region. These findings are consistent with median arcuate ligament syndrome (MALS). This condition is exacerbated by in expiration.
A. Incorrect. The symptoms experienced in MALS are worsening by eating.
C. Incorrect. MALS is exacerbated by lying supine but somewhat alleviated by an erect posture.
D. Incorrect.
Question 10.5: A 58-year-old male patient presents with elevated liver function tests. He was the recipient of a transplanted liver. What is suggested by this duplex evaluation at the porta hepatis.

Hepatic artery stenosis.
Hepatic arterial occlusion.
Aneurysmal portal vein.
Reversed portal venous flow.
Answer:
A. Correct. The image reveals spectral Doppler evaluation of the hepatic artery. The obtained waveform reveals a prolonged acceleration time and decreased overall peak velocity resulting in the classic “parvus tardus” waveform. This is usually the result of proximal stenosis.
B. Incorrect. The hepatic artery is seen to be patent.
C. Incorrect. The portal vein is normal in caliber.
D. Incorrect. The directionality of the portal vein cannot be definitely inferred since the directionality color bar has been cropped (though the flow is known to be antegrade by the author). However, reversed portal venous flow in the setting of a liver transplant is very uncommon, often with a poor outcome.
Question 10.6: Which of the following is a complication that is associated with hepatic artery stenosis in a transplanted liver?
Portal hypertension.
Biliary necrosis.
Thromboembolic disease.
Splenic vein occlusion.
Answer:
B. Correct. In the setting of a liver transplant, the integrity of the biliary tree is dependent on the hepatic arterial circulation. If hepatic arterial stenosis is sufficiently severe, it may lead to biliary necrosis.
A. Incorrect. Portal hypertension is not directly associated with hepatic artery stenosis.
C. Incorrect. Thromboembolic disease is not directly associated with hepatic artery stenosis.
D. Incorrect. Splenic vein occlusion is not directly associated with hepatic artery stenosis.
Question 10.7: A 54-year-old male presents with repeated episodes of hematemesis and hematochezia. An ultrasound of the upper abdomen is performed, an image from which is presented below. How should the patient be definitively managed?

Splenectomy.
Thrombectomy.
Thrombolysis.
Placement of TIPSS.
Answer:
A. Correct. The image demonstrates incomplete color fill-in of the splenic vein consistent with splenic vein thrombosis (SVT). SVT is occasionally complicated by upper gastrointestinal bleeding secondary to esophageal varices. This is usually treated definitively with splenectomy, effectively removing the problematic collateral pathway.
B. Incorrect. Thrombectomy is at best a temporizing measure.
C. Incorrect. Thrombolysis is at best a temporizing measure.
D. Incorrect. A TIPSS may be undertaken in patients with intractable upper gastrointestinal bleeding. However, extensive SVT, possibly extending to the portal vein often renders a TIPSS ineffective.
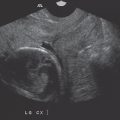
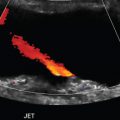
Question 10.8: What finding is depicted?

Cavernous transformation of the portal vein.
Aneurysmal portal vein.
Arteriovenous shunt.
Budd–Chiari syndrome.
Answer:
A. Correct. The images demonstrate occlusion of the main portal vein with multiple surrounding small collateral vessels. These finding represent cavernous transformation of the portal vein usually the result of longstanding portal hypertension.
B. Incorrect. An aneurysmal portal vein is not imaged.
C. Incorrect. Arterioportal shunts are usually observed as intrahepatic nodular enhancing foci on cross-sectional imaging.
D. Incorrect. Budd–Chiari syndrome usually manifests as marked enlargement of the caudate lobe and nonvisualization of the hepatic veins.
Question 10.9: The complex fluid collection superior to this transplanted kidney (arrow) was proven to be a hematoma. What other clinically pertinent finding is present?

Borderline elevated resistive index.
Absence of renal venous flow.
Concerning physiologic response.
Increased PSV of parenchymal vessels.
Answer:
C. Correct. The image demonstrates marked tachy-cardia, calculated by counting the peaks within the time scale outlined at the bottom of the image. The time scale indicates roughly 6 seconds, within which there are approximately 14 peaks. Consequently, the heart rate is about 140 beats/minute. Observing the pattern of the spectral tracing can often reveal clinically useful information such as arrhythmias.
A. Incorrect. The resistive index (0.74) is within normal limits.
B. Incorrect. Absent renal venous flow would manifest as reversed arterial diastolic flow.
D. Incorrect. PSV should be interpreted with caution since reliable angle correction is challenging when evaluating very small vessels.
Question 10.10: A 46-year-old male is to be discharged 2 days post TIPSS placement for refractory ascites. The clinical service requests an ultrasound study to confirm TIPSS patency prior to discharge. A representative image from this study is demonstrated below. Based on the appearances, which management strategy is correct.

Repeat angiography to confirm patency, even if there are no clinical signs of TIPSS occlusion.
Initiate thrombolytic therapy.
Repeat ultrasound in 1 week.
None of the above.
Answer:
C. Correct. Soon after the deployment of some TIPSS devices, in particular covered stents, air may become trapped within the expanding wall, rendering evaluation of patency invalid. One key clue to artifactual occlusion is the inability to visualize the far wall of the device, as in this case. It typically takes 1 week for the gas to dissipate so, unless there is a clinical concern regarding patency, some shunts are best evaluated at least 1 week post placement.
A. Incorrect. This measure would be unnecessary.
B. Incorrect. This measure would be unnecessary and inappropriate.
D. Incorrect.
Question 10.11: Regarding carotid ultrasound, the sonographic maneuver annotated TT below is most often used to identify which vessel?

Internal carotid artery (ICA).
External carotid artery (ECA).
Common carotid artery (CCA).
Vertebral artery (VA).
Answer:
B. Correct. TT refers to “temporal tap” as is obtained by tapping over the superficial temporal artery while interrogating the ECA. This transmitted thrill can be seen as a saw-tooth appearance. This helps to confirm that the ECA is being evaluated as opposed to the closely related ICA since the superficial temporal artery is a branch of the ECA.
A, C, D—Incorrect. The temporal tap maneuver is used to identify the ECA.
Question 10.12: Regarding carotid ultrasound, which of the imaging parameters below is most often the best for grading the severity of cervical carotid stenoses?
PSV in the ICA.
EDV in the ICA.
PSV in the CCA.
ICA/CCA PSV ratio.
Answer:
A. Correct. Primary parameters for estimating the degree of stenosis include the PSV and visible plaque.
B, C—Incorrect. These measures are not useful for estimating stenosis.
D. Incorrect. The ICA/CCA PSV ratio is a secondary parameter but may be of value when overall carotid velocities are elevated, say in hypertension.
Question 10.13: A 71-year-old diabetic male presents with right foot pain. An ultrasound is performed as shown. What finding is highly suggestive of distal occlusion?

Incomplete color fill-in.
Spectral broadening.
Aliasing.
Loss of the majority of diastolic flow.
Answer:
D. Correct. A normal popliteal artery would demonstrate vascular flow throughout the cardiac cycle, often creating a triphasic waveform. In this case, the peak velocity is marginally diminished and there is loss of the majority of diastolic flow. This has been described as the preocclusive “thump” or “staccato” waveform indicating a distal occlusion.
A. Incorrect. Incomplete color fill-in suggests thrombus at the site of interrogation.
B. Incorrect. Spectral broadening (filling in of the spectral curve) is also suggestive of stenosis at the site of interrogation.
C. Incorrect. Aliasing may be encountered within stenotic segments of vessels due to increased velocity. However, aliasing does not necessarily indicate a distal occlusion.
Question 10.14: This image is obtained from a patient with Gaucher’s disease. Which statement is correct?

Splenomegaly is an uncommon manifestation.
When hyperechoic lesions are present within the spleen, splenectomy is recommended.
Thrombocytopenia is a complication of this condition.
Splenic lesions in the setting of Gaucher’s disease are highly suggestive of lymphoma.
Answer:
C. Correct. Gaucher’s disease is a lysosomal storage disorder resulting in the accumulation of glucocerebroside within lysosomes of mononuclear phagocytes. This typically affects the bone marrow, liver, and spleen. The spleen is typically enlarged and may demonstrate several focal lesions which may be hypo- or hyperechoic on ultrasound. “Gaucheromas” may also be present within the liver. These lesions demonstrate no known malignant potential and, though of indeterminate etiology, may result from a combination of infarction, extramedullary hematopoiesis, and fibrosis. Thrombocytopenia is known complication of Gaucher’s disease.
A. Incorrect. Splenomegaly is typically present.
B. Incorrect. This would be an unnecessary measure.
D. Incorrect. These lesions are unlikely to represent lymphoma.
Question 10.15: Sonographic images of the spleen were obtained in an 8-year-old patient with bruising. What is the likely diagnosis?

Hemangioma.
Angiosarcoma.
Hamartoma.
Lymphangioma.
Answer:
A. Correct. The images represent a path-proven large splenic hemangioma. Large hemangiomas have a propensity to bleed. Also, there may be associated consumptive coagulopathy predisposing the patient to bleeds, for example, Kasabach–Merritt syndrome.
B. Incorrect. Splenic angiosarcomas are exceedingly rare and tend to occur in the middle-aged individuals. Ultrasound appearances are nonspecific.
C. Incorrect. Splenic hamartomas are uncommon lesions that tend to be hyperechoic with respect to the background splenic parenchyma. Bruising is not typically associated with splenic hamartomas.
D. Incorrect. Splenic lymphangiomas tend to occur in children but are typically cystic in morphology.
Question 10.16: The splenic lesion imaged below is consistent with which of the following?

An infarct.
An abscess.
A granuloma.
A metastatic deposit.
Answer 10.16:
A. Correct. The image demonstrates a wedge-shaped somewhat reticulated area of hypoechogenicity within the splenic parenchyma. This finding is typical of a splenic infarct.
B. Incorrect. Infarcts may progress to abscess formation. However, an abscess typically manifests as a complex fluid collection with surrounding hyperemia.
C. Incorrect. A granuloma typically presents as a punctate echogenic focus consistent with calcification. They are often multiple.
D. Incorrect. Splenic metastases are relatively uncommon but would typically present as a hypoechoic rounded lesion.
Question 10.17: What is the likely cause for this appearance in this 17-year-old African American patient with abdominal pain and anemia?

Splenic sequestration.
Echinococcal disease.
Splenic abscess.
Gamna–Gandy bodies.
Answer 10.17:
A. Correct. This patient has a history of sickle cell anemia. The spleen is larger than expected for age, since 94% of HbSS patients are “asplenic” by the age of 5 years. The heterogenous appearance of the splenic parenchyma is typical of splenic sequestration, the result of trapping of red blood cells within the spleen. Early recognition of the finding is vital to limit adverse outcomes.
B. Incorrect. Echinococcal disease of the spleen usually results in the formation of “hydatid cysts” which may vary from solitary cysts to a dominant cystic lesion with contained daughter cysts.
C. Incorrect. An abscess would manifest as a complex fluid collection with surrounding hyperemia. Gas may also be contained.
D. Incorrect. Gamna–Gandy bodies represent foci of microhemorrhage within the spleen and usually signify portal hypertension. These lesions are usually diagnosed on in-and-out of phase T1-weighted magnetic resonance images. Sonographically these lesions are frequently occult. Occasionally, Gamna–Gandy bodies are seen as punctate echogenic foci throughout the spleen, with or without acoustic shadowing.
Question 10.18: A patient presents with a history of recurrent abdominal pain. An ultrasound is undertaken. The width of which structure is being measured?

Pancreatic duct.
Left renal vein.
Splenic vein.
Common bile duct.
Answer:
A. Correct. The image demonstrates a tubular structure with numerous associated echogenic foci. This tubular structure is anterior to the splenic vein (star). The findings are consistent with a dilated pancreatic duct.
B. Incorrect. The left renal vein runs between the superior mesenteric artery (yellow arrow) and the aorta (blue arrow). It is not imaged.
C. Incorrect. The splenic vein is indicated by the star.
D. Incorrect. The distal portion of the common bile duct may be visualized as it traverses the pancreatic head. It is not imaged.
Question 10.19: What is the likely diagnosis of the patient in (Question 10.18)?
Splenorenal shunt.
Chronic pancreatitis.
Nonocclusive thrombosis of the splenic vein.
Choledocholithiasis.
Answer:
B. Correct. The combination of a dilated pancreatic duct and numerous parenchymal and ductal punctate calcifications are consistent with changes of chronic pancreatitis.
A. Incorrect. A splenorenal shunt is frequently encountered in portal hypertension, allowing blood to return to the right heart via the left renal vein and inferior vena cava, bypassing the portal circulation. Such a shunt is not imaged.
C. Incorrect. The splenic vein is patent.
D. Incorrect. The common bile duct is not imaged.
Question 10.20: A 36-year-old female presents with abdominal pain. The structure labeled “a” is?

Consistent with focal acute pancreatitis.
Consistent with a pancreatic neoplasm.
A peripancreatic lymph node.
A normal variant.
Answer:
D. Correct. The image demonstrates a well-defined area of relative hypoechogenicity involving the ventral pancreas. This is a normal variant due to relatively less fat content within the ventral pancreas as compared to the remaining pancreatic parenchyma.
A. Incorrect. The pancreas is often sonographically normal in the seating of generalized or focal pancreatitis.
B. Incorrect. A pancreatic neoplasm may be seen as a distinct mass within the pancreas, often with pancreatic ductal dilation.
C. Incorrect. A lymph node would be seen as a separate oval-shaped structure.
Question 10.21: A 36-year-old female presents with a history of abdominal pain. A longitudinal sonographic view of the upper abdomen is presented below. What is the likely underlying cause for finding indicated by the arrow ?

Serous cystadenoma.
Solid pseudopapillary epithelial neoplasm (SPEN).
Acute necrotic collection.
Walled-off necrosis.
Answer:
B. Correct. The arrow indicates a mixed solid and cystic lesion in the expected location of the pancreatic head. Of the choices provided, a SPEN is the most likely diagnosis, typically occurring in young female adults (third decade of life). This benign lesion is frequently noted to be solid with cystic areas.
A. Incorrect. A serous cystadenoma also demonstrates a female predilection, though in an older demographic. Also, these lesions are typically more cystic in morphology than demonstrated in this case.
C. Incorrect. An acute necrotic collection occurs as a complication of acute pancreatitis. This lesion would be predominantly cystic, unlike this case.
D. Incorrect. Walled-off necrosis occurs as a complication of acute pancreatitis. As above, this lesion would be predominantly cystic, unlike this case.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree